Group Therapy and Beyond: Effective Suicide Prevention Strategies

Why Evidence-Based Suicide Prevention is Critical for Saving Lives
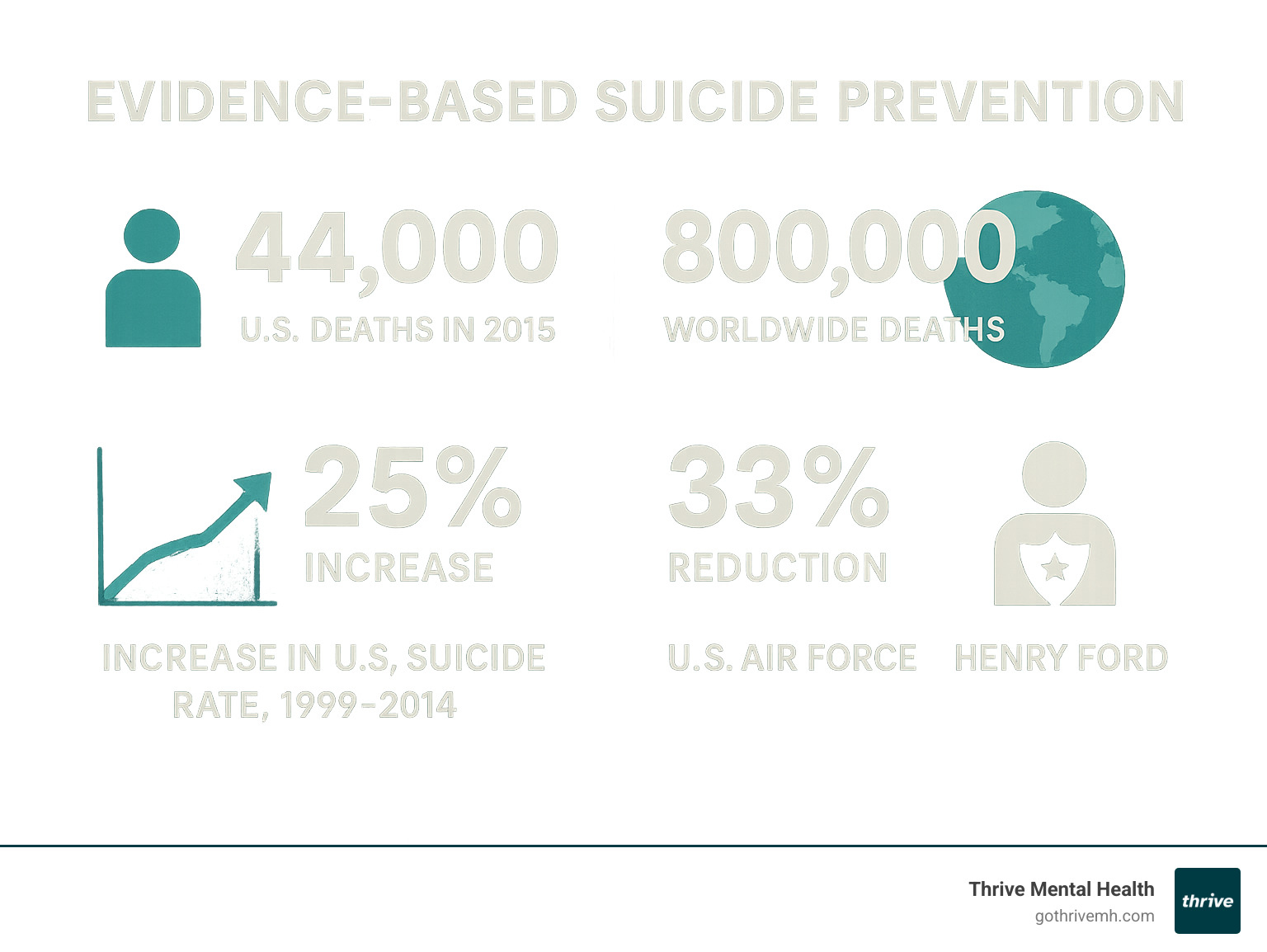
Evidence-based suicide prevention represents our most powerful weapon against a growing public health crisis. With over 44,000 deaths by suicide occurring in the US in 2015 and 800,000 worldwide, we’ve seen a devastating 25% increase in suicide rates between 1999 and 2014. Yet there’s hope – research shows that suicide is preventable when we apply proven, science-backed strategies.
Key Evidence-Based Suicide Prevention Strategies:
- Universal Prevention: Population-wide mental health promotion and stigma reduction
- Selective Prevention: Targeted support for high-risk groups through gatekeeper training
- Indicated Prevention: Clinical interventions for individuals showing warning signs
- Zero Suicide Framework: Comprehensive healthcare system approach with 7 core elements
- Clinical Tools: Validated assessment instruments like C-SSRS and SAFE-T
- Brief Interventions: Safety planning, lethal means counseling, and consistent follow-up
- Evidence-Based Treatments: CBT-SP, DBT, and CAMS therapies that directly target suicidal thoughts
The shift from guesswork to proven strategies has already shown remarkable results. The U.S. Air Force’s comprehensive program achieved a 33% reduction in suicide deaths, while Henry Ford Health System reduced their suicide rate by 75% through systematic implementation of evidence-based practices.
This isn’t just about individual interventions – it’s about creating layered systems of support that catch people at every level of risk. From community-wide awareness campaigns to intensive clinical care, evidence-based suicide prevention requires a coordinated approach that addresses the complexity of suicidal behavior.
As CEO of Thrive Mental Health, I’ve witnessed how evidence-based suicide prevention strategies can transform lives when integrated into comprehensive treatment programs. My experience leading behavioral health innovation has shown me that combining clinical excellence with accessible, flexible care delivery creates the foundation for sustainable recovery and hope.
Basic evidence-based suicide prevention terms:
A Public Health Approach: Layering Strategies for Maximum Impact
Effective suicide prevention works like overlapping safety nets. By combining population-wide efforts with targeted support and crisis care, we catch people at every level of risk.
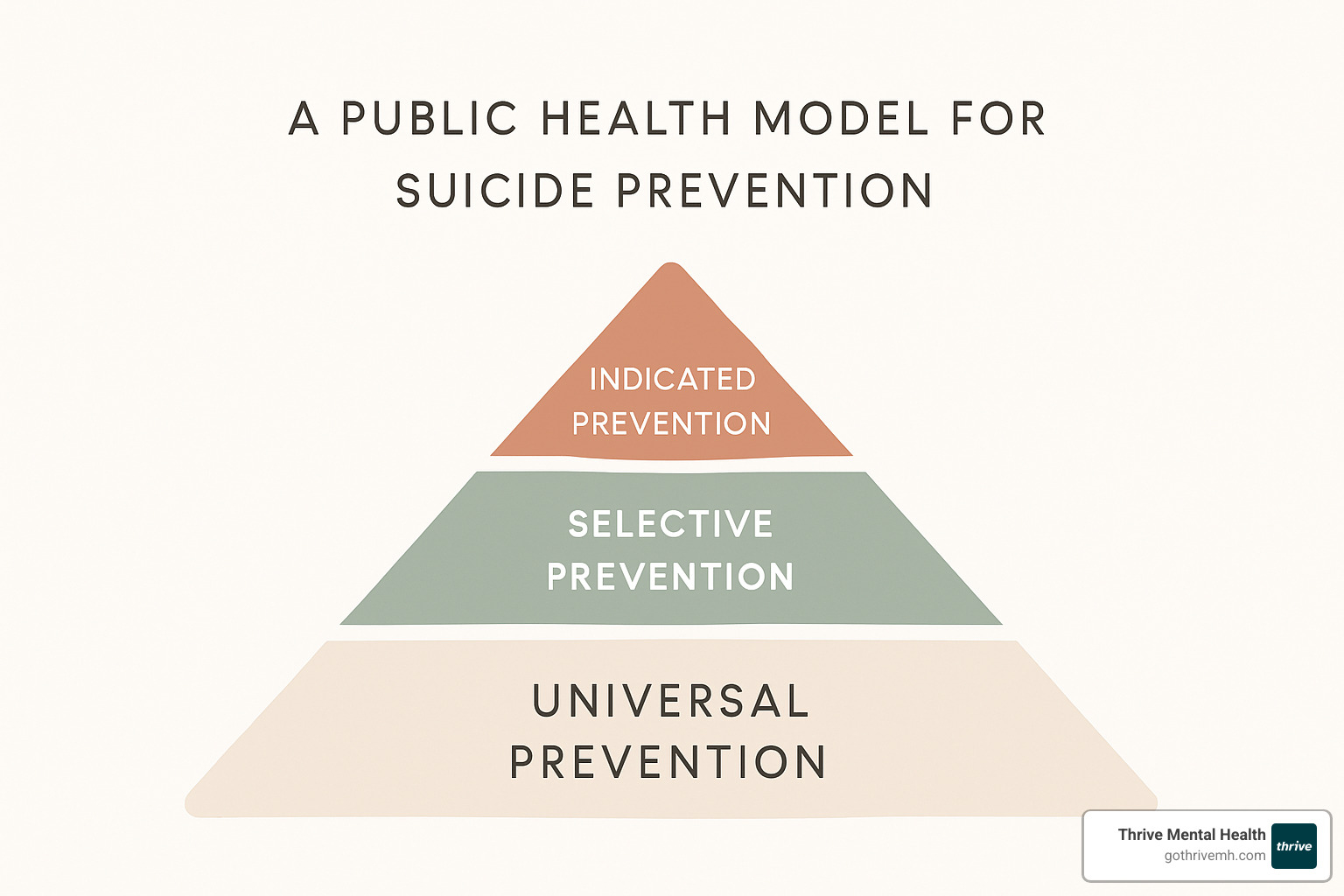
Universal Strategies: Promoting Mental Wellness for All
Universal prevention casts the widest net—reducing stigma, improving mental-health literacy, and strengthening protective factors in schools, workplaces and online campaigns. Programs like Signs of Suicide (SOS) and public initiatives such as #ShareHope show that sustained, positive messaging can lower suicidal ideation across entire communities.
Selective Strategies: Supporting At-Risk Groups
Selective prevention focuses on groups with liftd risk—veterans, LGBTQ+ youth, older adults, and people with trauma histories. Gatekeeper trainings such as QPR and ASIST equip teachers, healthcare staff, first-responders and community leaders to recognize warning signs and connect individuals to help. Research indicates that most trainees report higher confidence and change their clinical or community practices after training.
Indicated Strategies: Intervening for Individuals in Crisis
Indicated prevention is rapid, clinically driven care for people already showing suicidal thoughts or behaviors. Early identification matters: about half of those who die by suicide do so on their first attempt. Comprehensive risk assessment, personalized safety planning, and evidence-based therapies delivered through programs like Thrive’s IOP and PHP create the intensive support needed to move from crisis to recovery.
The Zero Suicide Framework: A System-Wide Commitment to Saving Lives
Zero Suicide is an aspirational yet practical roadmap for health systems: make suicide deaths never events by embedding prevention into every patient touchpoint.
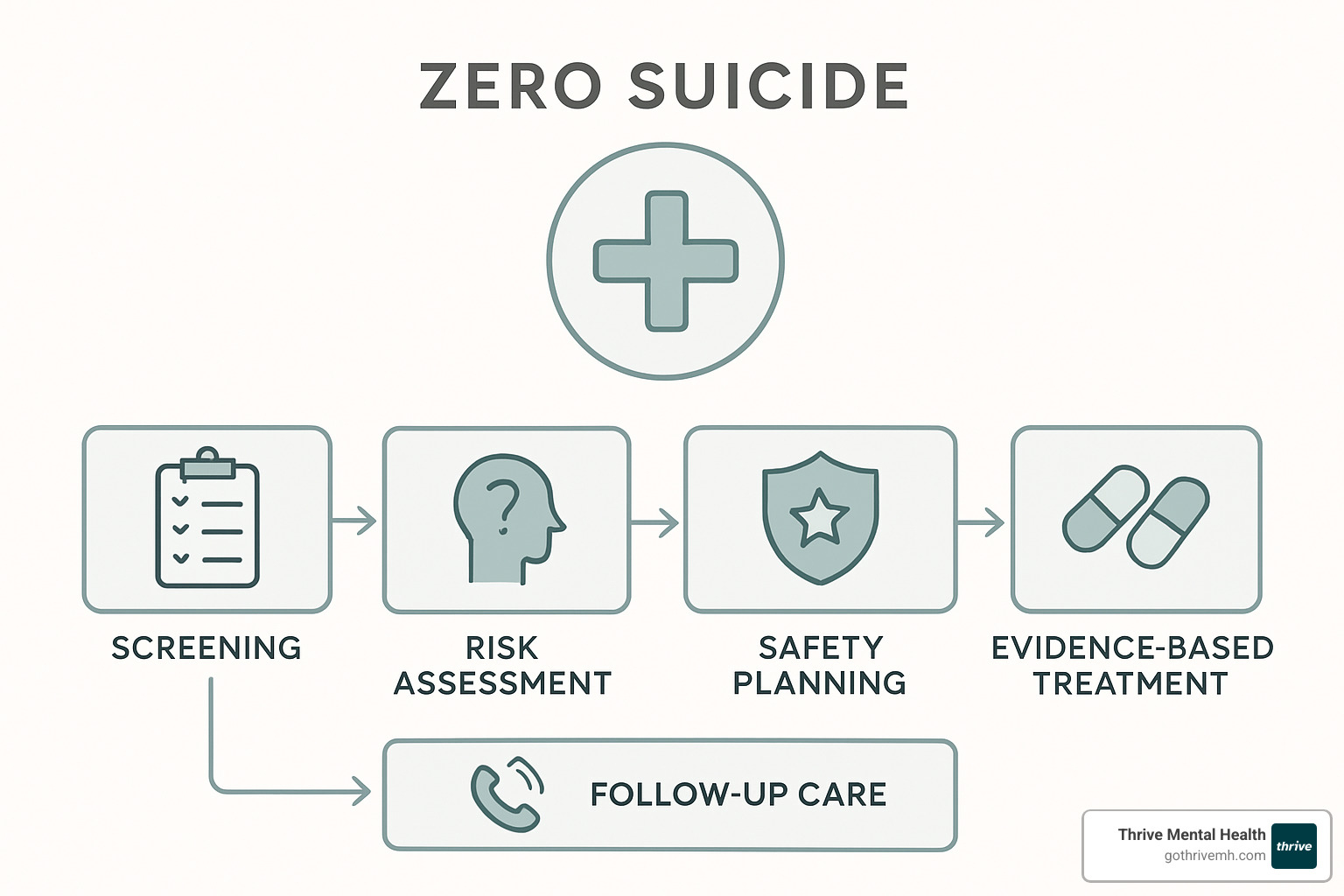
The 7 Elements of a Zero Suicide System
- Lead – visible, accountable leadership
- Train – role-specific education for all staff
- Identify – routine, systematic screening
- Engage – collaborative, person-centered care
- Treat – suicide-specific, evidence-based therapies
- Transition – safe handoffs between levels of care
- Improve – continuous quality improvement
Health systems that fully implement these steps, like Henry Ford and Centerstone, have cut suicide rates 65–75%.
Why Comprehensive Training Matters
Training closes the confidence gap: up to one in five clinicians still avoid asking about suicide. Ongoing, skills-based education—risk assessment, safety planning, documentation—turns discomfort into competence and drives system-wide policy change.
The Clinical Toolkit for Evidence-Based Suicide Prevention

Suicide-specific care follows three essential steps.
Step 1: Precise Assessment
• C-SSRS and SAFE-T quickly differentiate passive thoughts from active intent.
• AIM-SP expands assessment into a 10-step cycle of screening, formulation and monitoring.
Step 2: Targeted Treatments
• CBT-SP challenges hopeless thinking and rehearses alternative coping.
• DBT teaches emotion-regulation, distress-tolerance and interpersonal skills.
• CAMS turns the assessment itself into a collaborative treatment plan.
These therapies consistently outperform general mental-health care for reducing attempts and deaths.
Step 3: Brief, High-Impact Interventions
• Safety Planning turns vague advice into a six-step action plan the person can follow in moments of crisis.
• Lethal Means Counseling buys time by locking, removing or otherwise restricting access to firearms, medications and other means.
• Caring Contacts—short texts, emails or letters—maintain connection during vulnerable periods and are proven to lower repeat attempts.
Immediate Help: Resources for Crisis and Support
When someone is in crisis, knowing where to turn can literally save a life. The most important thing to remember is that you are not alone – help is available right now, and reaching out shows incredible courage and strength.

Crisis situations can feel overwhelming, but having immediate access to professional support can make all the difference. These resources use evidence-based suicide prevention techniques and are staffed by trained professionals who understand exactly how to help.
If You or Someone You Know is in Crisis
The 988 Suicide & Crisis Lifeline has transformed crisis support by making help as simple as remembering three numbers. Whether you call or text 988, you’ll connect with a trained crisis counselor who can provide immediate support, safety planning, and connection to local resources.
What makes this service so powerful is that it’s completely free, confidential, and available 24 hours a day, 365 days a year. Connect with a trained crisis counselor 24/7 – these aren’t just volunteers, but professionally trained individuals who understand crisis intervention and can provide real, practical help.
For people who feel more comfortable texting, the Crisis Text Line offers another lifeline. Simply text HOME to 741741 to reach a trained crisis counselor via text message. This can be especially helpful for young people who may find texting less intimidating than a phone call.
When someone is in immediate danger, don’t hesitate to call 911 or go directly to your nearest emergency department. Emergency services are equipped to handle psychiatric emergencies and can provide immediate safety assessment and stabilization.
How to Support a Person at Risk
Supporting someone who might be thinking about suicide requires specific skills, but you don’t need to be a mental health professional to make a difference. Your caring presence and willingness to help can be life-saving.
Ask directly about suicide using clear, straightforward language. Questions like “Are you thinking about suicide?” or “Are you thinking about killing yourself?” might feel scary to ask, but they’re crucial. Asking about suicide doesn’t plant the idea or increase risk – it shows you care enough to have a difficult conversation.
Listen without judgment and resist the urge to immediately try to fix or minimize their experience. Sometimes the most powerful thing you can do is simply be present and allow them to express their feelings. Avoid phrases like “you have so much to live for” or “things will get better” – instead, focus on understanding their pain.
Keep them safe by helping remove or restrict access to lethal means like firearms, medications, or other dangerous items. This isn’t about being controlling – it’s about reducing risk during a vulnerable time. Stay with them or ensure they’re with someone they trust until professional help is available.
Help them connect with professional support, whether that’s calling 988 together, contacting their therapist, or going to an emergency room. Don’t try to handle a crisis situation alone – professional help is essential.
Follow up regularly, especially during high-risk periods. A simple text checking in or a brief phone call can provide crucial connection and support. Consistent follow-up shows that you care and helps maintain the relationship that can be protective against suicide.
Being a supportive friend or family member is incredibly important, but it doesn’t make you responsible for preventing someone’s suicide. Professional intervention is essential for individuals in crisis, and connecting them with appropriate resources is one of the most helpful things you can do.
Frequently Asked Questions about Suicide Prevention
What’s the difference between a safety plan and a “no-suicide contract”?
A safety plan is a practical, collaborative roadmap for surviving a crisis. A no-suicide contract is simply a promise not to die; it offers no skills, no support, and can damage trust. Evidence strongly favors safety planning.
Can suicide really be prevented?
Yes. Air-Force, Henry Ford, and Centerstone programs cut deaths by 33–75% through systematic screening, evidence-based treatment, and consistent follow-up.
How can programs be adapted for different cultures?
Start with community leadership, translate more than words, respect local beliefs, and pair evidence-based methods with peer support drawn from the culture itself.
Conclusion: Building a Future with Hope and Healing
When we look at the devastating statistics – 44,000 suicide deaths in the US, 800,000 worldwide – it’s easy to feel overwhelmed. But here’s what gives me hope: evidence-based suicide prevention isn’t just theory. It’s a proven path forward that’s already saving lives in communities around the world.
The Henry Ford Health System didn’t just reduce their suicide rate by 75% through luck. The U.S. Air Force didn’t achieve a 33% reduction by accident. These remarkable outcomes happened because dedicated people implemented the comprehensive strategies we’ve explored together – from universal prevention efforts that reach entire communities to intensive clinical interventions that target suicidal thoughts directly.
What makes this approach so powerful is how all the pieces work together. Community gatekeeper training creates the first line of support. Universal prevention efforts reduce stigma and build mental health literacy. When someone does reach crisis, validated assessment tools like the C-SSRS help clinicians understand exactly what’s happening. Evidence-based treatments like CBT-SP and DBT then provide the targeted interventions that can interrupt suicidal crises.
The Zero Suicide framework shows us that systemic change is possible when healthcare organizations commit fully to evidence-based suicide prevention. Those seven elements – Lead, Train, Identify, Engage, Treat, Transition, and Improve – create systems so comprehensive that suicide becomes increasingly rare rather than inevitable.
But systems alone aren’t enough. Clinical excellence matters enormously. When clinicians receive proper training in suicide-specific interventions, their confidence increases and their practice changes. When they use collaborative tools like safety planning instead of ineffective “no-suicide contracts,” patients feel empowered rather than restricted.
Community support amplifies everything else. When family members know how to ask directly about suicide, when friends understand the importance of following up, when crisis resources are accessible 24/7, the entire safety net becomes stronger.
At Thrive Mental Health, we’ve seen how integrating these evidence-based suicide prevention strategies into flexible, accessible care transforms lives. Our IOP and PHP programs combine the clinical excellence of evidence-based treatments with the accessibility that people need to actually get help. Because what good is the best treatment in the world if someone can’t access it when they need it most?
Recovery isn’t just possible – it’s happening every day. When someone learns to recognize their warning signs through safety planning, when they develop new coping skills through DBT, when they feel genuinely heard and supported through CAMS, they’re not just surviving crisis. They’re building resilience for the future.
The evidence is clear, the tools are proven, and the results are achievable. We don’t have to accept suicide as inevitable. We can create communities where people feel safe seeking help, healthcare systems that respond with expertise and compassion, and treatment programs that meet people exactly where they are.
Together, we’re building a future where hope isn’t just a nice idea – it’s the foundation of effective, life-saving care.
Learn more about our evidence-based mental health programs and find how comprehensive, flexible treatment can support your journey toward recovery and resilience.