Beginner’s Guide to Understanding Trauma

What Is Trauma and Why Does It Matter?
Trauma is a psychological response to an event or series of events that overwhelm your ability to cope. It’s not about what happened, but about how your mind and body respond to the overwhelming experience.
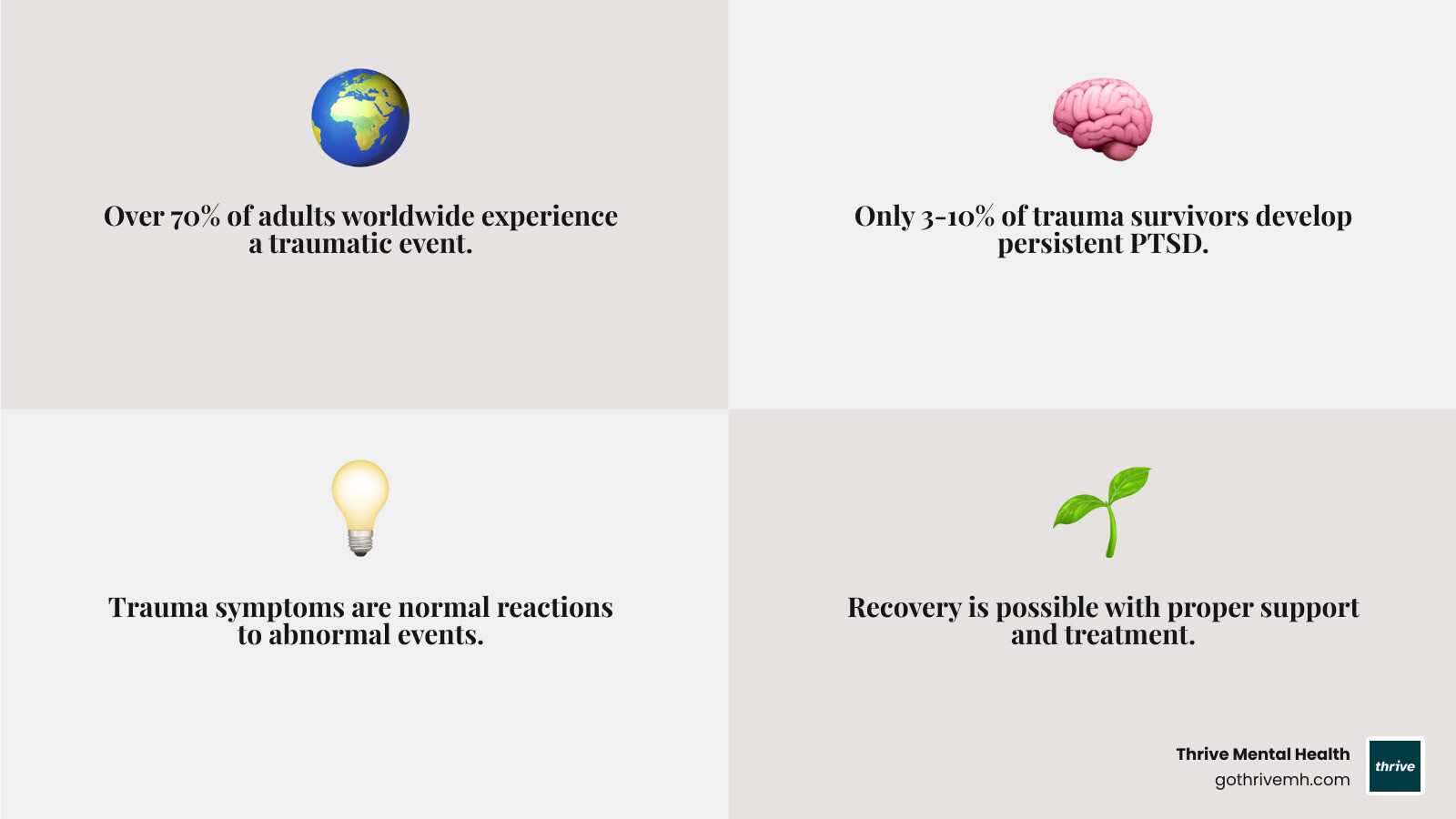
Quick Facts About Trauma:
- 60-75% of people in North America experience a traumatic event at some point
- Only 3-10% of people who experience trauma develop persistent mental health difficulties like PTSD
- 70% of adults worldwide have had at least one traumatic experience
- Trauma symptoms are normal reactions to abnormal events
- Recovery is possible with proper support and treatment
Trauma can result from many different experiences, from car accidents and natural disasters to abuse, neglect, or witnessing violence. What makes an event traumatic is how it affects you personally; the same situation might be traumatic for one person but not another.
Having trauma symptoms doesn’t mean you’re broken or weak. Your brain and body are doing what they’re designed to do when faced with overwhelming stress. As CEO of Thrive Mental Health, I’ve seen how trauma impacts busy professionals. My experience has confirmed that with evidence-based support, people can recover from trauma and build greater resilience.
What Is Psychological Trauma?
Trauma is your mind and body’s response to an experience that feels too overwhelming to handle. It’s like an internal alarm system that keeps ringing long after the danger has passed. Crucially, trauma isn’t about the event itself, but how your unique mind and body processed it. Two people can go through the same event with vastly different outcomes.
Defining Trauma
The American Psychological Association defines trauma as “an emotional response to a terrible event.” The key is that the event shatters your sense of security, leaving you feeling overwhelmed and unsafe. You might struggle with upsetting emotions, intrusive memories, or a constant sense of anxiety. Others may feel numb or disconnected.
To understand this better, professionals often use the “Three E’s” of trauma: the Event (what happened), the Experience (how you interpreted it), and the Effect (how it continues to impact you). The Substance Abuse and Mental Health Services Administration (SAMHSA) adds that trauma results from circumstances an individual experiences as physically or emotionally harmful or life-threatening, recognizing its wide range of sources.
The Different Types of Trauma
Understanding the different types of trauma can help you make sense of your experiences.

- Acute trauma results from a single, intense event, like a car accident or natural disaster.
- Chronic trauma stems from repeated exposure to distressing experiences, such as ongoing abuse or bullying.
- Complex trauma involves multiple traumatic events, often starting in childhood, which can deeply shape your sense of self and relationships. For more, see our article on effective complex PTSD counselling strategies and support.
- Secondary or vicarious trauma affects those who care for trauma survivors, like therapists or first responders, who absorb the emotional pain of others.
Common Causes of Trauma
Trauma can stem from a wide range of experiences, some less obvious than others. Common causes include:
- Abuse (physical, emotional, or sexual) and neglect during childhood.
- Accidents, such as car crashes or workplace injuries.
- Natural disasters that shatter your sense of security.
- Violence, including assault, robbery, or living in an unsafe community.
- Bullying, especially when persistent during formative years.
- Life-threatening illness or major medical procedures.
- Sudden loss of a loved one.
- Discrimination and racism, which create chronic, traumatic stress.
For those who have experienced sexual violence, our sexual trauma therapy page offers information on specialized support. If an experience felt overwhelming and continues to affect you, it is valid.
Recognizing the Symptoms of Trauma
When you experience trauma, your mind and body activate powerful protective mechanisms. These symptoms are not signs of weakness but your system’s attempt to keep you safe. Understanding them is a key step toward healing.
Emotional and Psychological Symptoms
Trauma can create a storm of confusing and intense emotions. You might find yourself navigating feelings you’ve never had before.

- Shock and Denial: It’s common to initially refuse to accept what happened, creating a mental buffer.
- Intense Emotions: You may experience overwhelming fear, anxiety, anger, irritability, sadness, or depression.
- Shame and Guilt: Many people blame themselves for the event or their reaction to it, even when it wasn’t their fault.
- Cognitive Difficulties: Confusion, difficulty concentrating, and a scattered mind are frequent symptoms.
- Numbness and Detachment: Feeling disconnected from your emotions or from others is a protective mechanism that can also block positive feelings.
- Re-experiencing: Flashbacks and nightmares can make you feel as if the trauma is happening all over again.
- Avoidance: You might go to great lengths to avoid people, places, or thoughts that remind you of the trauma.
These are normal reactions to abnormal events. For a deeper dive, explore our guide on understanding the emotional landscape of PTSD.
Physical Symptoms and Behaviors
Trauma resides in the body as much as it does in the mind. These physical symptoms are real manifestations of your body’s stress response.
- Hyperarousal: Your body may stay in a constant state of high alert, making you feel jumpy and easily startled.
- Fatigue: Despite feeling wired, you may be profoundly tired as your body works overtime to manage stress.
- Sleep Difficulties: Insomnia, racing thoughts at night, and frequent waking are common.
- Aches and Pains: Unexplained headaches, muscle tension, and digestive issues often appear as the body holds onto stress.
- Cardiovascular Symptoms: A racing heart or sweating during normal activities can occur as your body remains in a fight-or-flight state.
- Behavioral Changes: Some people turn to substance use to numb the pain, while others may withdraw socially. These maladaptive coping mechanisms can provide temporary relief but often create more problems.
These symptoms are your body’s attempt to protect itself. For help managing them, see our expert tips on coping with trauma.
The Lasting Impact on the Brain and Body
Trauma doesn’t just affect your thoughts and feelings—it can physically change how your brain works. These changes are your brain’s attempt to protect you, but they can make daily life more challenging.
How Trauma Rewires the Brain
When faced with overwhelming stress, your brain reorganizes itself for survival. This process involves three key areas.
- The amygdala, your brain’s smoke detector, can become hyperactive, keeping you in a constant state of high alert and triggering your fight-flight-freeze response.
- The hippocampus, your brain’s memory filer, can be impaired. This makes it difficult to store traumatic memories as past events, which is why flashbacks feel so immediate.
- The prefrontal cortex, your brain’s CEO, can become less effective at regulating emotions, making decisions, and thinking clearly under stress.
This rewiring is driven by a flood of stress hormones like cortisol. While helpful in the short term, prolonged exposure creates “toxic stress.” Research on how traumatic stress changes the brain shows how profound these changes can be. Understanding this helps us see that trauma symptoms are evidence of a brain working hard to protect you.
Understanding Childhood Trauma and ACEs
Trauma during childhood is particularly impactful because the brain is still developing. This is known as developmental trauma, and it can change how a child’s brain is wired, organizing it around survival instead of healthy growth.
The landmark ACE Study on Adverse Childhood Experiences revealed a powerful link between childhood trauma and adult health problems. The study found that 89% of U.S. adults have at least one ACE. Those with four or more ACEs are twice as likely to smoke, 7 times more likely to consider themselves alcoholic, and 12 times more likely to have attempted suicide.
While these statistics are sobering, they also point toward a path for healing. By understanding how childhood experiences shape adult challenges, we can begin to address them. The brain’s ability to change (neuroplasticity) means that healing can rewire the brain in healthier directions. It’s never too late to start that process, and our resources for overcoming childhood trauma can help.
The Connection Between Trauma and PTSD
Experiencing trauma does not automatically lead to PTSD. While the terms are often used interchangeably, trauma is the overwhelming experience, while PTSD is a specific mental health condition that can develop afterward. Most people are resilient and naturally recover from traumatic events over time.
What is Post-Traumatic Stress Disorder (PTSD)?
PTSD is a clinical diagnosis that may be made when trauma symptoms persist for more than a month and significantly interfere with daily life. It’s like the brain’s alarm system gets stuck in the “on” position. PTSD is typically characterized by four main symptom clusters:
- Re-experiencing: Unwanted intrusive memories, vivid flashbacks, and distressing nightmares.
- Avoidance: Actively avoiding people, places, thoughts, or feelings that remind you of the trauma.
- Negative Changes in Mood and Thoughts: Persistent negative beliefs about oneself or the world, feelings of guilt or shame, and emotional detachment.
- Changes in Arousal and Reactivity: Being easily startled, feeling constantly on edge (hypervigilance), having angry outbursts, or engaging in reckless behavior.
Symptoms can appear soon after the event or be delayed by months or even years. For a detailed look at the condition, explore our guide on understanding PTSD symptoms, causes, and treatment.
Comparing Acute Stress Disorder (ASD) vs. Post-Traumatic Stress Disorder (PTSD)
In the immediate aftermath of a traumatic event, some people experience Acute Stress Disorder (ASD). Understanding the difference between ASD and PTSD can help you know when to seek support. The key distinction is the duration of symptoms.
| Feature | Acute Stress Disorder (ASD) | Post-Traumatic Stress Disorder (PTSD) |
|---|---|---|
| Duration of Symptoms | 2 days to 4 weeks | More than 4 weeks (can be months or years) |
| Onset Time | Symptoms begin within 4 weeks of the traumatic event | Symptoms usually begin within 3 months of the traumatic event, but can be delayed for months or even years |
| Diagnostic Criteria | Requires 9 out of 14 symptoms from five categories (intrusion, negative mood, dissociation, avoidance, arousal) | Characterized by symptoms across four clusters: intrusion, avoidance, negative alterations in cognitions and mood, and alterations in arousal and reactivity |
| Relationship | Often seen as an early, acute response to trauma; effective treatment can reduce the likelihood of developing PTSD | A more persistent and chronic condition that can develop if ASD is left untreated or if the trauma is severe/prolonged |
Effective treatment for ASD can significantly reduce the chances of developing PTSD. Reaching out for support during this critical window can make a meaningful difference in your long-term recovery. Whether you’re dealing with ASD or PTSD, healing is possible.
Pathways to Healing: Treatment and Coping
The journey from trauma to healing is possible. Recovery works best when it combines professional support with personal coping strategies, much like healing a physical injury requires both medical treatment and physical therapy.
Professional Therapeutic Approaches
When trauma symptoms persist, professional help is invaluable. At Thrive Mental Health, we use a trauma-informed care approach, understanding that your reactions are coping strategies developed to protect you. Key evidence-based therapies include:
- Cognitive Behavioral Therapy (CBT): Helps identify and change negative thought patterns that keep you stuck in cycles of fear and avoidance.
- Eye Movement Desensitization and Reprocessing (EMDR): Uses bilateral stimulation (like guided eye movements) to help the brain process traumatic memories, reducing their emotional charge. Learn more about EMDR therapy here.
- Somatic Therapies: Focus on the mind-body connection, helping release trapped stress from the nervous system through gentle movement and body awareness.
- Psychodynamic Therapy: Explores how past experiences influence current emotional patterns and relationships.
- Medication: Antidepressants can help manage symptoms like anxiety and depression, making it easier to engage in therapy.
For a deeper look, explore the top 5 effective treatments for PTSD.
Self-Care and Coping Strategies
Daily choices can significantly support your healing. These strategies help regulate your nervous system and build resilience.
- Exercise and Movement: Rhythmic activities like walking or swimming help release pent-up energy.
- Mindfulness and Grounding: Techniques like deep breathing or the 5-4-3-2-1 method anchor you in the present moment.
- Connection: Spending time with trusted friends, family, or support groups reduces isolation.
- Creative Outlets: Art, music, or writing can help express emotions that are hard to verbalize.
- Routine: Predictable schedules for sleep, meals, and activities create a sense of safety.
- Healthy Habits: A balanced diet supports brain health, while avoiding self-medication with substances is crucial for healing.
For more ideas, see our article on effective strategies for managing trauma triggers.
How to Support a Loved One
Your patience and understanding can make a huge difference for a loved one who has experienced trauma.
- Listen without judgment and create a safe space for them to share.
- Offer practical support, like helping with daily tasks.
- Be patient with the healing process, as it is not linear.
- Educate yourself about trauma to better understand their reactions.
- Gently encourage professional help without pressure.
- Avoid minimizing their experience with phrases like “get over it.”
- Set boundaries to protect your own well-being.
Frequently Asked Questions about Trauma
Here are answers to some common questions about this complex topic.
Can you have trauma without developing PTSD?
Yes, absolutely. This is a critical distinction. Trauma is the emotional response to a distressing event. Most people who experience trauma will have some temporary symptoms like shock or anxiety that fade over time. PTSD is a specific clinical diagnosis with strict criteria that only a small percentage of people who experience trauma go on to develop. Having trauma symptoms is a normal reaction; it doesn’t automatically mean you have or will have PTSD.
What is the difference between “Big T” and “little t” trauma?
These are informal terms used to describe the scale of traumatic experiences. Both are valid and can have significant long-term effects.
- “Big T” trauma refers to major, life-threatening events that most people would recognize as traumatic, such as combat, a serious accident, or sexual assault.
- “little t” trauma refers to distressing events that are not necessarily life-threatening but still erode a person’s sense of safety and well-being. Examples include emotional neglect, chronic bullying, or a difficult divorce. The cumulative effect of “little t” traumas can be just as damaging as a single “Big T” event.
Can trauma be passed down through generations?
Yes, research shows that trauma can be passed down in a process known as intergenerational trauma. This can happen through learned behaviors and family dynamics, where a parent’s unresolved trauma impacts their children’s development. Furthermore, the field of epigenetics suggests that severe trauma can cause changes in how our genes are expressed—without altering the DNA itself. These epigenetic changes, which can affect stress responses, may then be passed down to offspring. You can explore the emerging research on intergenerational trauma to learn more. Understanding this doesn’t mean you are defined by your family’s history, but that healing can have a positive impact for generations to come.
Conclusion: Finding Your Path from Trauma to Triumph
Understanding trauma is the first step toward healing. It’s not about what happened to you, but about how your mind and body responded to protect you. Recovery is a journey, not a destination, and it is absolutely possible.
Your symptoms are not weaknesses; they are coping mechanisms that once served a purpose. With support, you can gently teach your nervous system that it’s safe to begin healing and learn new ways to steer the world.
Professional support is key on this path. Just as you would see a doctor for a physical injury, an expert can provide guidance for emotional wounds. At Thrive Mental Health, our flexible, expert-led programs are designed to help you process trauma and build lasting resilience without putting your life on hold.
Our virtual and in-person intensive outpatient programs are custom to your needs, whether you’re a busy professional or someone who needs the flexibility to heal at your own pace. Your trauma doesn’t define you, but your courage to heal does. Take that profound step toward not just surviving, but truly thriving.
Learn more about our virtual trauma program and find how we can support you on your path from trauma to triumph.
