Medicaid and Mental Health—Navigating Therapy Coverage Without Losing Your Mind

Navigating the Maze of Mental Health Coverage
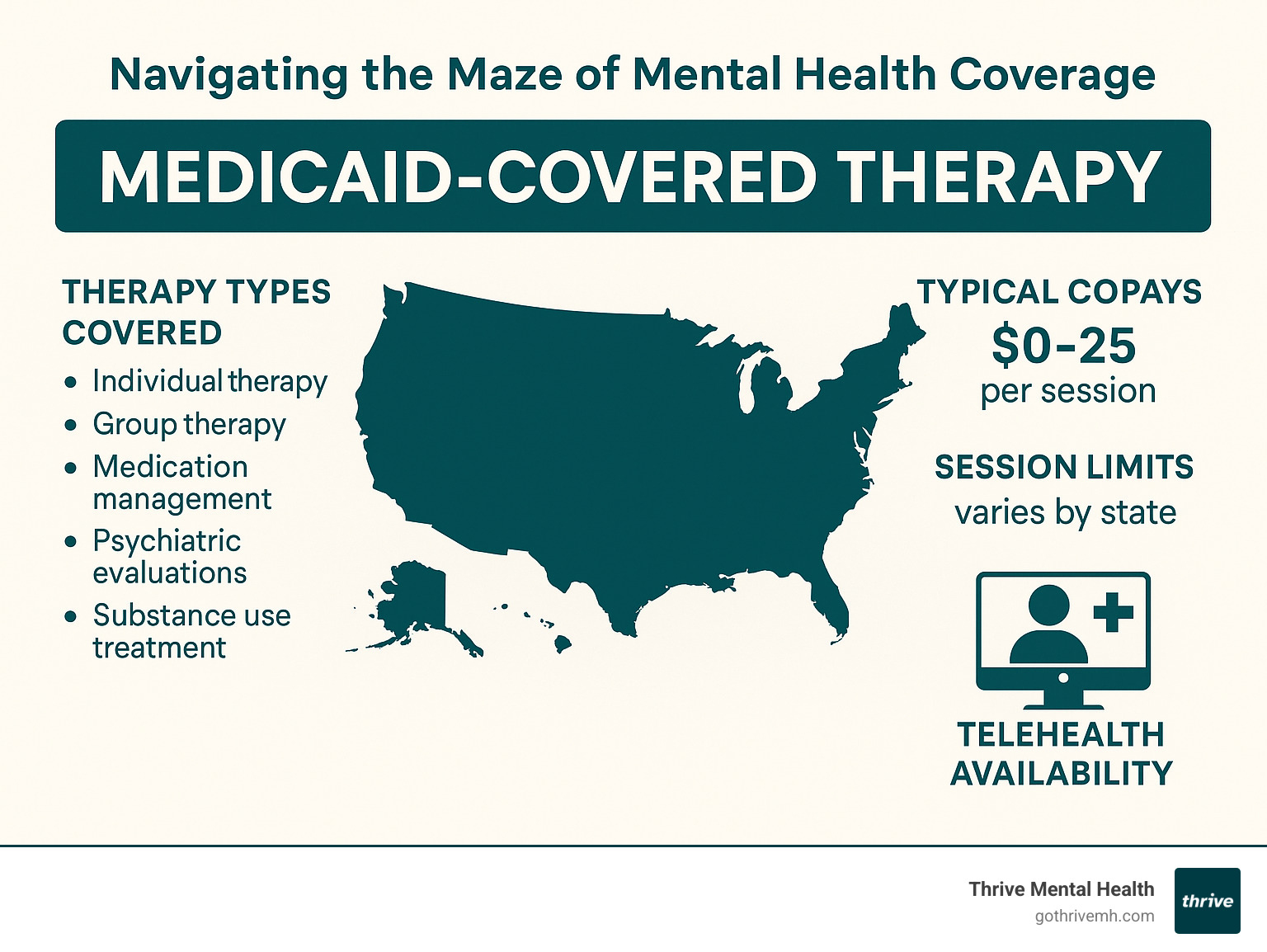
Medicaid covered therapy is available in all 50 states, providing essential mental health services to eligible low-income individuals. Here’s what you need to know:
- What’s covered: Individual therapy, group therapy, medication management, psychiatric evaluations, and substance use treatment
- Typical costs: $0-$25 copay per session (varies by state)
- Who qualifies: Low-income individuals, families, pregnant women, children, elderly, and people with disabilities
- Where to access: Community mental health centers, Federally Qualified Health Centers (FQHCs), and some private practices
Finding affordable mental health care shouldn’t feel impossible. Yet for millions of Americans, the cost of therapy remains a significant barrier to getting help. If you’re among the 85+ million people covered by Medicaid, you have access to mental health services that could be life-changing—if you know how to steer the system.
Medicaid is the single largest payer for mental health services in the United States. That’s good news. The challenging part? Coverage details vary significantly by state, provider, and specific plan.
I’m Nate Raine, CEO of Thrive Mental Health, where I’ve helped thousands of clients understand and maximize their Medicaid covered therapy benefits to access the care they deserve without financial strain. My experience working at the intersection of healthcare policy and mental health service delivery has shown me the critical gaps that exist between coverage on paper and actual access to care.
Medicaid 101: Who Qualifies and Why It Matters
Ever wonder how millions of Americans access mental health care when money is tight? The answer often lies in Medicaid – a lifeline for those who might otherwise fall through the healthcare cracks.
Established back in 1965, Medicaid serves as a partnership between federal and state governments to provide health coverage for people with limited income. Think of it as a safety net designed to catch those who might otherwise go without essential care.
As of June 2023, more than 85 million people were enrolled in Medicaid and the Children’s Health Insurance Program (CHIP). That’s more than one in four Americans!
Medicaid covered therapy matters tremendously because mental health challenges don’t check your bank account before they arrive. Anyone – regardless of income – can experience depression, anxiety, or other mental health conditions. Without insurance, therapy sessions typically cost $100-$200 each, placing regular mental health care out of reach for many families. And since mental health treatment often requires ongoing sessions rather than one-time visits, having continuous coverage becomes even more crucial.
The landscape of Medicaid has evolved significantly in recent years. The Affordable Care Act (ACA) expanded eligibility in many states, allowing more people to qualify based on income alone. Additionally, the Mental Health Parity and Addiction Equity Act (MHPAEA) requires Medicaid managed care plans to provide mental health benefits comparable to physical health benefits – a huge step forward in recognizing that mental health is health, period.
Key Eligibility Factors at a Glance
While Medicaid is a national program, states have considerable flexibility in how they implement it. This creates a patchwork of eligibility rules across the country. Generally speaking, your eligibility depends on several key factors:
Income thresholds serve as the primary qualification metric, usually based on the Federal Poverty Level (FPL). Your household size matters too – larger households can qualify at higher income levels. There’s also categorical eligibility with special provisions for children, pregnant women, parents, elderly individuals, and people with disabilities.
Most states require U.S. citizenship or qualified immigrant status, and you must be a resident of the state where you apply. It’s a local program in that sense – you can’t use New York Medicaid in California.
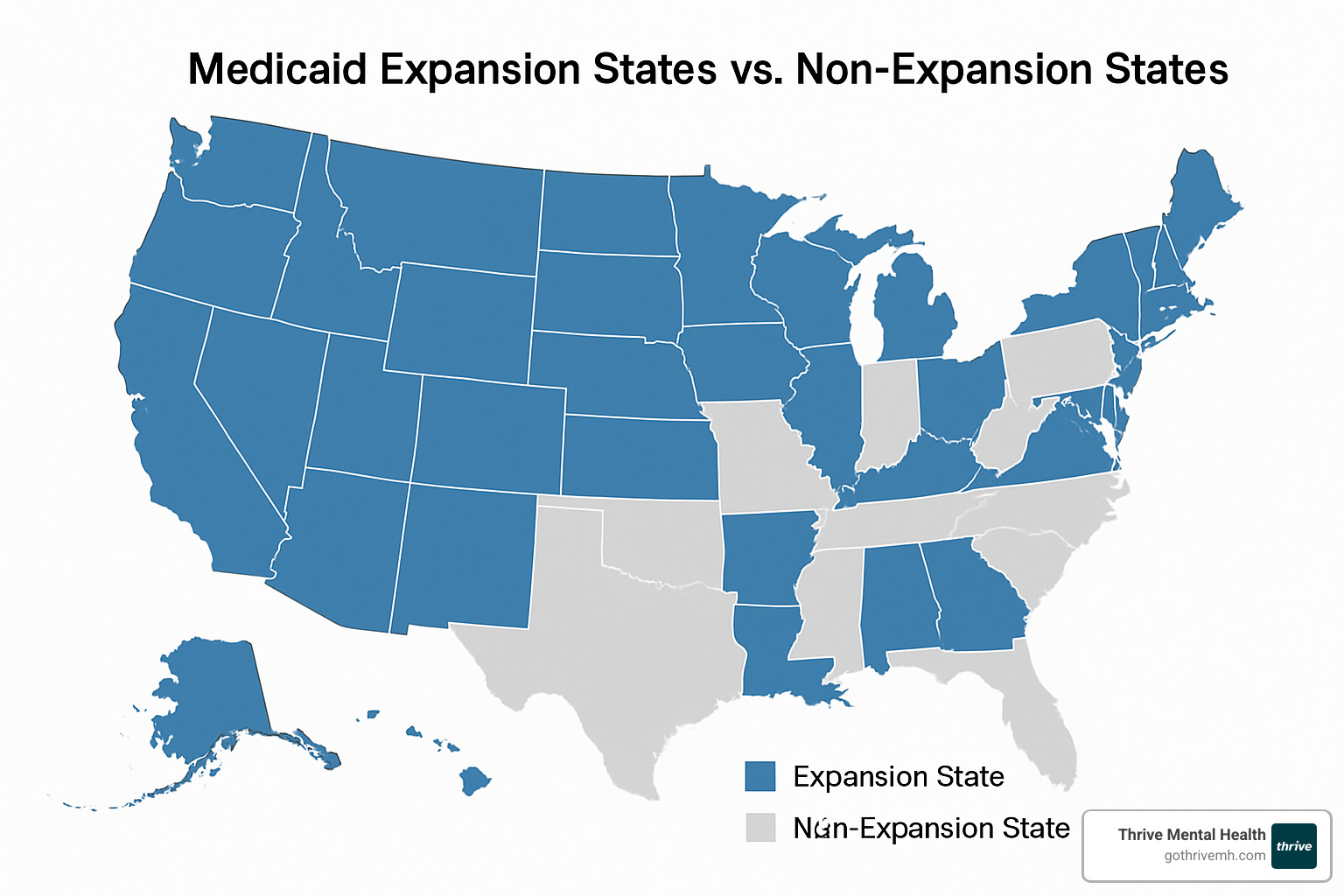
Perhaps the biggest difference in eligibility comes down to whether you live in an expansion or non-expansion state. In states that expanded Medicaid under the ACA (currently 41 states plus D.C.), adults with incomes up to 138% of the FPL can qualify regardless of parental or disability status. In non-expansion states, the criteria are typically much more restrictive.
Getting enrolled in Medicaid isn’t complicated, but it does require some paperwork. The process typically includes applying through your state Medicaid agency or Healthcare.gov, providing documentation of your income and residency, and waiting for a determination (usually within 45 days). If your state uses managed care plans, you’ll select one after approval. Medicaid requires annual recertification, and you should report any significant income or household changes to your state Medicaid office.
Life circumstances change – jobs come and go, families grow or shrink – and these changes can affect your Medicaid eligibility. That’s why staying in communication with your local Medicaid office about significant life changes is so important for maintaining continuous coverage.
According to recent research on Medicaid growth, enrollment has reached historic levels, underscoring just how essential this program has become for healthcare access in America.
Medicaid Covered Therapy: What’s Actually Included
When it comes to Medicaid covered therapy, there’s a silver lining for those struggling to afford mental health care. Every state Medicaid program must cover certain mental health and substance use disorder services. Thanks to the Mental Health Parity and Addiction Equity Act, these mental health benefits can’t be more restrictive than coverage for physical health conditions.
That said, the specific services available through your Medicaid plan might look different depending on which state you call home. Let me walk you through what you can generally count on:
Core Mental Health Services Every State Must Offer
I’ve worked with countless clients who were surprised to learn just how comprehensive Medicaid’s mental health coverage can be. While states have flexibility in their programs, certain services form the backbone of mental health coverage nationwide:
Individual therapy sessions give you one-on-one time with a licensed professional who can help you work through personal challenges. These sessions typically last 45-60 minutes and form the foundation of most treatment plans.
Psychiatric evaluations help determine what’s really going on and what might help. Think of these as the mental health equivalent of a thorough physical exam – they’re essential for accurate diagnosis and treatment.
Medication management appointments ensure any prescribed psychiatric medications are working properly without causing problematic side effects. These are usually shorter visits focused specifically on how your medications are working.
Crisis intervention services provide a safety net when things become overwhelming. These services can literally be lifesaving during mental health emergencies.
Inpatient psychiatric care offers round-the-clock support during acute mental health crises when safety is a concern or intensive treatment is needed.
Rehabilitation services help you recover or improve functioning after mental health setbacks, focusing on building skills for daily life.
Most states also cover group therapy (which can be incredibly powerful as you connect with others facing similar struggles), family therapy to address relationship dynamics, peer support services from people who’ve “been there,” and substance use disorder treatment for alcohol and drug issues.
Evidence-based therapies like Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and Eye Movement Desensitization and Reprocessing (EMDR) are typically covered when they’re considered medically necessary for your specific situation.
For children under 21, Medicaid goes even further with the Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) benefit, which provides comprehensive coverage for mental health services – even those not typically available to adults in that state.
Specialized Programs & Waivers for Medicaid Covered Therapy
Beyond basic services, many states offer specialized programs that provide improved mental health benefits. These can be game-changers for people who need more intensive support:
Intensive Outpatient Programs (IOP) provide structured support (typically 9-12 hours weekly) while allowing you to maintain your daily life. At Thrive Mental Health, we’ve seen how IOPs bridge the gap for people who need more than weekly therapy but don’t require 24-hour care.
Partial Hospitalization Programs (PHP) offer more intensive support than IOPs, usually involving 20+ hours weekly of structured treatment while still letting you return home each evening. These programs provide hospital-level care without overnight stays.
Home and Community-Based Services (HCBS) Waivers allow states to offer services beyond standard Medicaid benefits, helping people with mental health conditions live independently in their communities. These services might include skills training, supported employment, or peer support.
Habilitation Supports Waiver programs in some states provide specialized services for individuals with developmental disabilities that include mental health components.
Targeted Case Management helps coordinate care across multiple providers and systems, ensuring comprehensive treatment for complex mental health needs. Think of case managers as healthcare navigators who help you access all the services you need.
The availability of these specialized services varies significantly from one state to another. I always recommend checking with your state’s Medicaid office or managed care organization to understand exactly what’s available to you. Sometimes the most helpful programs aren’t the most widely advertised, so it’s worth asking specifically about services that might address your unique needs.
For a deeper dive into the full range of behavioral health services that might be available to you, check out our comprehensive guide to behavioral health services.
The Fine Print: Costs, Limits, and What Medicaid Won’t Pay For
While Medicaid covered therapy can be incredibly valuable, it’s important to understand the potential costs and limitations that might apply:
Costs
-
Copayments: While many states offer mental health services with no copay, some charge $0-$25 per session. These amounts are typically much lower than private insurance copays.
-
Deductibles: Most Medicaid plans don’t have deductibles for mental health services, meaning coverage begins immediately without having to pay a certain amount out-of-pocket first.
-
Premium payments: Some states charge small monthly premiums for certain Medicaid enrollees, though these are typically minimal and often waived for those with very low incomes.
Limits
-
Session caps: Some states limit the number of therapy sessions covered per year (often around 30 sessions), though exceptions can sometimes be made with proper documentation of medical necessity.
-
Prior authorization: Many states require providers to obtain approval before providing certain services, particularly for specialized or intensive treatments.
-
Provider networks: You’ll typically need to see providers who are in-network with Medicaid, which can sometimes limit your options.
What Medicaid Won’t Cover
Certain mental health services are typically not covered by Medicaid:
- Couples or marriage counseling: Unless directly related to an individual’s diagnosed mental health condition
- Career counseling or life coaching: These are generally considered non-medical services
- Alternative therapies: Services like hypnotherapy, art therapy, or music therapy may not be covered unless part of a comprehensive treatment plan
- Holistic treatments: Reiki, acupuncture, massage therapy, and similar services are typically excluded
- Experimental treatments: Therapies without established evidence bases are generally not covered
It’s worth noting that some states may cover certain services that others exclude, so always verify coverage with your specific Medicaid plan.
State-by-State Variations in Medicaid Covered Therapy
Perhaps the most challenging aspect of Medicaid covered therapy is the significant variation from state to state. These differences can include:
- Provider reimbursement rates: States with higher reimbursement rates typically have more providers willing to accept Medicaid
- Telehealth coverage: While the COVID-19 pandemic expanded telehealth coverage across all states, some have maintained more comprehensive telehealth benefits than others
- Specific therapy modalities covered: Some states cover a wider range of evidence-based therapies than others
- Service intensity and duration: Limits on session length, frequency, and total number can vary widely
- Provider qualifications: States differ in which types of mental health professionals can bill Medicaid
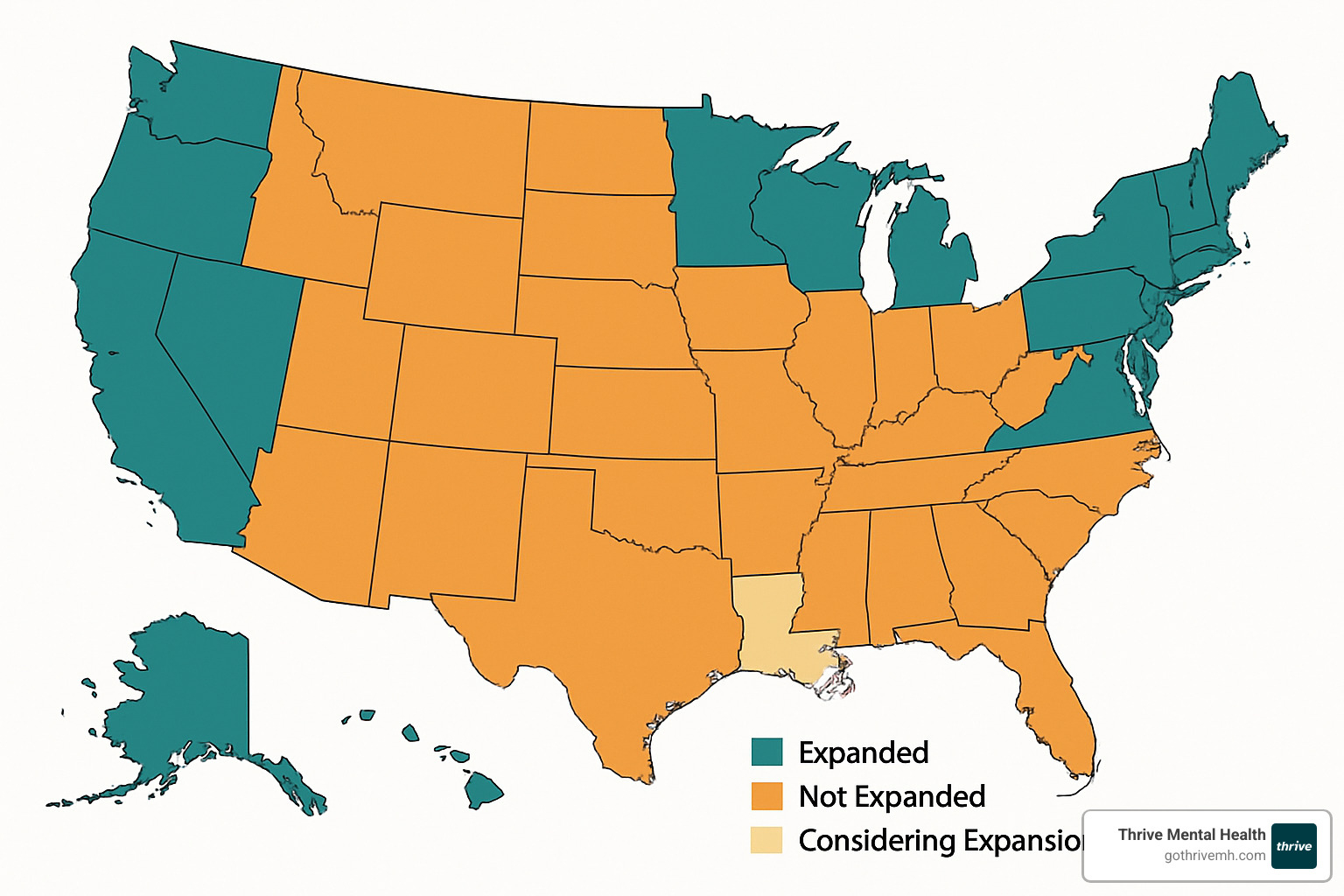
These variations mean that two people with identical mental health needs might have very different experiences accessing care depending on where they live. For example, someone in California might have access to unlimited therapy sessions and a wide range of providers, while someone in Mississippi might face stricter session limits and fewer provider options.
Comparing Medicaid to Private Insurance for Therapy
How does Medicaid covered therapy stack up against private insurance? Here’s a general comparison:
| Feature | Medicaid | Typical Private Insurance |
|---|---|---|
| Monthly Premium | $0-$25 (if any) | $300-$700+ |
| Therapy Copay | $0-$25 | $20-$50 |
| Deductible | Usually none | Often $1,000-$8,000 |
| Provider Network | More limited | Generally broader |
| Prior Authorization | Often required | Sometimes required |
| Session Limits | Varies by state | Often 20-30 per year |
| Telehealth Coverage | Varies by state | Increasingly comprehensive |
While private insurance may offer more provider options, Medicaid typically provides more affordable care with lower out-of-pocket costs. For many people with limited income, Medicaid makes therapy accessible when it would otherwise be financially out of reach.

How to Use Your Benefits: Finding a Therapist Who Accepts Medicaid
Finding a therapist who accepts Medicaid can feel like searching for a needle in a haystack, but don’t worry—I’ve helped hundreds of clients steer this exact challenge. The good news is that with the right approach, you can find quality mental health care through your Medicaid covered therapy benefits.
Many people don’t realize that your search strategy can make all the difference. Start with your state’s Medicaid provider directory—every state maintains an online database where you can search specifically for mental health providers. If you’re enrolled in a Medicaid managed care plan (which most beneficiaries are), contact your MCO directly for their most up-to-date list of in-network therapists.
Federally Qualified Health Centers (FQHCs) are often hidden gems for Medicaid covered therapy. These community-based clinics accept Medicaid by design and typically offer comprehensive mental health services alongside medical care. You can easily locate the nearest FQHC using the HRSA Find a Health Center tool online.
When I’m helping clients find affordable care, I often recommend using Psychology Today’s therapist directory, where you can filter specifically for providers who accept Medicaid. This approach often reveals private practitioners who might not appear in official directories but are still in-network.
Don’t underestimate the power of a good referral. Your primary care doctor likely knows which mental health providers in your area take Medicaid. Similarly, local mental health organizations and community support groups can point you toward resources that might not be widely advertised.
One important tip: when contacting potential therapists, always specify which Medicaid plan you have. Some providers accept certain Medicaid managed care plans but not others, and being specific from the start saves everyone time and frustration.
Step-by-Step Checklist to Start Medicaid Covered Therapy
Once you’ve identified potential providers, following a structured approach will help ensure a smooth start to your Medicaid covered therapy journey:
First, verify your eligibility by checking that your Medicaid coverage is active and includes mental health benefits. This might seem obvious, but I’ve seen many clients skip this step only to face complications later.
Next, double-check that your chosen therapist is truly in-network with your specific Medicaid plan. Provider networks change frequently, and online directories aren’t always up-to-date. A quick phone call to confirm can save headaches down the road.
Determine if you need a referral from your primary care provider. Some Medicaid plans require this formal step before they’ll cover specialist mental health care. Similarly, check if your plan requires prior authorization for therapy—certain services need pre-approval, especially intensive programs.
When you schedule your initial assessment, be prepared to discuss your symptoms, history, and goals. This first appointment helps establish your diagnosis and treatment needs, which are essential for Medicaid coverage.
Work closely with your provider to develop a clear treatment plan, including how often you’ll meet and for how long. Understanding this from the start helps you plan and ensures you know what to expect from your Medicaid covered therapy.
Keep detailed records of all referrals, authorizations, and communications with your Medicaid plan. If there’s ever a question about coverage, having this documentation can make all the difference.
Know your rights as a Medicaid beneficiary, including how to appeal if services are denied. Every state has a process for this, and understanding it empowers you to advocate for your care.
Don’t forget practical considerations like transportation. Many people don’t realize that some Medicaid plans offer transportation assistance to medical appointments, which can remove a significant barrier to consistent care.
Finally, mark your calendar for your annual Medicaid renewal. Maintaining continuous coverage is crucial for uninterrupted mental health care.

Can I Do It Online? Telehealth and Medicaid Covered Therapy
The landscape of Medicaid covered therapy transformed dramatically during the COVID-19 pandemic, with virtual options becoming widely available—and many of these changes are here to stay.
Most state Medicaid programs now cover telehealth therapy sessions, though the specifics vary significantly by location. Some states require video capability for these sessions to be covered, while others also reimburse for audio-only (phone) therapy, which can be a game-changer for clients with limited internet access.
Many states have also relaxed requirements about provider location, meaning you might be able to see a therapist anywhere in your state—not just in your immediate area. This has dramatically expanded access, especially for rural communities where local providers are scarce.
Privacy remains paramount in virtual care. Providers must use HIPAA-compliant telehealth platforms to ensure your sessions remain confidential and secure. And just like in-person care, telehealth sessions are documented in your medical record to maintain continuity of care.
I’ve seen telehealth be particularly valuable for clients who live in rural areas with few local providers, those who struggle with transportation or mobility challenges, individuals juggling busy schedules or childcare responsibilities, and people who simply feel more comfortable opening up from the privacy of their own home.
At Thrive Mental Health, our experience shows that virtual therapy can be just as effective as in-person care for many individuals. The flexibility of telehealth often leads to better attendance and consistency, which are crucial factors in successful mental health treatment.
If you’re curious about telehealth options, I recommend checking out our guide to choosing the right individual online counseling service for more detailed information about what to look for in virtual care.
Frequently Asked Questions about Medicaid Covered Therapy
Does Medicaid really cover therapy in every state?
Yes, mental health services including therapy are covered by Medicaid programs in all 50 states. The good news is that the Mental Health Parity and Addiction Equity Act requires Medicaid managed care plans to provide mental health benefits comparable to physical health coverage.
But here’s the reality check – coverage on paper doesn’t always mean easy access in practice. Many states struggle with limited networks of providers who accept Medicaid covered therapy payments. This creates a frustrating situation where you might have coverage but still face challenges finding available appointments. This problem is especially pronounced in rural communities, where mental health providers of any kind can be few and far between.
What should I do if no therapist in my area takes Medicaid?
I’ve worked with many clients who initially struggled to find Medicaid covered therapy in their area. While it can feel discouraging, you have several practical options:
Look beyond your immediate neighborhood if you have transportation options. Sometimes driving an extra 20-30 minutes can connect you with available providers. Telehealth has been a game-changer for many of our clients – virtual therapy lets you access providers throughout your state without leaving home.
Community mental health centers are often hidden gems for Medicaid covered therapy. They typically accept Medicaid and may have shorter wait times than private practitioners. Don’t forget to contact your Medicaid managed care plan directly – they’re required to ensure you have access to covered services and might help find a provider or even cover out-of-network care if necessary.
Federally Qualified Health Centers (FQHCs) and university training clinics can be excellent alternatives. FQHCs accept Medicaid by design, while university clinics offer supervised care by graduate students at reduced rates. Some therapists who don’t formally accept Medicaid might still offer sliding scale fees based on your income.
If you’re still stuck, reach out to your state’s mental health department. They often know about additional resources or specialized programs that aren’t widely advertised.
Will I have to stop therapy if my income changes during the year?
This is one of the most common concerns I hear from clients. Income changes can indeed affect your Medicaid eligibility, but this doesn’t automatically mean losing your mental health support.
The most important thing is to report significant income changes to your state Medicaid office promptly. Many states offer transitional Medicaid coverage for people whose income increases above eligibility limits, giving you time to make alternative arrangements.
If your income rises too much for Medicaid, you’ll likely qualify for subsidized coverage through the Health Insurance Marketplace. Some states have “continuity of care” provisions that allow you to continue seeing your current therapist for a certain period even after your Medicaid coverage ends.
Be open with your therapist about your situation – many providers are willing to work with clients during transitions, potentially offering sliding scale fees or helping you find other affordable options. Community mental health centers and FQHCs typically adjust their fees based on current income, providing a safety net during financial changes.
The key is planning ahead and open communication. Don’t let fear of losing coverage prevent you from accepting better employment opportunities. With some preparation, you can maintain your mental health support even through financial transitions.
Conclusion
Finding your way through the maze of Medicaid covered therapy might feel overwhelming at first, but I promise—it gets easier once you understand what’s available to you. Think of this guide as your mental health roadmap, helping you steer a system that sometimes feels designed to be confusing.

I’ve seen how life-changing therapy can be when people finally connect with the right provider. Medicaid is actually the largest payer for mental health services in America—which means you’re not alone in using these benefits. Millions of others are walking this same path.
What makes this journey unique for everyone is that coverage details vary significantly depending on which state you call home. Your specific plan’s benefits might look different from what your cousin across the country receives. That’s why understanding your particular coverage is so important.
Yes, finding providers who accept Medicaid can sometimes feel like searching for a needle in a haystack. But don’t get discouraged! Resources like state provider directories, community health centers, and the expanding world of telehealth have opened new doors for many people. Sometimes the perfect therapist isn’t down the street—they might be a video call away.
One of the most beautiful things about Medicaid covered therapy is that financial barriers are significantly reduced. With low or no copays, you can focus on your mental health journey instead of worrying about how to pay for it. While session limits might apply in some states, knowing these boundaries upfront helps you and your therapist create a treatment plan that makes the most of your coverage.
And if your income changes? Don’t panic. A shift in financial circumstances doesn’t have to mean the end of your mental health support. Transitional coverage, marketplace options, and community resources can help you maintain continuity of care during life’s inevitable changes.
At Thrive Mental Health, we believe everyone deserves access to quality mental health care regardless of their insurance situation. Our flexible intensive outpatient and partial hospitalization programs provide expert-led, evidence-based care that meets you where you are—whether that’s at our Florida locations or through virtual programs you can access from the comfort of your own home.
Mental health care isn’t a luxury—it’s essential health care. Your financial situation shouldn’t determine whether you get the support you need. If you’re covered by Medicaid, you have options that can work for you.
Taking that first step is often the hardest part of the journey. Whether you’re picking up the phone to call your Medicaid office, reaching out to a provider from a directory, or simply acknowledging to yourself that you could use some support—you’re already moving in the right direction. And that’s something to be proud of.
For more information about insurance coverage options and how to maximize your benefits, visit our insurance resources page.
3 thoughts on “Medicaid and Mental Health—Navigating Therapy Coverage Without Losing Your Mind”
Comments are closed.