Mindfulness, Emotions, and More: Your Guide to Dialectical Behavior Therapy Components

Understanding the Core Components of Dialectical Behavior Therapy
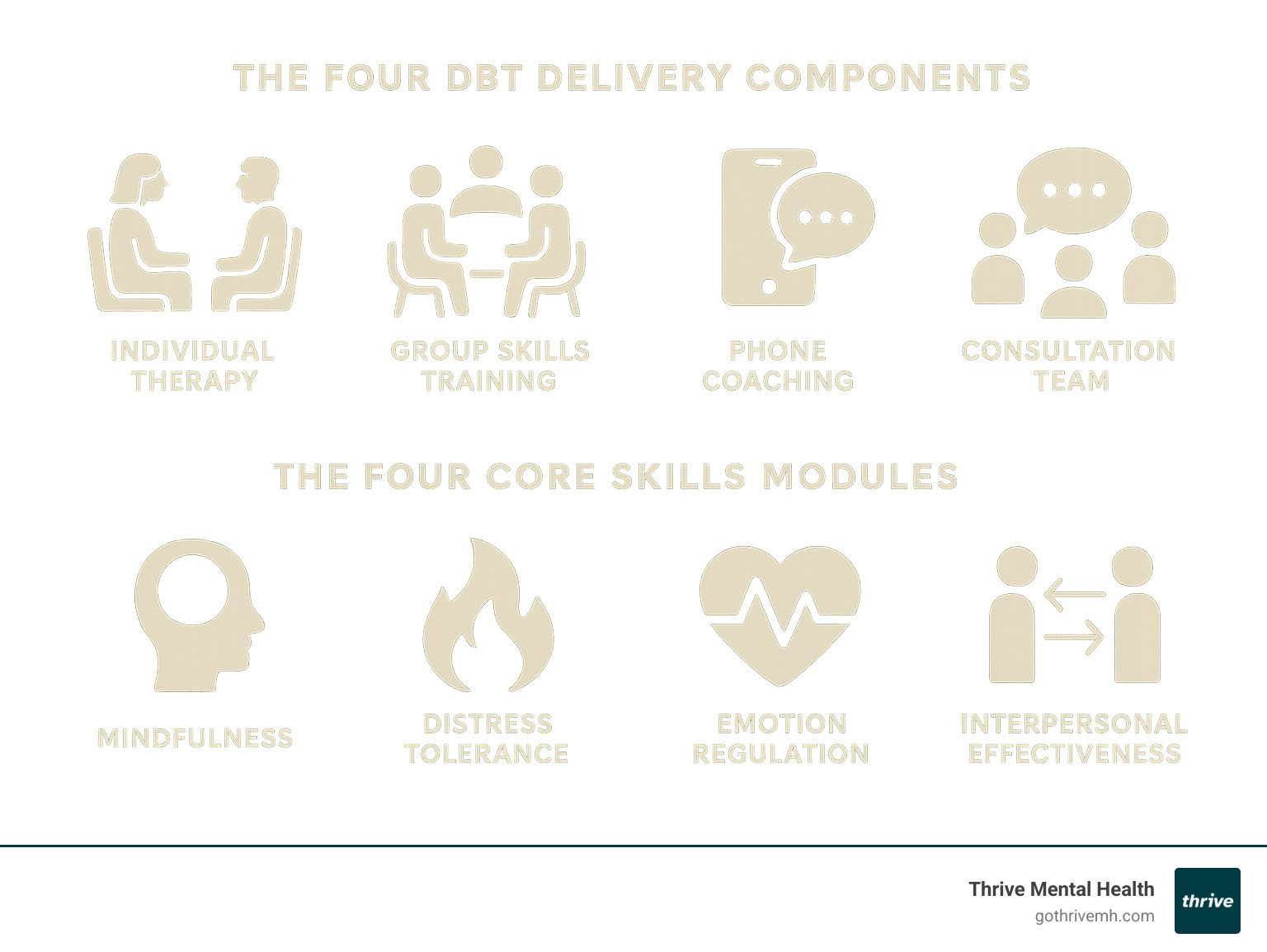
Dialectical behavior therapy components create a comprehensive treatment that helps people manage intense emotions and build healthier relationships. DBT combines four delivery methods with four core skill modules to create lasting change.
DBT Delivery Components:
- Individual therapy: Weekly one-on-one sessions.
- Group skills training: Weekly classes teaching practical coping skills.
- Phone coaching: In-the-moment support for crisis situations.
- Consultation team: A support system for therapists to ensure quality.
Core Skills Modules:
- Mindfulness: Staying present and aware.
- Distress tolerance: Managing crises without harmful behaviors.
- Emotion regulation: Understanding and changing intense emotions.
- Interpersonal effectiveness: Building and maintaining healthy relationships.
Originally developed by Dr. Marsha Linehan for borderline personality disorder, DBT is now used for depression, anxiety, eating disorders, and substance use. It uniquely balances acceptance of your current situation with change strategies to build a better life.
Research shows DBT significantly reduces suicide attempts, self-harm, and hospitalizations. A landmark study found 77% of participants no longer met the criteria for BPD after one year of treatment.
As CEO of Thrive Mental Health, I’ve seen these dialectical behavior therapy components transform lives. DBT’s structured, evidence-based approach provides the tools for emotional wellness and addresses the complex needs of those struggling with intense emotions.
The Core Dialectical Behavior Therapy Components: A Four-Part Structure
DBT is delivered through four interconnected parts that work together to provide a complete framework for support and growth. Each component serves a unique purpose, reinforcing the others to give you multiple touchpoints for learning.
-
Individual therapy: This is the foundation of your DBT experience. In weekly one-hour sessions, you and your therapist will address your personal challenges and goals. The focus is prioritized: first on life-threatening behaviors, then on therapy-interfering behaviors, and finally on improving your quality of life. It’s also where you apply the skills learned in group to your real-world situations.
-
Group skills training: These weekly 1.5 to 2.5-hour sessions function more like a class than traditional therapy. Alongside peers who understand your struggles, you will learn the four core DBT skills modules. This shared experience is powerful, as you both teach and learn from others.
-
Phone coaching: A unique feature of DBT, phone coaching provides in-the-moment support. When you’re in a crisis, you can contact your therapist to get coached through applying your skills right when you need them most.
-
Therapist consultation team: This component works behind the scenes. Your therapist meets regularly with other DBT clinicians to stay sharp, motivated, and true to the treatment model. This ensures you receive the best possible care because your therapist has their own support system.
The standard treatment schedule involves weekly individual and group sessions, with phone coaching available between appointments. This consistent structure provides multiple opportunities each week to practice and get support.
The Four Core Skills Modules of DBT
Within this structure, you’ll master four essential life skills. These are practical tools you can use daily to manage emotions, improve relationships, and build the life you want.
- Mindfulness teaches you to be present and aware without being swept away by thoughts and feelings.
- Distress tolerance gives you ways to survive crisis moments without making things worse.
- Emotion regulation helps you understand and change intense, overwhelming emotions.
- Interpersonal effectiveness shows you how to ask for what you need, say no, and maintain healthy relationships.
Understanding the Mindfulness Component
Mindfulness is the foundation of DBT. It’s about paying attention to the present moment without judgment. DBT divides mindfulness into “what” skills (what you do) and “how” skills (the attitude you bring).
- “What” Skills: Observe thoughts and feelings without getting attached; Describe your experience with facts, not interpretations; Participate fully in the current moment.
- “How” Skills: Be non-judgmental of your experience; Be one-mindful by focusing on one thing at a time; Be effective by doing what works, not what you think is “right.”
These skills build the self-awareness necessary for change. For more information, see this overview of mindfulness in DBT.
Exploring the Distress Tolerance Component
Distress tolerance skills help you survive tough moments when the situation can’t be immediately fixed. The goal is to get through a crisis without resorting to behaviors that cause more problems later.
- Radical Acceptance: This means accepting reality as it is, without approval. It’s about acknowledging what’s true so you can respond wisely instead of fighting an unwinnable battle.
- TIPP Skills: These techniques quickly calm your nervous system. Temperature (splashing cold water on your face), Intense exercise, Paced breathing, and Paired muscle relaxation.
- Self-Soothing: Comfort yourself by engaging your five senses: listen to calming music, look at beautiful art, taste something delicious, smell a favorite scent, or take a warm bath.
Breaking Down the Emotion Regulation Component
This module helps you understand your emotions, reduce your vulnerability to them, and change them when needed.
- Identify and Label Emotions: Learning to name what you’re feeling with precision gives you more control.
- Reduce Emotional Vulnerability (PLEASE Skills): Take care of your physical health to build emotional stability. Treat Physical iLlness, balance Eating, Avoid mood-altering drugs, get enough Sleep, and Exercise.
- Increase Positive Emotions: Actively schedule enjoyable activities to build emotional reserves.
- Change Unwanted Emotions: Use strategies like Opposite Action, where you act opposite to what your emotion tells you to do (e.g., approaching something you fear instead of avoiding it).
Mastering the Interpersonal Effectiveness Component
These skills help you steer relationships with more skill and less conflict, allowing you to ask for what you need while maintaining self-respect.
- DEAR MAN: A skill for getting what you want effectively. Describe the situation, Express your feelings, Assert your needs, Reinforce the outcome. Stay Mindful, Appear confident, and be willing to Negotiate.
- GIVE: A skill for maintaining the relationship during a conversation. Be Gentle, act Interested, Validate the other person’s feelings, and use an Easy manner.
These skills help you build genuine connections while honoring your needs and the needs of others.
The Philosophy Behind DBT: Acceptance and Change

At the heart of all dialectical behavior therapy components is a core philosophy: the balance between acceptance and change. The term “dialectical” refers to synthesizing two opposites. In DBT, this means you can accept yourself exactly as you are right now and simultaneously work to change your behaviors and build a better life.
This approach helps you move away from rigid, all-or-nothing thinking. Instead of self-criticism, you learn to honor where you are while gently moving toward your goals. Validation strategies are key to this process. Your therapist will validate your feelings and experiences, recognizing that your behaviors make sense given your history. This non-judgmental understanding creates the safety needed for change to occur.
The History and Development of DBT
DBT was developed in the 1970s by Dr. Marsha Linehan while working with chronically suicidal individuals, many with borderline personality disorder. She found that traditional cognitive behavioral therapy, with its sole focus on change, was invalidating for her clients and led to high dropout rates.
Dr. Linehan redesigned the treatment, incorporating her own insights and client feedback. She integrated mindfulness practices from contemplative traditions and emphasized the need for validation and acceptance alongside change strategies. Her personal experiences and scientific rigor created a approach. You can learn more about Dr. Marsha Linehan’s work and its ongoing impact.
The Biosocial Theory: Understanding Emotional Dysregulation
DBT uses the biosocial theory to explain why some people struggle with intense emotions. This theory removes blame by showing how emotional difficulties develop from a transaction between two factors:
- Biological Vulnerability: Being born with a more sensitive emotional system, meaning you feel things more and take longer to return to baseline.
- An Invalidating Environment: Growing up in an environment where your emotional responses were consistently dismissed, punished, or criticized.
When your natural emotional expressions are invalidated, you don’t learn how to manage them effectively. This understanding is freeing and informs the treatment, which focuses on validating your experience while teaching you the skills you never learned.
The Role of the DBT Therapist and Consultation Team
The therapeutic relationship in DBT is collaborative and supportive. Your therapist acts as an ally, balancing validation of your struggles with gentle challenges to try new behaviors. They are your coach in building a life worth living.
Crucially, your therapist is not alone. The consultation team is a vital component where your therapist meets regularly with other DBT clinicians. This team prevents therapist burnout, ensures treatment fidelity by keeping the therapy consistent with its principles, and helps your therapist maintain compassion and effectiveness. At Thrive Mental Health, this team approach ensures you receive the highest quality of care from a supported, motivated clinician.
Who Benefits from DBT and How Effective Is It?

DBT was originally developed for individuals with Borderline Personality Disorder (BPD), particularly those struggling with chronic suicidal thoughts and self-harm. It remains the gold-standard treatment for BPD. However, the dialectical behavior therapy components have proven effective for a wide range of issues rooted in emotional dysregulation.
At Thrive Mental Health, we see how DBT helps people with various diagnoses who share a common goal: to stop feeling overwhelmed by their emotions and build better relationships.
Conditions Effectively Treated with DBT
DBT’s focus on fundamental skills—managing emotions, tolerating distress, and effective communication—makes it broadly applicable.
- Post-Traumatic Stress Disorder (PTSD): Distress tolerance skills help manage flashbacks, while emotion regulation techniques address the intense fear and anger associated with trauma.
- Substance Use Disorders: DBT provides tools to manage cravings, cope with triggers, and build a life that doesn’t rely on substances for emotional relief.
- Eating Disorders: For conditions like binge eating and bulimia, DBT helps individuals identify and cope with underlying emotions, reducing the urge to use food for regulation. One study showed 86% of participants with binge-eating disorder stopped bingeing after 20 weeks of DBT.
- Depression: For treatment-resistant depression, DBT’s focus on building a “life worth living” helps create meaning and joy beyond just symptom reduction.
- Bipolar Disorder: Emotion regulation skills help manage mood swings and reduce impulsive behaviors, complementing medication.
- Anxiety: Mindfulness skills help ground individuals in the present, while distress tolerance provides tools for managing panic attacks.
The Evidence for DBT’s Effectiveness
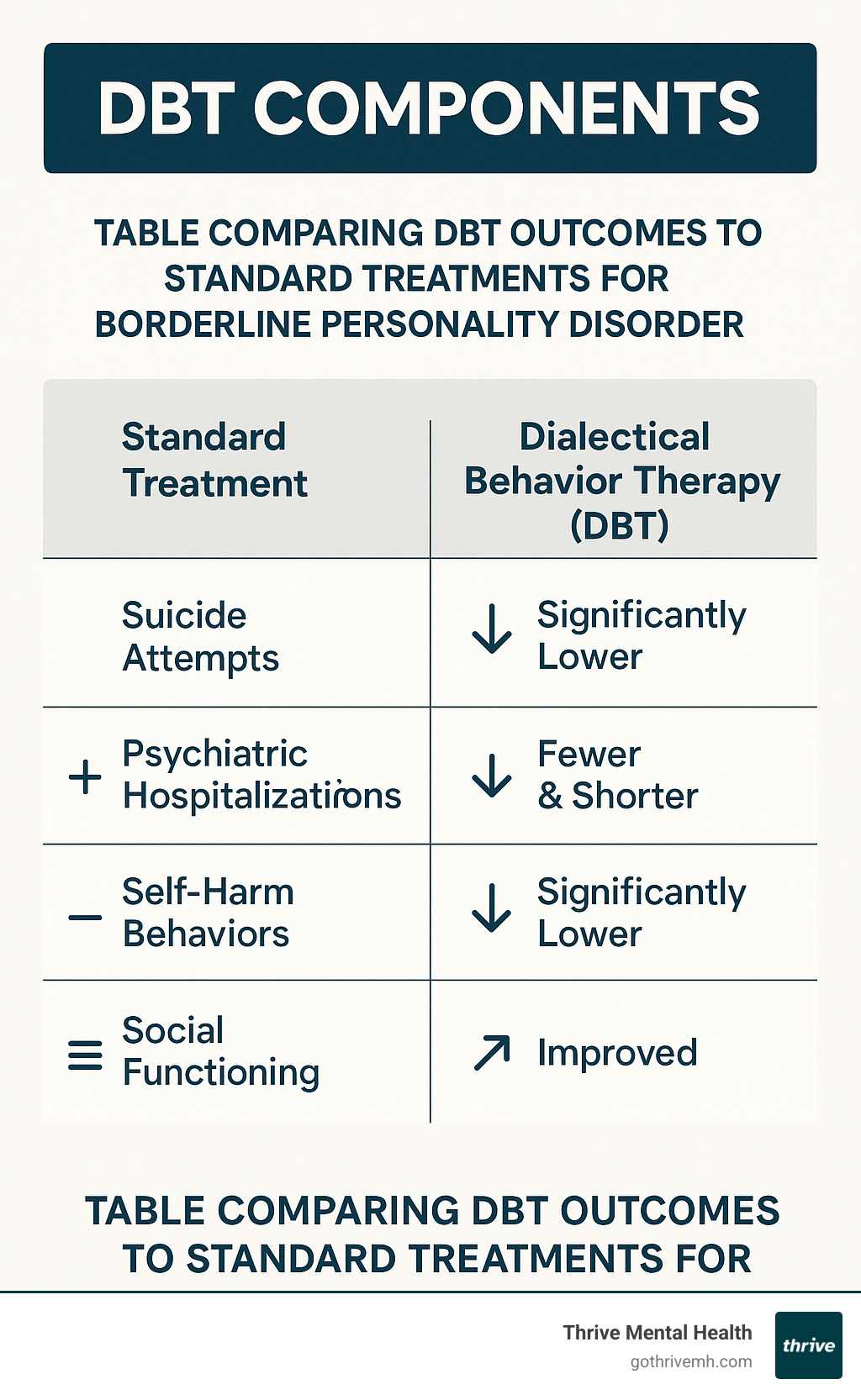
Numerous randomized controlled trials have proven DBT’s effectiveness. The results are consistently life-changing.
A groundbreaking 1991 study and a larger 2006 replication study showed that compared to standard treatment, individuals receiving DBT had:
- Significantly fewer suicide attempts.
- Fewer emergency room visits and psychiatric hospitalizations.
- Reduced anger and impulsive behavior.
- Improved social and overall functioning.
These benefits were shown to hold strong even a year after treatment ended. One of the most encouraging findings is that many participants achieve behavioral control—stopping life-threatening behaviors—within the first four to eight months of comprehensive DBT. The evidence is clear: DBT doesn’t just reduce symptoms; it helps people build satisfying lives.
How DBT Compares to Cognitive Behavioral Therapy (CBT)

Many people wonder about the difference between DBT and Cognitive Behavioral Therapy (CBT). Dialectical behavior therapy components actually evolved from CBT, so they share common ground. Both are evidence-based talk therapies focused on the connection between thoughts, feelings, and behaviors, and both provide practical strategies for change.
Think of CBT as the parent therapy from which DBT grew, developing its own unique features. While CBT focuses primarily on changing unhelpful thoughts and behaviors, DBT adds a crucial layer of acceptance.
Core Differences in Focus and Strategy
The key distinctions lie in DBT’s unique approach and structure:
- Emphasis on Acceptance: DBT’s core dialectic is balancing acceptance and change. Before changing difficult emotions, you first learn to accept and tolerate them. This is especially helpful for those with intense emotional sensitivity.
- Focus on Emotion Regulation: DBT places a heavy emphasis on emotional skills, with an entire curriculum dedicated to understanding, experiencing, and managing intense feelings.
- The Dialectical Component: DBT teaches clients to move away from black-and-white thinking and synthesize opposites (e.g., acceptance and change), a concept not central to traditional CBT.
- The Therapeutic Relationship: The DBT therapist often acts as a coach, creating a collaborative and validating relationship that balances warmth with challenging the client to grow.
- Treatment Structure: Standard CBT is often limited to weekly individual sessions. Comprehensive DBT is more intensive, including individual therapy, group skills training, and phone coaching to provide a robust support system.
For more context on traditional cognitive approaches, you can read more on cognitive behavior therapy. While CBT helps you change your thinking, DBT teaches you to manage your emotions and build a life, especially when those emotions feel overwhelming.
Frequently Asked Questions about DBT Components
Here are answers to some of the most common questions we receive about the practical aspects of dialectical behavior therapy components.
How long does standard DBT treatment typically last?
DBT is a commitment, as it works to change long-standing patterns. Standard comprehensive DBT typically lasts six months to a year, sometimes longer, depending on individual needs. This includes weekly individual therapy (about an hour) and weekly group skills training (1.5 to 2.5 hours).
The full skills curriculum takes about 24 weeks to complete, and many programs repeat it to ensure the skills become second nature. You also have phone coaching availability for in-the-moment support. While the program is long-term, many people achieve behavioral control (a significant reduction in life-threatening behaviors) within four to eight months.
What is a “diary card” in DBT?
A diary card is a daily tracking tool, like an emotional weather report. Each day, you spend a few minutes recording key information:
- Urges and Target Behaviors: Any urges you felt (e.g., to self-harm) and whether you acted on them.
- Emotion Intensity: Rating your emotions (like anger, sadness, joy) on a scale.
- Skills Used: Which DBT skills you practiced and how helpful they were.
This card is not busy work; it becomes the roadmap for your individual therapy sessions. It helps you and your therapist identify patterns, triggers, and progress, and it sets the agenda for each week’s session.
Can DBT be done online or in an intensive outpatient program?
Yes. DBT has adapted to modern needs and is highly effective when delivered online or through structured programs. DBT is frequently offered via telehealth and in Intensive Outpatient Programs (IOP) and Partial Hospitalization Programs (PHP).
At Thrive Mental Health, our flexible IOP and PHP programs are designed to deliver comprehensive DBT in formats that fit your life, both virtually and in-person. Research shows that online DBT can improve attendance and produce results comparable to in-person treatment, as long as treatment fidelity (adherence to the model) is maintained.
This flexibility increases accessibility, allowing you to receive life-changing care without the logistical challenges of traditional appointments. You can access expert-led dialectical behavior therapy components from wherever you are. Learn more about our flexible IOP and PHP programs to see how we can support you.
Start Your Journey with DBT Today
Understanding the dialectical behavior therapy components is the first step toward emotional freedom. DBT is a comprehensive, evidence-based treatment that has transformed lives by teaching practical skills for managing intense emotions and building meaningful relationships.
You learn mindfulness to stay grounded, distress tolerance to steer crises, emotion regulation to manage feelings, and interpersonal effectiveness to build healthy connections. These are real tools for daily life.
Research consistently shows that DBT works, reducing self-harm and hospitalizations while improving overall well-being. It offers genuine hope, especially if you feel overwhelmed by your emotions, struggle in relationships, or feel stuck in unhelpful behaviors.
At Thrive Mental Health, we know that traditional therapy schedules don’t work for everyone. Our virtual and in-person IOP and PHP programs are designed to be as flexible as they are effective, bringing expert-led DBT care to you.
Building the life you want is possible, and learning new skills is a sign of wisdom, not weakness. Ready to take the first step? Learn more about our flexible IOP and PHP programs and find how DBT can help you build the resilient, fulfilling life you deserve.