Mindfully Effective: Evidence-Based Occupational Therapy for Mental Health

Why Evidence-Based Practice in Mental Health OT Matters Now
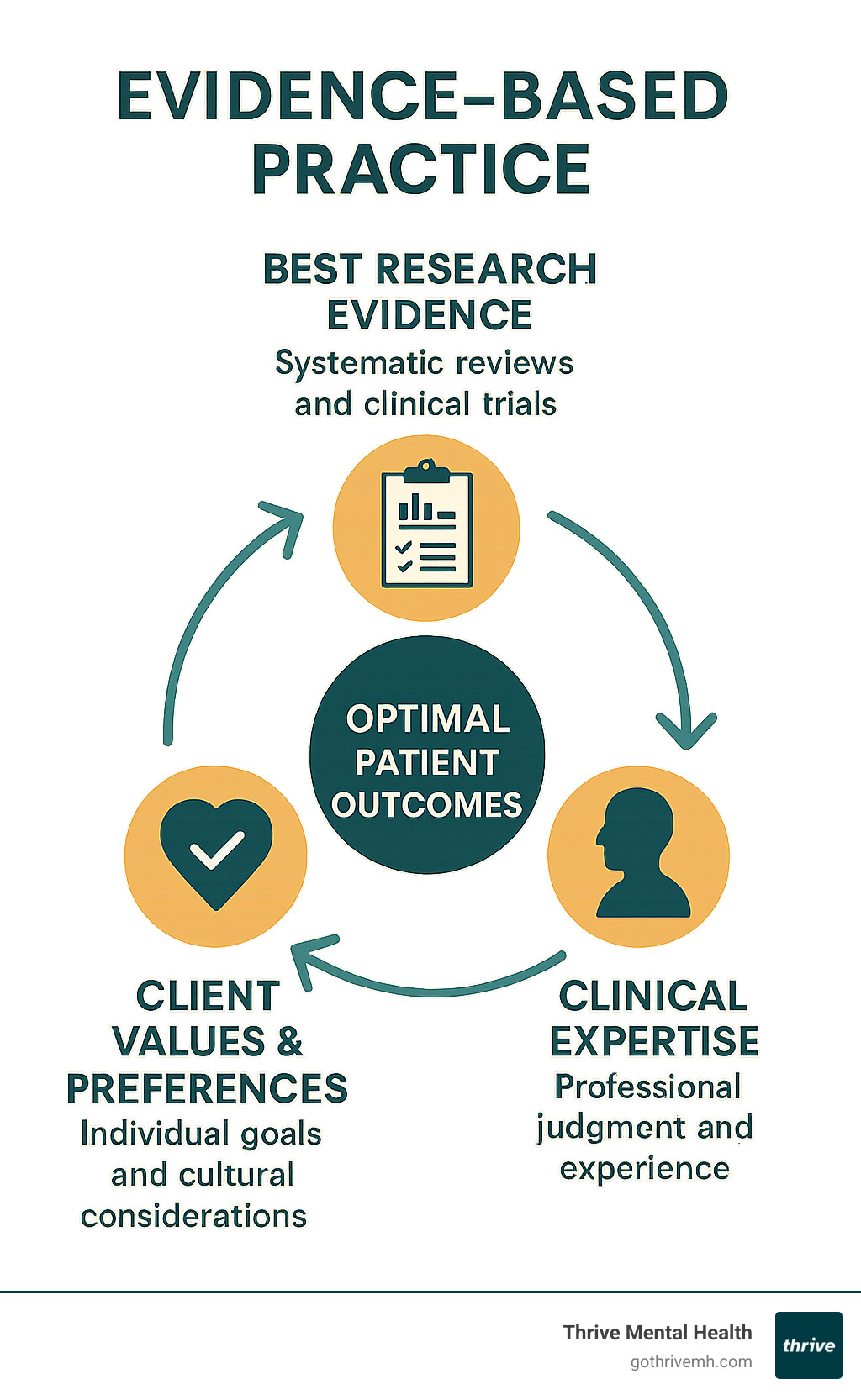
Evidence based practice occupational therapy mental health represents the gold standard for delivering effective, accountable care to individuals struggling with mental health challenges. This approach combines the best research evidence with clinical expertise and client preferences to create personalized treatment plans that actually work.
Quick Answer: Evidence-Based Practice in Mental Health OT includes:
- Best Research Evidence: Systematic reviews, clinical trials, and practice guidelines
- Clinical Expertise: Therapist’s professional judgment and experience
- Client Values: Individual preferences, goals, and cultural considerations
- Proven Interventions: CBT, DBT, trauma-informed care, social skills training
- Measurable Outcomes: Improved function, reduced symptoms, better quality of life
The numbers tell a compelling story. 97% of occupational therapists agree that evidence-based practice is necessary, while 92% say it helps with clinical decision-making. Yet despite this overwhelming support, many practitioners struggle to consistently implement EBP in their daily practice.
This challenge is particularly acute in mental health settings, where the complexity of human experience meets the need for systematic, research-backed interventions. The stakes are high – mental health conditions affect 1 in 8 people globally, with treatment gaps ranging from 53% to 79% for moderate to severe disorders.
As CEO of Thrive Mental Health, I’ve witnessed how evidence based practice occupational therapy mental health transforms lives when implemented effectively within our flexible, client-centered programs in Florida. My experience scaling behavioral health companies has shown me that the most successful outcomes happen when rigorous evidence meets compassionate, individualized care.
What is Evidence-Based Practice (EBP) in Occupational Therapy?
Think of evidence based practice occupational therapy mental health as your treatment team’s North Star – it’s the guiding principle that ensures every decision about your care is grounded in science, expertise, and your unique needs.
At Thrive Mental Health, we define Evidence-Based Practice (EBP) using the framework that has transformed healthcare globally. EBP is ‘the conscientious, explicit and judicious use of the best evidence in making decisions about the care of the individual patient’ according to this paper.
What does this mean for you? Simply put, we don’t guess when it comes to your mental health. Instead of relying on outdated methods or personal hunches, we actively seek out and apply the latest research findings to create your personalized treatment plan.
The three core components work together like legs of a sturdy stool, each one essential for effective clinical decision-making:
Best Research Evidence forms our scientific foundation. We dive deep into high-quality studies, systematic reviews, and clinical practice guidelines to understand what actually works for conditions like depression, anxiety, and trauma. This isn’t about cherry-picking studies that support what we want to believe – it’s about the conscientious and judicious use of evidence from trusted sources like the Cochrane Library.
Clinical Expertise brings the human element to the equation. Our seasoned therapists contribute years of professional judgment, clinical reasoning, and real-world experience. They know how to read between the lines of research studies and adapt proven interventions to fit your specific situation. This expertise allows us to bridge the gap between what works in controlled studies and what works in your daily life.
Client Values and Preferences – that’s where you come in as the most important member of your treatment team. Your cultural background, personal beliefs, life goals, and what matters most to you shape every aspect of your care. We use collaborative approaches to ensure your voice guides the entire process, because the most effective intervention is one that truly resonates with who you are.
This approach is sometimes called evidence-informed practice to emphasize how these three elements work together dynamically rather than following a rigid formula. Regardless of the terminology, this represents the gold standard of care in modern mental health treatment.
When we combine rigorous research with clinical wisdom and your personal insights, something powerful happens – treatment that’s not just effective, but meaningful and sustainable for your unique journey toward mental wellness.
The “Why”: The Critical Importance of EBP in Mental Health OT

When I talk with families about why evidence based practice occupational therapy mental health matters so much, I often see a mix of hope and skepticism in their eyes. They’ve tried different approaches before, and they want to know: “Will this actually work?”
That’s exactly the right question to ask. And it’s precisely why evidence-based practice isn’t just an academic concept – it’s the foundation of everything we do at Thrive Mental Health.
Improved client outcomes are the heart of why EBP matters. When we use interventions backed by solid research, we see real changes in people’s lives. I’m talking about tangible improvements: better sleep, stronger relationships, the ability to return to work, or simply feeling hopeful again. Research consistently demonstrates that EBP produces better outcomes in a more cost-effective way compared to treatments that aren’t grounded in evidence.
This isn’t just about feeling better temporarily – it’s about lasting change that transforms how you engage with the world around you.
From a practical standpoint, cost-effectiveness benefits everyone involved. When we use proven methods, we’re not wasting time on approaches that sound good but don’t deliver results. This means you spend less time in treatment and more time living your life. It also means healthcare resources go further, helping more people access the care they need.
Professional accountability is something we take seriously. When 97% of occupational therapists agree that EBP is necessary, we’re not just following a trend – we’re upholding a professional standard. This commitment aligns with the AOTA Vision 2025, which envisions occupational therapy as a science-driven, evidence-based profession that people can trust.
The reality of today’s healthcare system also makes EBP essential for insurance reimbursement. With value-based payment initiatives becoming the norm, insurance companies want to see proof that treatments actually work. When we can show clear evidence supporting our interventions, it helps ensure you can access the care you need without unnecessary barriers.
At Thrive Mental Health, our programs are built on a solid foundation of evidence-based practice. We’ve seen how this approach transforms lives.
Our flexible Intensive Outpatient Program (IOP) and Partial Hospitalization Program (PHP) serve clients across Florida, including Miami-Dade, Broward, Palm Beach, Hillsborough, Orange, and Duval counties. These aren’t just convenient options; they’re effective because they’re rooted in what research proves works for mental health recovery.
Evidence-Based Practice Occupational Therapy Mental Health in Action: Key Interventions
When you walk into one of our therapy sessions at Thrive Mental Health, you might wonder what evidence based practice occupational therapy mental health actually looks like in real life. The truth is, it’s not about rigid protocols or cookie-cutter approaches. Instead, it’s a rich, dynamic toolkit that our occupational therapists draw from to help you steer mental health challenges and refind meaningful participation in your daily life.
Think of it this way: every intervention we use has been tested, studied, and proven effective through rigorous research. But here’s where the magic happens – we take that solid foundation of evidence and carefully adapt it to fit your unique story, goals, and circumstances.
Cognitive Behavioral Therapy (CBT) principles form a cornerstone of our approach, though you might be surprised to learn how occupational therapists weave these concepts into daily life skills. Rather than just talking about thought patterns, we help you recognize how your thoughts directly impact your ability to get dressed in the morning, maintain your job, or enjoy time with friends. In our psychoeducational groups, you’ll find practical ways to cope with anxiety or depression that go far beyond the therapy room – techniques you can use while grocery shopping or preparing for a work presentation.
For those dealing with intense emotions, Dialectical Behavior Therapy (DBT) principles become invaluable tools. Our therapists integrate DBT skills training into real-world situations, helping you practice emotional regulation while engaging in meaningful activities. Maybe you’re learning distress tolerance techniques while working on a pottery project, or developing interpersonal effectiveness skills during group cooking sessions.
Acceptance and Commitment Therapy (ACT) principles offer another powerful approach, especially when you’re struggling to find direction. ACT helps you develop psychological flexibility – the ability to stay present with difficult feelings while still moving toward what matters most to you. Our occupational therapists excel at helping you identify those important occupations and values, then creating concrete steps to re-engage with them.
Social skills training addresses one of the most common challenges in mental health recovery: reconnecting with others. Mental health conditions often leave people feeling isolated or uncertain in social situations. Our group-based interventions provide a safe, supportive environment where you can practice communication skills, learn to read social cues, and build confidence in relationships. The beauty of this approach is that you’re not just talking about social skills – you’re actively using them in real time with peers who understand your journey.
For many of our clients, returning to work or school represents a major milestone in recovery. Supported employment and education interventions, particularly the Individual Placement and Support (IPS) model, have strong research backing for helping individuals with serious mental illness achieve their vocational goals. Our occupational therapists assess your unique strengths and interests, then provide targeted support – whether that’s job coaching, developing workplace social skills, or even practical assistance with professional grooming and attire.
Psychoeducational groups serve as knowledge-building foundations, covering everything from understanding your diagnosis to mastering daily living skills. But these aren’t dry, lecture-style sessions. Instead, they’re interactive experiences where you gain practical strategies for symptom management while connecting with others who share similar challenges.
At the heart of occupational therapy lies activity-based and occupation-based interventions – using meaningful activities as healing tools. This might involve nature-based activities like hiking, creative pursuits such as pottery or artwork, sports, or even gardening. The Tree Theme Method (TTM) helps individuals with depression or anxiety explore their life story through daily activities, fostering deep, reflective dialogue. The Grocery Shopping Skill Program (GSSP) improves executive function and daily living skills for patients with schizophrenia. These specialized interventions often prove more effective than conventional approaches because they’re rooted in activities that already hold meaning for you.
Trauma-informed care underpins everything we do, recognizing that trauma’s impact extends far beyond the initial experience. Our occupational therapists create safe, trustworthy environments where you feel respected and empowered throughout your healing journey. This approach shapes how we build therapeutic relationships and collaborate with you, always building upon your existing strengths and coping strategies.
Daily living skills training might sound basic, but it’s often the foundation that makes everything else possible. Our therapists help you plan, initiate, and track both short-term and long-term goals for daily life participation. This includes practical strategies for managing mental illness effects, structuring your days for better balance, and even addressing basic self-care needs when depression or anxiety makes these tasks feel overwhelming. One client struggling with abstract thinking found success through visual reminders and checklists – simple tools that transformed their daily routine.
The effectiveness of these interventions continues to evolve through ongoing research. Comprehensive reviews, including studies on occupational therapy for mental health conditions and substance use disorders, demonstrate significant improvements in reducing symptoms of depression and anxiety, enhancing social functioning, improving cognitive performance, and reducing rehospitalization rates for conditions like schizophrenia.
While research gaps still exist – particularly around cost-effectiveness and specific evidence for conditions like bipolar disorder or PTSD – we remain committed to using the best available evidence while contributing to the growing body of knowledge in our field. This commitment to continuous learning and improvement is what makes evidence based practice occupational therapy mental health so powerful and why it forms the foundation of our flexible, evidence-based programs here in Florida.
Overcoming Problems: Challenges in Implementing EBP

Let’s be honest – implementing evidence based practice occupational therapy mental health sounds great on paper, but the reality of daily clinical practice can feel like trying to fold a fitted sheet while riding a bicycle. Even the most dedicated therapists face real, practical challenges that can make consistent EBP implementation feel overwhelming.
Time constraints top the list of barriers our therapists encounter. Picture this: you’re juggling a heavy caseload, completing documentation, attending team meetings, and providing direct client care. When exactly are you supposed to find time for thorough literature searches and critically appraising research studies? It’s like trying to squeeze an extra hour into a 24-hour day – theoretically possible, practically challenging.
The struggle becomes even more pronounced when there’s a lack of organizational support. For EBP to truly thrive, therapists need access to research databases, protected time for professional development, and leadership that champions evidence-based culture. Without these foundational supports, even the most enthusiastic practitioner can feel like they’re swimming upstream against a strong current.
Heavy caseloads compound these challenges significantly. When you’re seeing client after client with complex mental health needs, the immediate demands of providing care can overshadow the longer-term investment in staying current with research. It’s a classic case of urgent tasks crowding out important ones.
Another significant hurdle involves practitioner habits and the natural human tendency to resist change. We’re all creatures of habit, and healthcare professionals are no exception. Sometimes therapists develop strong preferences for methods they’ve used successfully in the past, or they rely heavily on their clinical “mindlines” – those internal guidelines developed through experience. While clinical expertise is absolutely vital, it shouldn’t overshadow the importance of integrating new research findings.
Mentorship gaps create additional challenges, particularly for newer practitioners. Without experienced mentors to guide the integration of evidence into practice, early-career therapists can struggle to bridge the gap between academic training and real-world application. An AJOT report highlighted how crucial mentorship is for sustaining EBP skills throughout a therapist’s career.
Perhaps most concerning is the reality that over 64% of new graduates show a decline in EBP use within their first three years of practice. This “reality shock” phenomenon occurs when the ideals of academic training collide with the practical demands of clinical work. It’s a sobering reminder that good intentions aren’t always enough to maintain evidence-based practices.
The challenge of limited evidence in emerging areas also creates uncertainty. While the research base for occupational therapy in mental health continues to grow, gaps remain – particularly around cost-effectiveness studies and interventions for specific conditions. This can leave therapists feeling like they’re navigating without a complete map.
It’s worth noting that this isn’t just an occupational therapy problem. Healthcare broadly struggles with the gap between evidence and practice, as highlighted in investigations showing when evidence says no, but doctors say yes. The tendency to continue familiar practices despite contradictory evidence is a very human challenge.
At Thrive Mental Health, we recognize these barriers aren’t just obstacles to overcome – they’re realities that require systematic support and understanding. That’s why we’re committed to creating an environment where our therapists have the resources, time, and support they need to consistently deliver evidence-based care to our clients throughout Florida and beyond.
The Practitioner’s Journey: How OTs Grow and Sustain EBP Skills

Picture this: a fresh occupational therapy graduate walks into their first mental health setting, head full of research studies and evidence-based protocols. Fast-forward three years, and that same therapist might find themselves relying more on “what usually works” than the latest research findings. Sound familiar? You’re not alone – and more importantly, there’s a path forward.
The journey of mastering evidence based practice occupational therapy mental health isn’t a straight line. It’s more like learning to ride a bike while the road keeps changing beneath you. But here’s the encouraging news: the therapists who thrive in this field have finded some key strategies that make all the difference.
Lifelong learning becomes the fuel that keeps the EBP engine running. Our most successful therapists treat professional development not as a chore, but as an trip. They attend workshops, dive into continuing education, and approach clinical research with genuine curiosity. It’s not about cramming more information into an already busy brain – it’s about developing the skills to quickly spot quality evidence and weave it into daily practice.
Peer support emerges as perhaps the most powerful tool in sustaining EBP skills. Research shows us something fascinating: 67% of therapist discussions about EBP are facilitators rather than barriers. In other words, when therapists talk with colleagues about evidence-based approaches, they’re usually encouraging and supporting each other, not complaining about the extra work.
The magic happens in those informal moments – grabbing coffee with a colleague and discussing a challenging case, or sharing insights from a recent journal article during a team meeting. These conversations transform abstract research into practical, applicable knowledge that actually sticks.
But perhaps the most compelling motivator is witnessing positive patient outcomes firsthand. When you see a client make breakthrough progress because of an evidence-based intervention you implemented, it creates a powerful feedback loop. That success story becomes part of your clinical DNA, reinforcing why staying current with research matters so much.
The Early Career Experience with evidence based practice occupational therapy mental health
New graduates enter the field with impressive preparation. Two-thirds of new OT graduates report using EBP right out of school, armed with solid research skills and fresh knowledge of the latest interventions. Their academic training has equipped them well with EBP principles and the ability to formulate good clinical questions.
Then reality hits – and it hits hard. The transition from classroom to clinic can feel like jumping from a quiet library into a busy emergency room. Heavy caseloads demand immediate attention. Documentation piles up. Complex workplace cultures present unspoken rules about “how things are really done around here.”
This “reality shock” isn’t a personal failing – it’s a predictable part of professional development. The challenge lies in maintaining that initial enthusiasm for evidence-based approaches while learning to steer the practical demands of clinical practice. It’s like trying to follow a recipe while the kitchen is on fire around you.
The statistics tell the story clearly: over 64% of new graduates show a decline in EBP use during their first three years. But understanding this pattern helps us address it proactively rather than letting talented therapists drift away from best practices.
Cultivating a Career of Excellence in evidence based practice occupational therapy mental health
The therapists who buck this trend and maintain strong EBP practices throughout their careers share some common strategies. They’ve learned to work smarter, not harder, when it comes to staying evidence-informed.
Peer support networks become their secret weapon. Whether it’s joining a journal club, participating in online communities of practice, or simply making time for meaningful conversations with colleagues, these connections provide both practical support and professional motivation. Knowledge becomes less intimidating when it’s shared and discussed rather than tackled in isolation.
Mentorship relationships create bridges between academic ideals and clinical reality. Experienced therapists help newcomers prioritize information, interpret complex research findings, and integrate evidence with developing clinical intuition. This guidance proves invaluable in making EBP feel achievable rather than overwhelming.
As therapists mature in their practice, they develop what researchers call “mindlines” – internal guidelines that blend clinical experience with accumulated knowledge. Think of these as your professional GPS system, helping you steer complex cases efficiently. The key is keeping these mindlines flexible and open to updates based on new evidence.
Finding quality resources becomes an art form. Rather than drowning in information, successful practitioners learn to identify trusted sources like the Cochrane Library, which provides synthesized evidence in digestible formats. They develop efficient systems for staying current without becoming overwhelmed by the constant stream of new research.
At Thrive Mental Health, we’ve built our culture around supporting this professional growth journey. Our therapists in Florida benefit from collaborative environments that make evidence based practice occupational therapy mental health feel natural and sustainable rather than burdensome. We understand that when our therapists thrive professionally, our clients receive the exceptional care they deserve.
Conclusion
Our exploration of evidence based practice occupational therapy mental health shows us something beautiful: it’s not about following a rigid playbook, but about creating a thoughtful partnership between science, experience, and you. Think of it as a three-legged stool – the best research evidence, clinical expertise, and your personal values all working together to support your recovery journey.
This approach matters because it transforms how we deliver care. When we accept EBP, we’re not just being compassionate (though we absolutely are that too) – we’re being accountable, effective, and smart with resources. It’s how we ensure that every intervention we use, from social skills training to trauma-informed care, has a real purpose and proven track record of helping people like you reclaim meaningful participation in life.
Yes, implementing EBP consistently has its bumps in the road. Time pressures, heavy caseloads, and the very human tendency to stick with what feels familiar can all get in the way. But here’s what inspires us: the dedication of occupational therapists who never stop learning, who support each other through peer collaboration and mentorship, and who find their greatest motivation in watching you thrive.
The journey of mastering EBP is really a lifelong trip. It starts with solid training, faces some real-world challenges (that “reality shock” we talked about), but ultimately grows into something sophisticated and deeply rewarding when the right support systems are in place.
At Thrive Mental Health, we believe you should be more than a passive recipient of care – you should be an informed partner who asks questions, understands your treatment, and actively participates in your healing process. This collaborative spirit isn’t just nice to have; it’s the heart of what makes evidence based practice occupational therapy mental health truly effective.
If you’re ready for mental health support that blends rigorous evidence with genuine care, we’re here.
Thrive Mental Health offers flexible Intensive Outpatient Program (IOP) and Partial Hospitalization Program (PHP). These programs serve adults and young professionals across Florida – from Miami to Jacksonville. We provide both virtual and in-person options, custom-custom to your unique needs and schedule.
Ready to take the next step in your mental wellness journey?
Explore our evidence-based programs to find the gold standard of care you deserve.