Breaking the Clouds: How to Treat Autism and Depression Together

Autism and Depression Treatment: Hope in 2025
Autism and Depression Treatment [2025]: What Works, What to Avoid, and How to Start
Summary: Autism and depression treatment works best when it’s individualized, autism-informed, and combines modified therapy with thoughtful medication management.
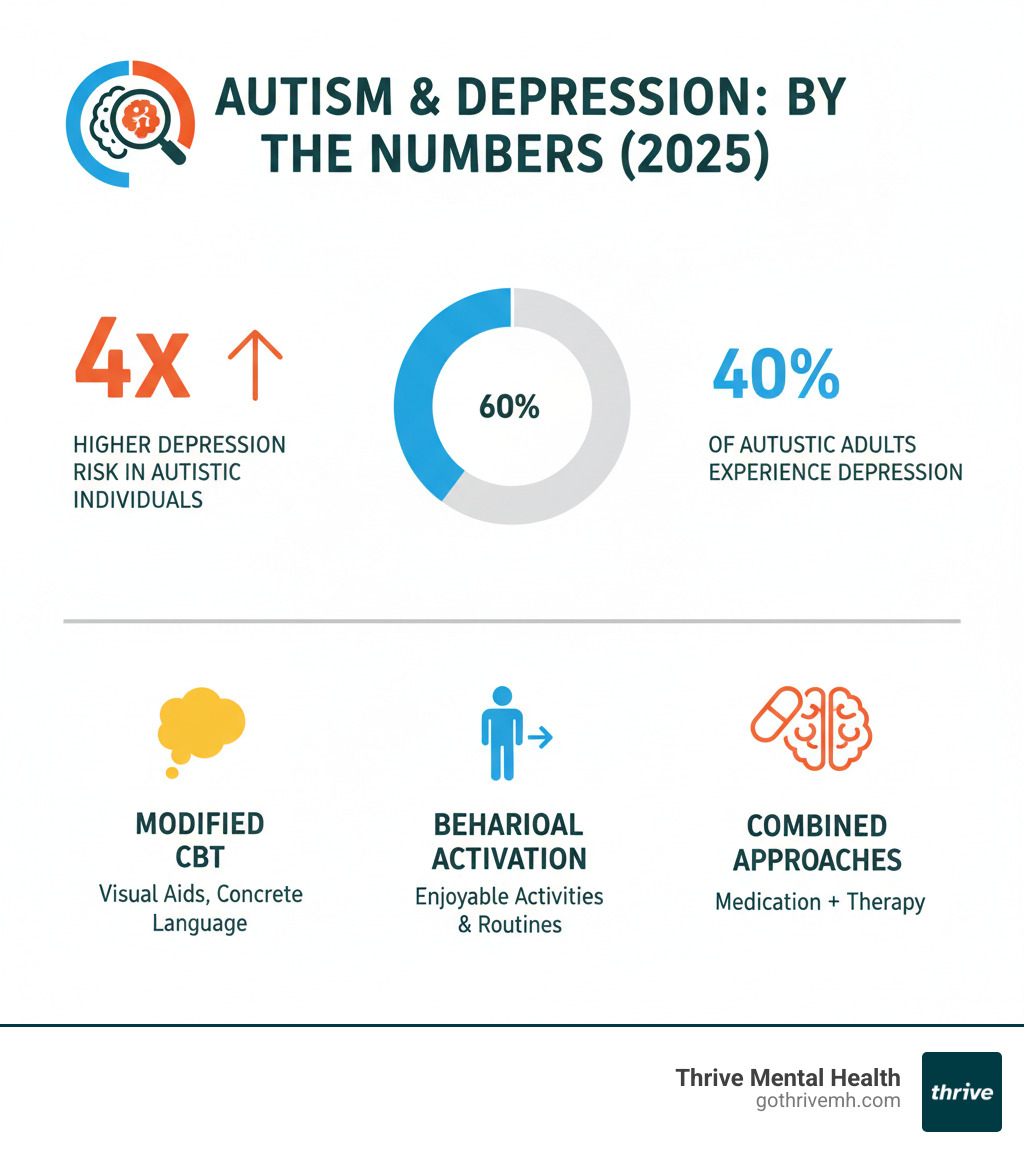
Autism and depression treatment requires a specialized approach because these conditions often occur together in ways that complicate traditional care. Research shows that autistic people are four times more likely to experience depression than the general population, with some studies finding depression rates as high as 40% in autistic adults.
Key Treatment Options for Autism and Depression:
- Modified Cognitive Behavioral Therapy (CBT) – Adapted with concrete language and visual aids
- Behavioral Activation – Focusing on enjoyable activities and routines
- Mindfulness-based interventions – Custom for autistic learning styles
- Medication (SSRIs) – Used cautiously with “start low, go slow” approach
- Combined therapy and medication – Often most effective when used together
The challenge lies in recognizing depression in autistic individuals. Symptoms often look different – increased irritability instead of sadness, worsening repetitive behaviors, or withdrawal that goes beyond typical autistic traits. Many clinicians miss these signs because they attribute them to autism itself rather than recognizing co-occurring depression.
What makes this even more complex is that traditional depression treatments need significant modifications to work for autistic people. Standard talk therapy approaches often fail because they don’t account for differences in communication styles, sensory needs, and information processing.
As Anna Green, LMHC, LPC, Chief Clinical Officer at Thrive Mental Health, I’ve seen how crucial specialized autism and depression treatment becomes when working with neurodiverse clients in our virtual IOP and PHP programs in Florida. My training in evidence-based therapies like EMDR and Mentalization-Based Therapy has shown me that individualized, autism-informed care makes all the difference in treatment outcomes.
Autism and depression treatment basics:
The Overlap: Why Depression is So Common in Autistic Individuals
If you’re autistic or love someone who is, you’ve probably noticed that depression seems to show up more often than it should. The statistics tell a sobering story: autistic people are four times more likely to experience depression than the general population.
While depression affects about 7% of all adults in the U.S. each year, the numbers jump dramatically for autistic individuals. The CDC estimates that 26% of people with autism experience depression, but adult rates paint an even starker picture – ranging from 50% to 77% in some studies. These aren’t just numbers; they represent real people struggling with overlapping challenges that make daily life incredibly difficult.
Social challenges create one of the biggest risk factors for depression in autistic individuals. Many autistic people find forming and maintaining relationships genuinely difficult, leading to profound loneliness and feelings of exclusion. Research on social impairments and depression shows that self-reported social struggles predict depression even when accounting for autism severity and cognitive ability.
The exhausting process of “masking” – trying to appear neurotypical in social situations – adds another layer of stress. Imagine spending your entire day performing a role that doesn’t feel natural. That constant effort to fit into neurotypical social norms can leave someone feeling emotionally drained and disconnected from their authentic self.
Bullying and trauma unfortunately occur far too often in the lives of autistic individuals. From childhood through adulthood, many face negative social experiences that leave lasting psychological scars. These cumulative traumatic events significantly contribute to depression risk, especially during the vulnerable transition to adulthood.
Sensory overload creates another pathway to depression that many people don’t consider. Imagine living in a world where the fluorescent lights feel like daggers, where the sound of the air conditioning is overwhelming, or where certain fabrics against your skin cause genuine distress. This constant sensory bombardment can lead to chronic stress and eventually depression.
Alexithymia – difficulty identifying and describing emotions – affects many autistic individuals and complicates both depression recognition and autism and depression treatment. When you can’t easily identify that you’re feeling sad or overwhelmed, those emotions can build up and manifest in unexpected ways.
Co-occurring anxiety frequently travels alongside depression in autistic individuals. The constant worry about social situations, sensory experiences, or changes in routine can create a perfect storm for depressive episodes.
There’s also a genetic predisposition component that researchers are still understanding. Families often see patterns of both autism and depression across generations, suggesting shared biological vulnerabilities.
Risk increases significantly during adolescence, when social pressures intensify and the gap between autistic and neurotypical experiences becomes more apparent. Young autistic people aged 13-17 show depression rates over 20%, and these numbers continue climbing into adulthood.
Interestingly, autistic individuals with average or above-average IQ sometimes face higher depression risk. Greater self-awareness of their differences and social difficulties can lead to more distress and rumination on negative experiences.
Understanding these interconnected risk factors is crucial for developing effective autism and depression treatment approaches that address the whole person, not just individual symptoms.
Spotting the Signs: How Depression Presents Differently in Autism

Recognizing depression in autistic individuals can feel like solving a puzzle where half the pieces look identical. The challenge isn’t just that depression symptoms can be subtle—it’s that they often hide behind behaviors we might already expect to see in autism.
Think about it: social withdrawal, reduced eye contact, and quiet communication are all common autistic traits. When depression enters the picture, these same behaviors might intensify, but they can easily be dismissed as “just autism.” This phenomenon, called diagnostic overshadowing, has historically led to missed opportunities for autism and depression treatment.
The situation becomes even more complex when we consider that many autistic people struggle with alexithymia—difficulty identifying and describing emotions. Someone might feel deeply sad or hopeless but lack the words to express it, or they might not even recognize these feelings as depression. For individuals with significant communication challenges, behavioral changes often become our primary clues.
Here’s what makes depression recognition particularly tricky: we need to look for changes from baseline rather than textbook symptoms. An autistic person’s depression might show up in several ways:
- Increased self-injurious behavior like head-banging or scratching.
- Sudden aggression or irritability, especially around routine changes.
- Loss of previously learned skills, such as personal hygiene or daily tasks.
- Intensified repetitive behaviors or stimming as a sign of distress.
- Worsening sleep patterns that disrupt carefully maintained schedules.
- Social withdrawal beyond their baseline, like suddenly stopping engagement with special interests or preferred people.
The key insight here is that depression in autism isn’t necessarily about looking sad in conventional ways. It’s about noticing when someone’s internal world shifts, even if they can’t tell us directly. Keeping a simple journal of behaviors, moods, and daily patterns can be incredibly helpful for spotting these subtle but significant changes.
Getting an accurate assessment requires working with professionals who understand neurodiversity and can distinguish between autism traits and co-occurring depression. This expertise is essential for developing effective autism and depression treatment plans that address both conditions appropriately.
A Custom Path Forward: Effective Autism and Depression Treatment

Finding the right treatment path when you’re dealing with both autism and depression isn’t about following a standard playbook—it’s about creating a completely personalized approach. Think of it like getting a custom-custom suit instead of grabbing something off the rack. What works beautifully for a neurotypical person with depression might miss the mark entirely for someone who’s autistic.
The most effective autism and depression treatment requires providers who truly understand neurodiversity. These aren’t just therapists who’ve read about autism in textbooks—they’re professionals who get how an autistic brain works differently, processes information uniquely, and experiences the world through a completely different lens.
At Thrive Mental Health, we’ve seen how crucial this individualized approach becomes for our clients in Florida. Our virtual and hybrid programs are specifically designed to accommodate the unique needs of neurodiverse clients, offering the flexibility and specialized care that makes all the difference in treatment outcomes.
Modified Psychotherapy for Autism and Depression Treatment
Traditional therapy approaches often fall short for autistic individuals, not because they’re ineffective treatments, but because they weren’t designed with neurodiversity in mind. It’s like trying to use a Windows program on a Mac—the basic functions might be similar, but you need the right operating system for everything to work smoothly.
Modified Cognitive Behavioral Therapy (CBT) represents one of the most promising approaches for autism and depression treatment. While standard CBT relies heavily on abstract thinking and verbal insight—areas where many autistic people face challenges—modified versions adapt these concepts brilliantly. Instead of asking “How does that make you feel?” a therapist might use concrete language and visual aids to help someone identify emotions through charts, pictures, or written examples.
The magic happens in the structured sessions that provide predictability and reduce anxiety. Many autistic clients thrive when they know exactly what to expect from each therapy appointment. Smart therapists also weave in special interests as powerful motivational tools. If someone’s passionate about trains, discussions about depression might center around how low mood affects their enjoyment of train documentaries or model building.
Research on evidence-based therapies shows how these adaptations can transform treatment outcomes. The key insight? We’re not changing the core therapeutic principles—we’re changing how we deliver them.
Behavioral Activation (BA) offers another powerful tool because it focuses on doing rather than just talking. This approach helps combat the withdrawal and loss of pleasure that depression brings by systematically scheduling enjoyable activities. For autistic individuals who might struggle to verbalize their emotions, this action-based therapy can feel much more accessible and concrete.
Dialectical Behavioral Therapy (DBT) brings valuable skills for emotional regulation and distress tolerance. Its structured, step-by-step approach to learning coping strategies often aligns well with how autistic minds prefer to process information. Rather than abstract concepts, DBT offers concrete tools that can be practiced and mastered.
The Role of Medication in Autism and Depression Treatment
Medication can play an important supporting role in autism and depression treatment, but it requires a thoughtful, specialized approach. The relationship between autism and antidepressants is complex, with research showing both promise and caution.
Selective Serotonin Reuptake Inhibitors (SSRIs) are commonly prescribed, but here’s where things get interesting—and a bit frustrating. Despite widespread use, we actually lack robust research specifically studying SSRIs for depression in autistic populations. Most of what we know comes from general depression studies or research focused on other autism-related symptoms.
What we do know is that autistic individuals often show higher sensitivity to side effects. This has led many specialists to adopt a “start low, go slow” approach, beginning with very small doses and increasing gradually while carefully monitoring for both benefits and adverse reactions.
Perhaps most importantly, research consistently shows that medication is most useful when combined with therapy. Think of medication as potentially helpful support rather than a standalone solution. The real therapeutic work often happens in those modified therapy sessions where someone learns new coping strategies and ways to steer their unique challenges.
Finding the right psychiatrist makes all the difference—someone who understands both autism and depression, who won’t dismiss concerning symptoms as “just autism traits,” and who can steer the delicate balance of medication management in neurodiverse individuals. This specialized expertise becomes crucial when considering that autistic individuals may have higher rates of other co-occurring conditions that could complicate treatment decisions.
The bottom line? Effective autism and depression treatment isn’t about finding a magic bullet—it’s about building a comprehensive, individualized plan that honors both the autism and the depression, treating the whole person rather than just isolated symptoms.
Navigating Crisis and Finding Hope [Important Safety Information]
Disclaimer: If you or someone you know is in crisis or thinking of suicide, please call or text 988 to reach the Suicide & Crisis Lifeline. They offer free, confidential support 24/7.

The connection between autism and depression carries a sobering reality that we must address head-on. Research shows that autistic adults face a nine times higher risk of suicidal thoughts compared to their neurotypical peers. This alarming statistic underscores why effective autism and depression treatment isn’t just importantit can be lifesaving.
Depression symptom severity serves as a significant predictor of suicide risk in autistic individuals. The combination of chronic social challenges, sensory overwhelm, and difficulty expressing emotional distress creates a perfect storm that can push someone toward crisis. Understanding this connection helps us recognize when immediate intervention becomes necessary.
Warning signs in autistic individuals may look different from what we typically expect. Beyond the standard indicators like talking about death or expressing hopelessness, watch for sudden changes in special interests, dramatic increases in self-injurious behaviors, or complete withdrawal from previously enjoyed activities. An autistic person might not verbally express suicidal thoughts but instead show through actionsgiving away treasured collections, abandoning routines they’ve maintained for years, or displaying uncharacteristic aggression.
When you notice these concerning changes, asking direct questions becomes crucial. Many people worry that bringing up suicide will plant the idea, but research consistently shows the opposite. Direct questions open doors to support rather than creating new problems. Questions like “Are you thinking about hurting yourself?” or “Have you thought about not wanting to be alive?” can provide the opening someone desperately needs to share their pain.
Creating a safety plan with a mental health professional familiar with autism provides concrete steps during crisis moments. These plans identify personal warning signs, coping strategies that work for that individual’s sensory and communication needs, and emergency contacts who understand their autism. For someone who struggles with phone calls, the plan might emphasize texting or using apps instead.
[Callout Box] If youre in crisis, call/text 988 right now. You are not alone.
Resources for neurodiverse and autistic people: https://988lifeline.org/help-yourself/individuals-with-neurodivergence/
The path through crisis toward hope requires understanding that suicidal thoughts don’t mean someone wants to diethey usually mean they want their pain to stop. With proper autism and depression treatment, that pain can be addressed, managed, and ultimately reduced. Many autistic individuals who’ve experienced suicidal thoughts go on to live fulfilling lives once they receive appropriate, autism-informed care.
Crisis is temporary, but the support and treatment that follows can create lasting change. Hope isn’t just possibleit’s probable when the right help is in place.
Finding the Right Support (and How to Pay for It)
Finding the right support for autism and depression treatment can feel overwhelming, but you don’t have to steer this journey alone. The most important step is connecting with autism-competent care—mental health professionals who truly understand how depression shows up differently in neurodiverse individuals and know how to adapt their approach accordingly.
When searching for the right therapist, resources like the Psychology Today therapist directory allow you to filter specifically for providers who specialize in autism. This can save you time and help ensure you’re connecting with someone who gets it from the start.
At Thrive Mental Health, we recognize that traditional therapy settings don’t work for everyone. Our virtual and hybrid programs bring expert-led, evidence-based care directly to you:
- Intensive Outpatient Program (IOP): https://gothrivemh.com/iop/
- Partial Hospitalization Program (PHP): https://gothrivemh.com/php/
- Virtual Therapy options: https://gothrivemh.com/virtual-therapy/
- Verify Insurance (2 minutes): https://gothrivemh.com/verify-insurance/
Our flexible treatment models mean you can access specialized autism and depression treatment from the comfort of your own space, right here in Florida. Evening options are available too, making it easier to fit treatment around work, school, or other commitments.
Insurance Coverage for Treatment
Here’s some good news: mental health parity laws require most insurance plans to cover mental health services at the same level as physical health care. This means that intensive outpatient and partial hospitalization programs are often covered by insurance. We work with many common providers including Cigna, Optum, and Florida Blue, among others. Verify your benefits here: https://gothrivemh.com/verify-insurance/
Want a deeper dive? Read our related blog on understanding mental health insurance: https://gothrivemh.com/blog/understanding-mental-health-insurance/
The financial aspect of treatment shouldn’t be another source of stress when you’re already dealing with so much. Getting clarity on your benefits allows you to focus on what matters most—your healing and recovery.
Frequently Asked Questions about Autism and Depression [Quick Answers]
What are early signs of depression in an autistic person?
Look for changes from baseline: more irritability, loss of interest in special interests, worse sleep, reduced self-care, or increased self-injury.
Does CBT work for autistic people with depression?
Yes—when adapted. Modified CBT uses concrete language, visuals, structure, and special interests to make skills easier to learn and use.
Are antidepressants (SSRIs) safe for autistic individuals?
Often helpful, but start low and go slow due to sensitivity to side effects. Combine meds with therapy and monitor closely with an autism-aware prescriber.
What’s the difference between autistic burnout and depression?
Burnout is exhaustion from chronic demands/masking and improves with rest and accommodations. Depression is a mood disorder that often needs therapy and sometimes medication.
How can I find autism-competent care near me?
Seek clinicians experienced with neurodiversity and ask about adapted approaches. Thrive offers specialized IOP/PHP and virtual therapy in Florida: https://gothrivemh.com/iop/, https://gothrivemh.com/php/, https://gothrivemh.com/virtual-therapy/
Suggested JSON-LD FAQ schema markup:
{
"@context": "https://schema.org",
"@type": "FAQPage",
"mainEntity": [
{
"@type": "Question",
"name": "What are early signs of depression in an autistic person?",
"acceptedAnswer": {"@type": "Answer", "text": "Look for changes from baseline: more irritability, loss of interest in special interests, worse sleep, reduced self-care, or increased self-injury."}
},
{
"@type": "Question",
"name": "Does CBT work for autistic people with depression?",
"acceptedAnswer": {"@type": "Answer", "text": "Yes—when adapted. Modified CBT uses concrete language, visuals, structure, and special interests to make skills easier to learn and use."}
},
{
"@type": "Question",
"name": "Are antidepressants (SSRIs) safe for autistic individuals?",
"acceptedAnswer": {"@type": "Answer", "text": "Often helpful, but start low and go slow due to sensitivity to side effects. Combine meds with therapy and monitor closely with an autism-aware prescriber."}
},
{
"@type": "Question",
"name": "What’s the difference between autistic burnout and depression?",
"acceptedAnswer": {"@type": "Answer", "text": "Burnout is exhaustion from chronic demands/masking and improves with rest and accommodations. Depression is a mood disorder that often needs therapy and sometimes medication."}
},
{
"@type": "Question",
"name": "How can I find autism-competent care near me?",
"acceptedAnswer": {"@type": "Answer", "text": "Seek clinicians experienced with neurodiversity and ask about adapted approaches. Thrive offers specialized IOP/PHP and virtual therapy in Florida."}
}
]
}
Conclusion
The connection between autism and depression runs deep, creating a complex web that requires careful understanding and specialized care. When depression goes untreated in autistic individuals, it doesn’t just affect mood—it can dramatically impact their ability to engage with their special interests, maintain relationships, and steer daily life. The ripple effects touch every aspect of their world, from work and school performance to family dynamics and personal growth.
But here’s what gives us hope: autism and depression treatment works when it’s done right. The key lies in moving away from cookie-cutter approaches and embracing truly individualized care. We’ve seen remarkable changes when autistic individuals receive therapy that speaks their language—literally and figuratively. Modified CBT that uses concrete examples instead of abstract concepts, visual aids that make complex emotions understandable, and therapists who genuinely understand neurodiversity can be life-changing.
The most encouraging part? We’re getting better at this every day. More clinicians are learning to recognize the subtle ways depression shows up in autistic people. We’re developing treatment approaches that honor both the autism and the depression, rather than trying to treat them as separate issues. And we’re creating spaces—like virtual therapy programs—that remove barriers and make quality care accessible.
At Thrive Mental Health, we’ve built our autism and depression treatment programs around this understanding for our clients in Florida. Our virtual IOP and PHP programs recognize that healing happens differently for everyone. Some of our clients thrive in the comfort of their own homes, away from overwhelming sensory environments. Others appreciate the flexibility to attend evening sessions that work around their routines and sensitivities.
What matters most is that specialized, evidence-based care is available. No one should have to steer this journey alone, and no one should settle for treatment that doesn’t truly understand their needs.
Ready for support? Thrive offers virtual and hybrid IOP/PHP with evening options. Verify your insurance in 2 minutes (no obligation) → https://gothrivemh.com/verify-insurance/ or call 561-203-6085. If you’re in crisis, call/text 988.