Choosing Between CBT and DBT Therapy Without Losing Your Mind

Decoding the Alphabet Soup of Therapy
Choosing the right mental health support can feel like navigating an alphabet soup. Among the many options, CBT and DBT often come up, and it’s easy to wonder how they differ. Both are powerful tools for improving your well-being, but they shine in slightly different situations.
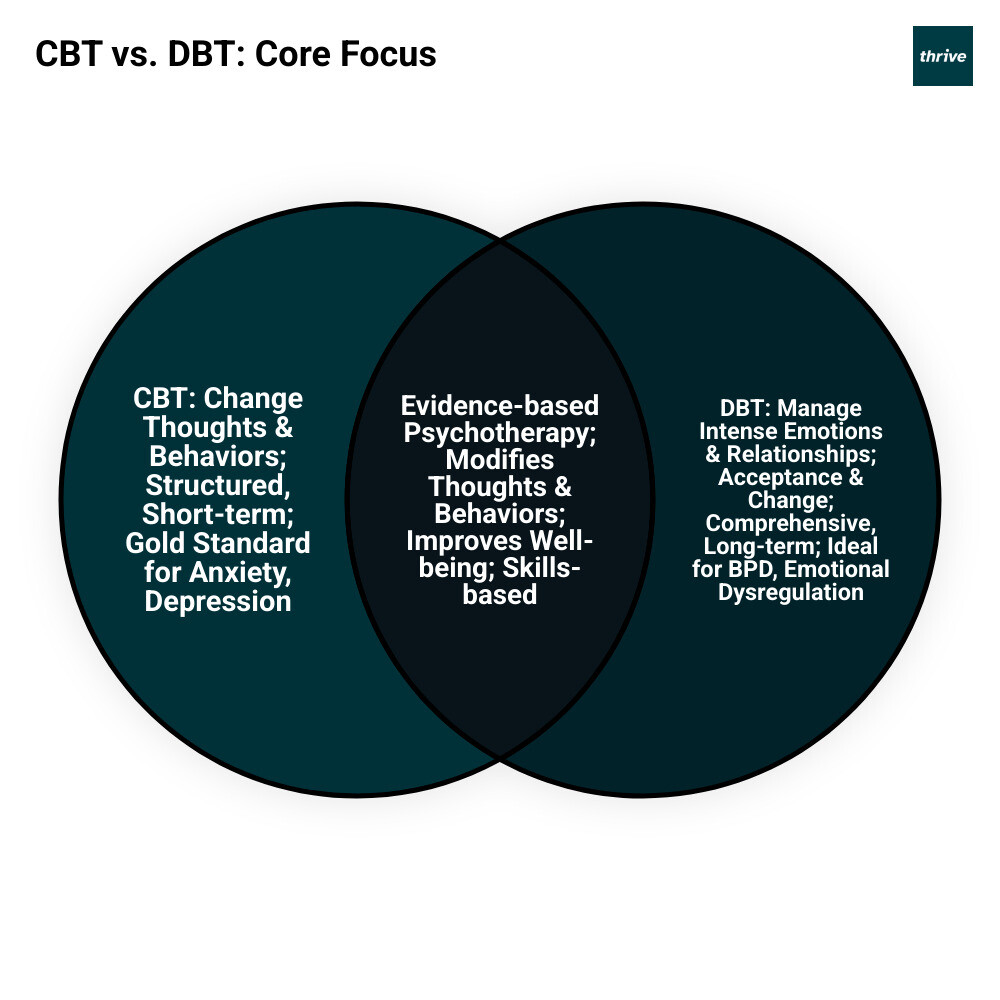
Here’s a quick look at their core distinction:
- Cognitive Behavioral Therapy (CBT): Focuses on identifying and changing unhelpful thought patterns and behaviors to improve feelings. It’s often structured and short-term.
- Dialectical Behavior Therapy (DBT): An evolution of CBT that adds a strong emphasis on managing intense emotions, distress tolerance, and interpersonal skills, often involving both acceptance and change. It’s typically more comprehensive and longer-term.
Understanding these differences is key to finding the path that best supports your unique journey.
As CEO of Thrive, I oversee mental health programs, including those featuring CBT and DBT skills, ensuring effective, evidence-based care. My focus is on creating impactful solutions that bridge behavioral health with broader healthcare needs, delivering measurable results for patients.
The Foundations: What Are Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT)?
Before we dive into choosing between CBT and DBT, let’s explore what makes each of these therapeutic approaches so powerful. Think of them as different tools in a mental health toolkit – both designed to help you steer life’s challenges, but each with its own special strengths.
Both therapies fall under the umbrella of psychotherapy, or “talk therapy.” They’re not just about talking through problems, though. These approaches give you practical skills and strategies to build healthier responses to whatever life throws your way.
Cognitive Behavioral Therapy (CBT): The Gold Standard for Changing Thought Patterns
Cognitive Behavioral Therapy (CBT) has earned its reputation as the gold standard for good reason. It’s structured, goal-focused, and deals with what’s happening in your life right now – not just what happened years ago.
Here’s the core idea behind CBT: your thoughts, feelings, and behaviors are all connected in what we call the thoughts-feelings-behaviors triangle. Picture this – if you think “Nobody likes me” (thought), you might skip that work happy hour (behavior) and end up feeling isolated (feeling). CBT helps you spot these patterns and break the cycle.
The main goal is helping you recognize when your thinking gets stuck in unhelpful patterns. Maybe you’re telling yourself “I’m terrible at everything” after one mistake at work. CBT teaches you to question that thought – is it really true? What evidence supports it? What would you tell a friend in the same situation?
This process is called cognitive restructuring, and it’s like becoming your own detective. You learn to challenge distorted thoughts and develop more balanced, realistic ways of thinking. CBT also focuses on problem-solving skills, giving you practical tools to tackle real-world challenges.
The philosophical roots of CBT actually go way back to Stoicism – the ancient idea that our emotions come more from how we interpret events than from the events themselves. CBT therapists often use the Socratic method, asking thoughtful questions to guide you toward your own insights rather than just telling you what to think.
What makes CBT so trusted is the mountain of research behind it. Studies consistently show its effectiveness across many mental health conditions, which is why it’s considered a gold standard due to extensive evidence-based research. For a deeper dive into how CBT works, check out The Ultimate Guide to Understanding Cognitive Behavioral Therapy (CBT).
Dialectical Behavior Therapy (DBT): An Evolution of CBT for Intense Emotions
Dialectical Behavior Therapy (DBT) takes CBT and adds some powerful new elements, especially for people dealing with overwhelming emotions. Dr. Marsha Linehan developed DBT in the 1970s when she realized that traditional CBT wasn’t quite cutting it for people with intense emotional experiences, like those with Borderline Personality Disorder.
The word “dialectical” might sound fancy, but it simply means balancing two seemingly opposite ideas. DBT’s genius is in teaching you to accept yourself exactly as you are while simultaneously working to change and grow. It’s like saying “I’m struggling right now, and that’s okay” while also saying “I’m committed to building the skills I need to feel better.”
DBT draws heavily from Zen Buddhism and mindfulness practices. The philosophical foundation centers on the balance between acceptance and change – learning to sit with difficult emotions without being overwhelmed by them, while also developing skills to create positive change in your life.
DBT teaches practical skills through four core areas:
Mindfulness helps you stay present and observe your thoughts and feelings without getting caught up in them. Distress tolerance gives you tools to ride out emotional storms without making things worse through destructive behaviors. Emotion regulation teaches you to understand and manage intense feelings, while interpersonal effectiveness focuses on communicating your needs and maintaining healthy relationships.
Unlike CBT’s focus on changing thoughts, DBT emphasizes validation – acknowledging that your emotions make sense given your experiences. It’s comprehensive support that recognizes some people need more than just cognitive techniques to heal.
To learn more about how DBT can support your mental health journey, explore How Dialectical Behavior Therapy (DBT) Can Improve Mental Health.
Head-to-Head Comparison: Key Differences in CBT and DBT
Now that we understand the foundations of both therapies, let’s explore how CBT and DBT actually differ in practice. While they share some common ground, their approaches are quite distinct – think of them as two different recipes for mental wellness, each with its own special ingredients and cooking methods.

Approach to Emotions and Thoughts
The biggest difference between these therapies lies in how they handle our emotional experiences and thought patterns.
CBT takes a “detective” approach to our thoughts. It helps us identify those sneaky, unhelpful thought patterns that might be making us feel worse than we need to. The goal is to challenge and change these thoughts into more balanced, realistic ones. If you’re terrified of giving a presentation because you’re convinced everyone will think you’re incompetent, CBT helps you examine the evidence and develop a more realistic perspective. It also uses behavioral activation – encouraging you to take positive actions even when you don’t feel like it, which can help break cycles of depression or anxiety.
DBT takes a different path entirely. Instead of immediately trying to change how you think, it starts with validation and radical acceptance. DBT says, “Hey, it’s completely understandable that you’re feeling this intense emotion right now.” It teaches us to sit with difficult feelings without judging them as “wrong” or trying to push them away immediately. The focus then shifts to changing behaviors and building skills to handle these intense emotions more effectively.
This difference is crucial. While CBT might help you challenge the thought “I’m a terrible person,” DBT might first validate that you’re in real pain, then teach you skills to tolerate that pain without acting destructively.
Treatment Structure and Duration
The way CBT and DBT are structured feels quite different when you’re actually in treatment.
| Feature | Cognitive Behavioral Therapy (CBT) | Dialectical Behavior Therapy (DBT) |
|---|---|---|
| Core Focus | Changing unhelpful thoughts and behaviors | Accepting emotions while building coping skills |
| Typical Duration | 5-20 sessions (short-term) | 6-12 months (long-term) |
| Session Structure | Weekly individual sessions | Individual therapy + group skills training + phone coaching |
| Key Techniques | Cognitive restructuring, behavioral experiments | Mindfulness, distress tolerance, emotion regulation, interpersonal skills |
CBT feels more like a focused workshop. You typically meet with your therapist weekly for individual sessions that are highly goal-oriented and structured. Most people complete CBT in 5-20 sessions, making it a relatively short-term commitment. Each session has clear objectives, and you’ll often have homework assignments to practice new skills between sessions.
DBT is more like enrolling in a comprehensive program. It’s a multi-component approach that includes individual therapy sessions, group skills training (where you learn alongside others), and even phone coaching for crisis situations. The treatment typically lasts 6-12 months or longer, recognizing that building emotional regulation skills takes time and practice.
The Role of the Therapeutic Relationship
The relationship between you and your therapist also feels different in each approach.
In CBT, your therapist acts like a collaborative partner or teacher. Together, you work as a team to identify problems, set goals, and develop strategies. The relationship is warm and supportive, but the focus remains primarily on the techniques and skills being learned. Your therapist guides you through exercises and helps you practice new ways of thinking and behaving.
In DBT, the therapeutic relationship is central to the healing process. Your therapist serves as both a coach and an ally, with validation being a cornerstone of every interaction. This means your therapist consistently acknowledges your emotions and experiences as understandable, even when working toward change. The importance of the therapeutic relationship cannot be overstated in DBT – it’s often through this validating relationship that people learn to validate themselves and build healthier connections with others.
Understanding these key differences helps explain why certain people might gravitate toward one approach over the other, depending on their specific needs and circumstances.