From Trauma to Psychosis – Understanding Schizophrenia Risks
Can trauma cause schizophrenia: 2025 Insights
The Critical Link Between Trauma and Mental Health
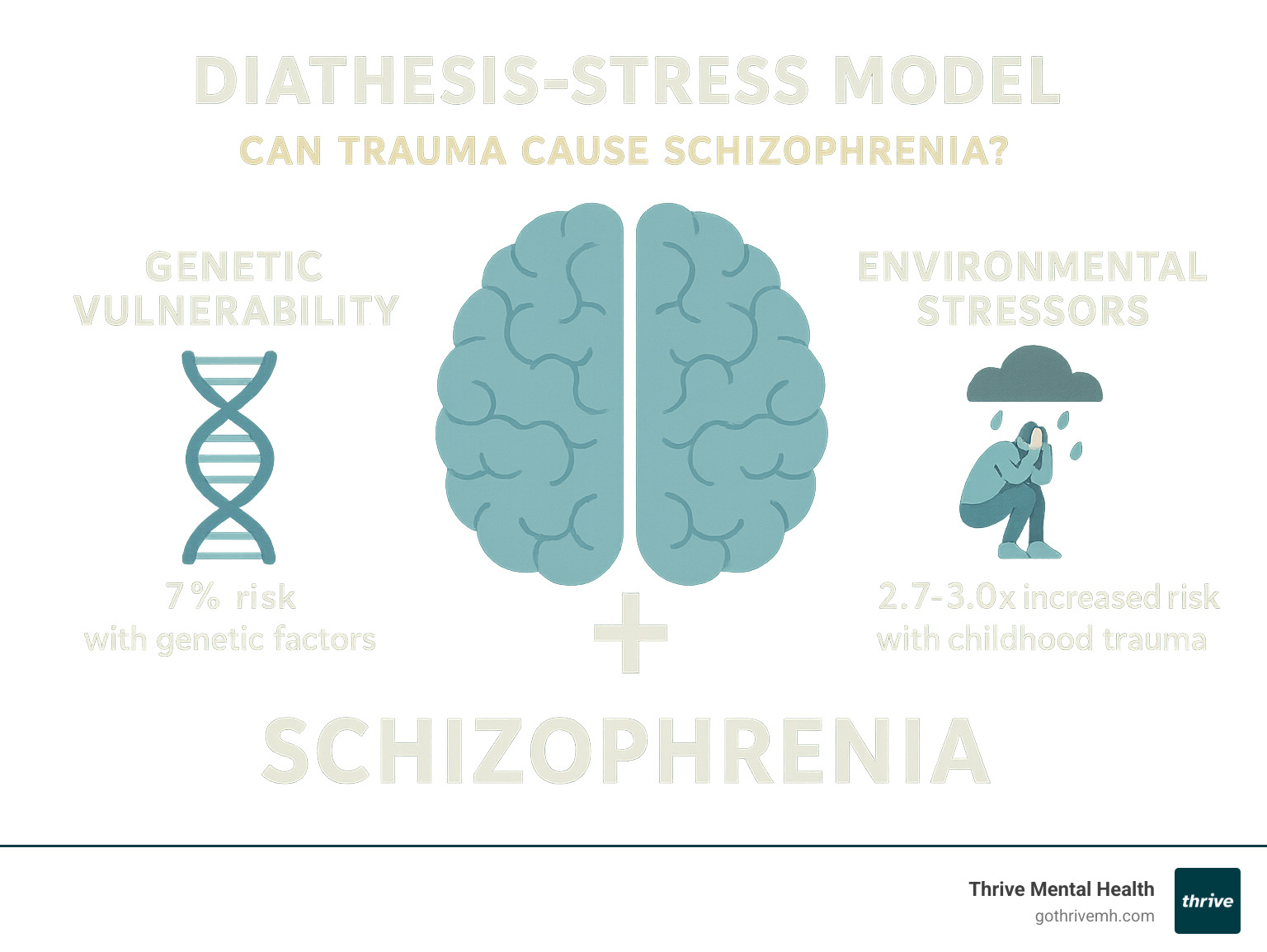
Can trauma cause schizophrenia? The answer isn’t a simple yes or no. Research shows that trauma – especially in childhood – significantly increases the risk of developing schizophrenia, but it rarely acts alone.
Here’s what the science tells us:
- Childhood trauma increases schizophrenia risk by 2.7-3.0 times according to large-scale studies
- Trauma acts as a trigger in people who already have genetic vulnerability
- Most people who experience trauma do not develop schizophrenia – other factors must be present
- The combination of genes + trauma creates the highest risk, following what experts call the “stress-diathesis model”
Schizophrenia is a complex mental health condition that affects how someone thinks, feels, and perceives reality. It involves symptoms like hallucinations, delusions, and disorganized thinking. While we once thought it was purely genetic, decades of research now show that environmental factors like trauma play a crucial role.
Trauma – whether it’s childhood abuse, neglect, or severe stress – doesn’t just leave emotional scars. It actually changes how the brain develops and functions. These biological changes can make someone more vulnerable to mental health conditions, including schizophrenia.
The relationship between trauma and schizophrenia follows something called the diathesis-stress model. Think of it like this: some people are born with a genetic “vulnerability” (diathesis). When life throws major stressors their way – like trauma – it can trigger the development of symptoms.
As Nate Raine, CEO of Thrive Mental Health, I’ve spent years working in behavioral health and have seen how understanding the trauma-schizophrenia connection is essential for effective treatment. Through my experience leading mental health programs, I’ve learned that addressing both trauma history and psychotic symptoms together leads to better outcomes for people wondering can trauma cause schizophrenia.
Can trauma cause schizophrenia vocabulary:
The Complex Causes of Schizophrenia: A Multifactorial Puzzle
Schizophrenia is a severe mental health condition characterized by psychosis, a decline in function, and deficits in social, emotional, and cognitive abilities. Its exact causes remain unknown, but current understanding points to a complex interplay of physical, genetic, psychological, and environmental factors. It’s never just one thing; rather, it’s a combination of these elements that can increase a person’s likelihood of developing the condition.
The Genetic Blueprint: What Twin Studies Reveal
Genetics play a significant role in schizophrenia, as the condition tends to run in families. However, it’s crucial to understand that no single gene is solely responsible. Instead, it’s often a combination of different genes that can make an individual more vulnerable.
Twin studies provide compelling evidence for this genetic component. For identical twins, who share nearly 100% of their genes, if one twin develops schizophrenia, the other has a 1 in 2 chance of developing it as well, even if they are raised separately. This high concordance rate highlights the strong genetic influence.
However, genetics aren’t the only factor. In non-identical twins, who share roughly 50% of their genes (like any other siblings), if one twin develops schizophrenia, the other has only about a 1 in 8 chance of developing the condition. While this is still higher than the 1 in 100 chance seen in the general population, it clearly demonstrates that genes alone do not dictate whether someone will develop schizophrenia. Environmental and other factors are always at play.
Brain Development and Neurotransmitter Imbalances
Research suggests that schizophrenia may partly be a disorder of the brain itself. Studies have revealed subtle differences in brain structure in individuals with schizophrenia compared to those without the condition. These changes are not universal, but they point to potential underlying neurological differences.
The function of neurotransmitters—chemicals that carry messages between brain cells—is also thought to be crucial. Imbalances in these chemical messengers, particularly dopamine, are heavily implicated in schizophrenia. Medications that help regulate dopamine levels can often alleviate symptoms, supporting this hypothesis. Other neurotransmitters, like glutamate and serotonin, are also believed to play a role in the complex neurobiology of the disorder. For more detailed information on brain-related causes, Mind offers valuable insights into What causes schizophrenia?.
Early Life Risk Factors: Pregnancy and Birth Complications
The journey to schizophrenia can sometimes begin even before birth. Research indicates that individuals who develop schizophrenia are more likely to have experienced complications during pregnancy or delivery. Factors such as low birthweight, premature labor, or a lack of oxygen (asphyxia) during birth can affect early brain development, potentially increasing vulnerability to the condition later in life. Additionally, maternal infections or malnutrition during pregnancy have been studied as potential early environmental risk factors.
Can Trauma Cause Schizophrenia? Examining the Powerful Role of Environment
Here’s where things get really interesting. While genes and brain chemistry set the stage, environmental triggers often determine whether someone actually develops schizophrenia. Think of it like having a loaded gun – genetics provide the ammunition, but environmental factors pull the trigger.
The most powerful environmental triggers include childhood adversity, major life stressors, and substance use. These don’t work in isolation, though. They’re most dangerous when they interact with someone who’s already genetically vulnerable.

How does childhood trauma increase the risk for schizophrenia?
Childhood trauma is one of the strongest environmental risk factors for developing schizophrenia later in life. The numbers are striking: people who experienced significant childhood adversity have 2.7 to 3.0 times higher odds of developing psychosis or schizophrenia compared to those who didn’t.
But not all trauma affects the brain the same way. Emotional neglect appears to be the most common type of childhood trauma found in people with schizophrenia. Physical abuse and sexual abuse also significantly increase risk, but emotional neglect – being ignored, dismissed, or emotionally unavailable caregiving – seems to be particularly damaging to developing brains.
Why does childhood trauma have such lasting effects? Because it literally changes how the brain develops. When a child experiences repeated trauma, it disrupts the normal growth of brain areas responsible for working memory, executive function, and attention – the exact same cognitive abilities that are often impaired in schizophrenia.
This isn’t just about psychological scars. Trauma creates biological changes that make someone more vulnerable to mental health conditions. For those wondering can trauma cause schizophrenia, the answer is that trauma rewires the brain in ways that significantly increase risk, especially when combined with genetic vulnerability. You can see the complex biological pathways in scientific research on the pathophysiological pathways between trauma and schizophrenia.
The Impact of Stressful Life Events
Trauma doesn’t stop affecting us after childhood. Major stressful life events at any age can trigger schizophrenia in someone who’s already vulnerable. We’re talking about experiences like losing a loved one, going through a divorce, losing a job, or experiencing abuse as an adult.
The key thing to understand is that these events don’t cause schizophrenia in everyone – only in people who already have that underlying vulnerability. It’s like the final straw that breaks the camel’s back.
Social-evaluative stress – situations where you feel judged or criticized – and uncontrollable situations seem to be particularly triggering. People with high-trait reactivity (those who are naturally more sensitive to stress) are especially at risk for having their symptoms worsen when faced with these situations.
This is why understanding someone’s stress response is so important in treatment. At Thrive Mental Health, we see how addressing both trauma history and current stressors helps people manage their symptoms more effectively.
Substance Abuse as a Catalyst for Psychosis
Here’s something that might surprise you: drug use can be both a trigger and a consequence of schizophrenia risk. Some people use substances to cope with early symptoms, while others find that drug use triggers their first psychotic episode.
Cannabis has gotten a lot of attention in research, and for good reason. Regular use of high-potency cannabis by teenagers and young adults significantly increases the risk of developing schizophrenia. The stronger the cannabis (higher THC content), the greater the risk appears to be.
Other substances that can trigger psychotic episodes include cocaine, LSD, and amphetamines. These drugs can either trigger the initial onset of symptoms or cause relapses in people already diagnosed with schizophrenia.
What makes this particularly concerning is that the teenage and young adult years – when many people first experiment with drugs – are also the peak years for schizophrenia to first appear. It’s a dangerous combination of timing and vulnerability.
For anyone struggling with both substance use and mental health concerns, it’s crucial to address both issues together. Mind offers helpful information on how recreational drugs can affect mental health.
The Neurobiology of Trauma: How Stress Rewires the Brain
When we ask “can trauma cause schizophrenia,” we’re really asking about one of the most fascinating and complex processes in neuroscience: how our experiences literally reshape our brains. The relationship between trauma and schizophrenia isn’t just psychological – it’s deeply biological.
The neurodevelopmental hypothesis of schizophrenia suggests that the disorder stems from early brain changes that don’t show up until later in life. Think of it like a house with a foundation that looks fine but has subtle cracks. Everything seems normal until stress tests the structure, and then problems emerge.
Trauma, especially during childhood when our brains are still developing, can profoundly influence these processes. It’s not just that trauma “hurts” – it actually creates lasting biological changes that can increase someone’s vulnerability to developing schizophrenia later.
The Stressed Brain: HPA Axis, BDNF, and Epigenetic Changes
Your body has a built-in alarm system called the HPA axis (hypothalamic-pituitary-adrenal axis). When you face stress or trauma, this system releases hormones like cortisol to help you cope. It’s designed to handle short-term emergencies, like running from a bear.
But when trauma is chronic or severe – like ongoing childhood abuse – this system gets stuck in “emergency mode.” The constant flood of stress hormones starts damaging important brain areas, particularly the hippocampus (which handles memory) and the prefrontal cortex (which manages thinking and decision-making). It’s like having a car alarm that won’t turn off – eventually, it damages the car’s electrical system.
Another key player is Brain-Derived Neurotrophic Factor (BDNF), a protein that acts like fertilizer for brain cells. It helps neurons grow, survive, and form new connections. Trauma and chronic stress can reduce BDNF levels, making it harder for the brain to maintain healthy function and adapt to challenges.
Perhaps most remarkably, trauma can create changes through epigenetics – modifications that affect how genes are expressed without changing the DNA itself. Think of your genes like a piano. Epigenetic changes don’t add or remove keys, but they can make certain keys harder or easier to press.
DNA methylation and histone modification are two ways trauma can “tune” this genetic piano. Childhood trauma can essentially flip switches that make someone more sensitive to stress for the rest of their life. This oxidative stress creates inflammation and makes it harder to regulate emotions, further contributing to these lasting changes.
What is the evidence linking childhood trauma to schizophrenia?
The research connecting childhood trauma to schizophrenia is both extensive and compelling. In one major study of 406 patients with schizophrenia spectrum disorders, researchers found clear links between early trauma and the cognitive problems that define the condition.
People who experienced physical abuse, sexual abuse, or physical neglect as children showed significant difficulties with working memory, executive function, and verbal tasks. These aren’t just minor differences – they’re the same cognitive impairments that make daily life challenging for people with schizophrenia.
Brain imaging studies reveal the physical evidence of these connections. Childhood trauma is associated with hippocampal volume reduction and prefrontal cortex alterations – actual structural changes in brain regions crucial for memory, thinking, and emotional regulation.
These changes also affect functional connectivity – how different brain regions communicate with each other. It’s like having a phone system where some lines are damaged, making it harder for different departments to coordinate effectively.
Gene-Environment Interactions: A Risky Combination
Here’s where the story gets really interesting: not everyone who experiences trauma develops schizophrenia. The key lies in gene-environment interactions – how specific genetic variations influence how someone responds to traumatic experiences.
Several genes play crucial roles in this process. The COMT gene affects how quickly your brain breaks down dopamine, a neurotransmitter involved in thinking and emotion. The FKBP5 gene influences stress hormone regulation, while BDNF val66met affects that brain fertilizer protein we discussed earlier.
The 5-HTTLPR gene variant affects serotonin transport, influencing mood and stress sensitivity. People with certain versions of these genes may be more vulnerable to trauma’s effects on brain development and function.
Research on BDNF val66met and trauma in psychosis shows that individuals with specific BDNF genotypes are more susceptible to the negative brain effects of childhood trauma. This helps explain why some people exposed to similar traumas develop schizophrenia while others don’t – their unique genetic makeup creates different levels of vulnerability.
This genetic-environmental interaction is why understanding both trauma history and family mental health history is so important in treatment. It’s not just about what happened to someone, but how their individual biology responded to those experiences.
Getting the Right Diagnosis and Treatment [Your Path to Recovery]
When you’re wondering can trauma cause schizophrenia, getting the right diagnosis becomes absolutely critical. The symptoms can be confusing and often overlap with other mental health conditions, which is why a thorough, comprehensive assessment is so important.
At Thrive Mental Health, we understand that each person’s journey is unique. Our integrated treatment approaches are designed to address not just the symptoms you’re experiencing, but the whole picture – including any trauma history that might be contributing to your current struggles.

Is It Schizophrenia, PTSD, or Both?
Here’s where things get tricky: the symptoms of trauma-related conditions can look surprisingly similar to schizophrenia. This overlap makes diagnosis challenging, but understanding it is crucial for getting the right treatment.
Post-Traumatic Stress Disorder (PTSD) can include hallucinations, social withdrawal, and dissociative symptoms like feeling detached from reality or having memory problems. Sound familiar? These symptoms can easily be mistaken for schizophrenia, especially when someone has experienced severe childhood trauma.
Major Depressive Disorder and Bipolar Disorder can also share features with schizophrenia, particularly when psychotic symptoms are present during severe episodes. The challenge is that trauma doesn’t just affect one area of mental health – it has what researchers call “transdiagnostic effects,” meaning it can influence multiple conditions at once.
This is why a comprehensive assessment that looks at your complete trauma history alongside your current symptoms is so important. Sometimes people have both PTSD and schizophrenia. Sometimes what looks like schizophrenia is actually severe PTSD. Getting this right from the start makes all the difference in your recovery journey.
Integrated Treatment for Co-Occurring Conditions
If you’re dealing with both trauma and psychotic symptoms, treating them separately just doesn’t work well. The trauma can make psychotic symptoms worse, and untreated psychosis can make it nearly impossible to process and heal from trauma. That’s why we use an integrated approach.
Cognitive Behavioral Therapy (CBT) helps you identify and change thought patterns that might be contributing to both trauma symptoms and psychotic experiences. Trauma-focused therapies provide a safe space to process difficult memories while building coping skills.
Our Intensive Outpatient Programs (IOP) and Partial Hospitalization Programs (PHP) are designed with flexibility in mind. You can access expert-led, evidence-based care from anywhere, with evening options that work around your schedule.
We also offer group therapy sessions where you can connect with others who understand your experiences, family therapy to help rebuild important relationships, and psychiatric medication management to address the biological aspects of your condition.
Paying for Care in Florida
Quality mental health care should be accessible, not a luxury. That’s why we work with major insurance providers to make our programs affordable for people in Florida.
We accept many major insurance providers, including:
- Cigna
- Optum
- Florida Blue
- Aetna
Coverage can vary between in-network and out-of-network benefits, so we make it easy to understand exactly what your plan covers.
You can verify your insurance coverage in 2 minutes right on our website – no obligation, no hassle. Just quick answers about your benefits so you can focus on what really matters: getting the support you need.
Frequently Asked Questions about Trauma and Schizophrenia
When people first learn about the connection between trauma and schizophrenia, they often have many questions. These are some of the most common ones we hear from families and individuals seeking answers.
What is the difference between trauma-induced psychosis and schizophrenia?
This is an important distinction that many people find confusing. Psychosis is a symptom – it’s essentially a break from reality that can include hallucinations, delusions, or severely disorganized thinking. Think of it like a fever – it’s a sign that something’s happening, but it’s not the illness itself.
Schizophrenia, on the other hand, is a complex, long-term mental illness that involves psychosis but also includes other symptoms like cognitive difficulties, social withdrawal, and problems with motivation. It’s a chronic condition that requires ongoing management.
Here’s where it gets interesting: severe trauma can trigger a brief psychotic episode that may resolve relatively quickly and never develop into full schizophrenia. However, for people who already have a genetic predisposition, trauma can be the key environmental trigger that leads to the onset of schizophrenia. Can trauma cause schizophrenia in these vulnerable individuals? It’s more accurate to say trauma can trigger its development.
Can you develop schizophrenia without any trauma?
Absolutely. While trauma is a significant risk factor that we can’t ignore, schizophrenia is what we call multifactorial – meaning multiple factors contribute to its development.
A person can develop schizophrenia due to a strong genetic predisposition combined with other biological factors, brain chemistry imbalances, or even birth complications, all without having experienced significant trauma. Remember those twin studies we discussed earlier? Even identical twins don’t always both develop the condition, showing that genetics alone aren’t destiny.
This is why the diathesis-stress model is so helpful in understanding schizophrenia. Some people might have a high genetic vulnerability but never encounter the environmental stressors that would trigger symptoms. Others might have moderate genetic risk but experience severe trauma that pushes them over the threshold.
At what age does schizophrenia typically appear?
Schizophrenia has a fairly predictable timeline, which can actually be helpful for early intervention. Most cases emerge between the late teens and early 30s, but there are some important gender differences to know about.
Men typically develop symptoms earlier – usually in their late teens to early 20s. Women tend to develop symptoms slightly later – typically in their early 20s to early 30s. This difference might be related to hormonal factors, particularly estrogen’s protective effects on the brain.
It’s rare for schizophrenia to first appear in childhood or after age 45, though it can happen. The peak risk period aligns with major life transitions like starting college, entering the workforce, or other stressful life changes that can act as triggers in vulnerable individuals.
Is schizophrenia caused by bad parenting?
This is one of the most harmful myths about schizophrenia, and I want to address it directly: No, schizophrenia is not caused by bad parenting. This outdated belief has caused tremendous guilt and pain for families already dealing with a challenging situation.
Schizophrenia is a neurobiological disorder – it involves real changes in brain structure and chemistry. While we know that a stressful, abusive, or neglectful childhood environment can be a risk factor that contributes to its onset, it absolutely does not “cause” the illness on its own.
The difference is crucial: trauma and stress can trigger schizophrenia in someone who already has a biological vulnerability, but they don’t create that vulnerability. Many people experience difficult childhoods without developing schizophrenia, and many people with loving, supportive families still develop the condition.
Understanding this distinction is essential for families seeking help. Instead of focusing on blame, we can focus on what really matters: getting effective, compassionate treatment that addresses both the biological aspects of schizophrenia and any trauma history that might be present.
Conclusion
The question can trauma cause schizophrenia doesn’t have a simple yes or no answer. What we’ve learned through decades of research is that trauma – especially during childhood – acts as a powerful risk factor that can trigger schizophrenia in people who already have genetic vulnerabilities.
The diathesis-stress model gives us the clearest picture: some people are born with a biological predisposition (the diathesis), and when they encounter severe stressors like trauma (the stress), it can set off the complex chain of events that leads to schizophrenia. This explains why childhood trauma increases schizophrenia risk by nearly three times, yet most trauma survivors never develop the condition.
Recovery is absolutely possible with the right support and treatment approach. The key is understanding that if trauma played a role in triggering someone’s schizophrenia, then addressing both the psychotic symptoms and the underlying trauma history gives people the best chance at healing.
At Thrive Mental Health, we’ve built our programs around this understanding. Our integrated approach treats trauma and schizophrenia together, not as separate issues. Whether you’re in Florida or anywhere else, our virtual and hybrid programs make evidence-based care accessible when you need it most.
We know that seeking help can feel overwhelming, especially when you’re dealing with complex mental health challenges. That’s why we’ve made the first step as simple as possible – you can verify your insurance coverage in just two minutes, with no pressure or obligation.
Ready for support? Thrive offers virtual and hybrid IOP and PHP programs with evening options. Verify your insurance in 2 minutes (no obligation) → Start benefits check or call 561-203-6085. If you’re in crisis, call/text 988.