Breaking Down OCD Symptoms Without Breaking Down Yourself

Understanding OCD Symptoms: Beyond the Stereotypes
OCD symptoms are far more complex than common misconceptions suggest. True Obsessive-Compulsive Disorder isn’t about preferring things organized; it’s a debilitating cycle of unwanted thoughts and repetitive behaviors that cause significant distress.
Core OCD symptoms include:
- Obsessions: Unwanted, intrusive thoughts, images, or urges that cause intense anxiety
- Compulsions: Repetitive behaviors or mental acts performed to reduce distress from obsessions
- Time consumption: Symptoms take more than one hour per day on average
- Interference: Significant impact on daily life, relationships, and functioning
- Distress: Causes major emotional suffering and shame
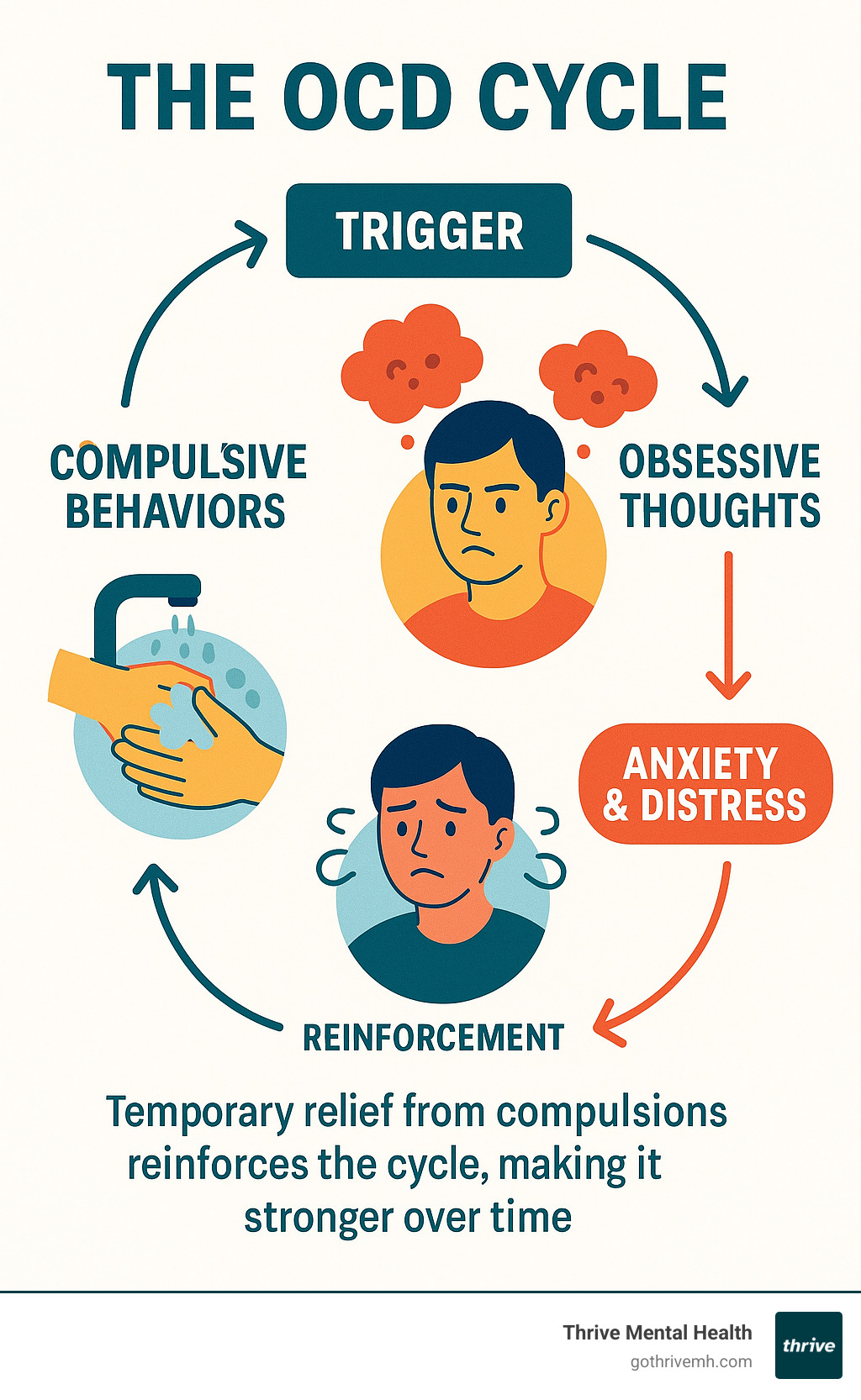
Affecting 1-2% of the US population, OCD often begins in childhood or young adulthood. It creates a vicious cycle: obsessions trigger anxiety, leading to compulsions that offer temporary relief but ultimately reinforce the pattern.
Common obsession themes include fears of contamination, harm to self or others, need for symmetry, unwanted sexual or religious thoughts, and excessive doubt about safety. Common compulsions involve excessive cleaning, checking, counting, arranging, seeking reassurance, and mental rituals.
A key challenge is their ego-dystonic nature—the thoughts and behaviors feel foreign and go against a person’s values, yet they feel compelled to perform them.
As Nate Raine, CEO of Thrive Mental Health, I’ve seen how OCD symptoms impact young professionals’ careers and relationships. Understanding these symptoms is the crucial first step toward effective treatment.
The Core of OCD: Understanding Obsessions and Compulsions
At its core, OCD involves two key components: obsessions and compulsions. Obsessions are the unwanted, intrusive thoughts that cause anxiety, while compulsions are the repetitive actions you feel driven to perform to reduce that anxiety. The relief from compulsions is only temporary and paradoxically strengthens the OCD cycle over time. This cycle can consume hours a day, severely impacting work, relationships, and well-being.
If you’re wondering whether certain experiences might indicate a broader mental health concern, you might want to Explore Symptoms: Signs You Shouldn’t Ignore.
What Are Obsessions in OCD?
Obsessions are persistent, intrusive thoughts, images, or urges that feel foreign and distressing because they often go against your core values (ego-dystonic). For example, a loving parent might have horrifying, unwanted thoughts about harming their child, leading to intense shame.
While most people have occasional intrusive thoughts, the difference in OCD is their frequency, intensity, and the distress they cause. A fleeting worry about a locked door becomes an overwhelming fear. People with OCD often know these obsessions are irrational but feel powerless to control them, leading to exhaustion from the constant waves of anxiety and fear. You can learn more about the nature of these experiences through Scientific research on intrusive thoughts.
Common Examples of Obsessive Thoughts as OCD Symptoms
OCD symptoms related to obsessions can latch onto almost anything. Common themes include:
- Fear of contamination: Intense fear of germs, disease, or feeling “mentally contaminated” by people or objects.
- Fear of harming yourself or others: Unwanted thoughts of accidentally or deliberately causing harm, which are deeply disturbing to the individual.
- Need for symmetry or orderliness: An overwhelming need for things to be perfectly aligned or “just right” to prevent distress or a feared event.
- Unwanted sexual thoughts: Intrusive sexual thoughts or urges that are explicit and go against one’s values or orientation, causing shame and worry.
- Religious or moral fears: Excessive worry about sin, blasphemy, or violating personal ethical codes (scrupulosity).
- Doubts about safety: Persistent and paralyzing doubt about safety actions, like whether the door is locked or the stove is off, despite repeated checks.
What Are Compulsions in OCD?
Compulsions are repetitive behaviors or mental acts performed to neutralize the anxiety from an obsession or prevent a feared outcome. While they provide temporary relief, this only reinforces the OCD cycle.

People with OCD don’t enjoy these rituals; they feel an overwhelming pressure to perform them. These compulsions can become rigid, time-consuming, and interfere with daily life, and can be either visible actions or hidden mental acts.
Common Examples of Compulsive Behaviors as OCD Symptoms
Compulsions can take many forms, including:
- Excessive cleaning or hand washing: Washing hands until raw, excessive showering, or spending hours cleaning to combat contamination fears.
- Checking behaviors: Repeatedly checking locks, appliances, or on loved ones to alleviate fears of harm or danger.
- Counting or repeating: Performing actions a specific number of times or repeating words to neutralize bad thoughts or achieve a “safe” feeling.
- Ordering and arranging: Spending hours arranging items in a specific way to relieve the distress caused by a need for symmetry.
- Hoarding behaviors: Difficulty discarding items, regardless of value, due to fears of losing something important or causing harm.
- Reassurance seeking: Constantly asking others for confirmation that a feared outcome won’t happen or that a task was done correctly.
- Mental compulsions: Invisible rituals like mentally repeating phrases, reviewing events, praying, or counting to neutralize obsessions. Often called ‘Pure O’.
- Avoidance: Actively staying away from people, places, or situations that trigger obsessions.
These OCD symptoms show just how extensive and often hidden the impact of the disorder can be, driving people to perform behaviors that feel irrational but absolutely necessary in the moment.
The Vicious Cycle: How OCD Symptoms Manifest and Differ from Everyday Habits
The persistence of OCD symptoms is due to a powerful cycle:
- Trigger: An internal or external cue starts the process.
- Obsession: The trigger leads to an intrusive, distressing thought.
- Anxiety: The obsession causes intense fear or distress.
- Compulsion: To relieve the anxiety, you perform a ritual.
- Relief & Reinforcement: The compulsion provides temporary relief, which teaches your brain that the ritual is necessary. This reinforcement strengthens the cycle, making the obsession more likely to return.
This cycle explains why telling someone with OCD to “just stop” is ineffective. The disorder hijacks the brain’s learning process, turning behaviors into compulsive traps. For more comprehensive information about this process, you can explore Information on OCD from the National Institute of Mental Health.
The Relationship Between Obsessions and Compulsions
The link between obsessions and compulsions isn’t always logical. While a fear of germs logically leads to handwashing, someone might tap a desk seven times to prevent a loved one from harm. This is driven by “neutralizing thoughts” and “just in case” thinking—the belief that a specific ritual can prevent a feared outcome.
Even if the person knows it’s irrational, the “what if” fear is too strong. This creates an illusion of control that reinforces the compulsion. Each time the ritual is performed and nothing bad happens, the brain credits the ritual, making it stronger and more elaborate over time.
OCD vs. Being a ‘Perfectionist’ or Having Habits
It’s crucial to distinguish OCD symptoms from perfectionism or healthy habits. The casual use of “I’m so OCD” often misrepresents a serious condition. Here are the key differences:
- Motivation: Perfectionism is driven by a desire for excellence. OCD is driven by a desperate need to reduce anxiety or prevent a feared outcome.
- Distress vs. Satisfaction: A perfectionist often feels satisfaction from their efforts. OCD compulsions provide no pleasure, only temporary relief from intense distress, fear, or disgust.
- Ego-Dystonic Nature: Perfectionistic traits are usually aligned with a person’s values (ego-syntonic). OCD obsessions are unwanted and feel foreign to one’s true self (ego-dystonic).
- Interference and Control: Healthy habits and even perfectionism are generally manageable. OCD symptoms consume more than an hour a day, feel uncontrollable, and significantly interfere with work, relationships, and daily functioning.
Recognizing these differences is key to understanding when professional help is needed for a medical condition, not just a personality trait.
The Real-Life Impact of OCD Symptoms
The impact of OCD symptoms extends far beyond thoughts, reshaping a person’s entire world. The constant battle with obsessions and compulsions infiltrates daily routines, relationships, and work, causing profound ripple effects.
Simple tasks become monumental challenges, and focus at work or school is nearly impossible when the mind is hijacked by intrusive thoughts. Shame and secrecy often lead to isolation, as individuals hide their symptoms from loved ones, feeling trapped and exhausted by the internal struggle.

Onset, Severity, and Co-Occurring Conditions
OCD symptoms typically emerge in adolescence or early adulthood, though childhood onset is possible. The severity can fluctuate, often worsening during times of stress or major life transitions.
OCD rarely exists in isolation. It frequently co-occurs with other conditions, complicating diagnosis and treatment. Common co-occurring disorders include:
- Anxiety Disorders (generalized anxiety, panic disorder, social anxiety)
- Depression, often resulting from the chronic distress of OCD
- Tic Disorders
- Eating Disorders
- Hoarding Disorder
- Body Dysmorphic Disorder
Effective treatment requires addressing these related conditions. For more comprehensive information, you can explore Disorders Related to (And Sometimes Confused with) OCD.
How OCD Affects Daily Functioning and Relationships
The daily impact of OCD is immense. Symptoms can consume three to eight hours a day, derailing routines and harming academic and professional performance. Relationships suffer as family and friends become entangled in rituals or frustrated by constant reassurance-seeking.
To avoid triggers and shame, many people withdraw socially, leading to profound isolation. The physical toll is also significant, from raw skin due to excessive washing to sheer exhaustion. This constant struggle diminishes quality of life and can lead to hopelessness.
Recognizing this full-scope impact is a crucial first step toward seeking treatment, as OCD symptoms are highly treatable with the right support.
Recognizing When to Seek Professional Help
Knowing when to seek help for OCD symptoms is critical. The line is crossed when thoughts and behaviors cause significant distress, consume over an hour a day, and interfere with your life. Reaching out can be daunting due to shame, but OCD is a serious condition that rarely improves without specialized treatment.
If symptoms are impacting your quality of life and feel beyond your control, it’s time to speak with a mental health professional. This is a courageous step toward reclaiming your life. For guidance on finding the right support, explore our guide on Finding the Best Mental Health Therapist Near You.
The Diagnostic Criteria for OCD
A formal OCD diagnosis requires that OCD symptoms meet specific criteria. A mental health professional will assess for the following:
- Presence of Obsessions, Compulsions, or Both: The individual experiences intrusive thoughts and/or engages in repetitive behaviors.
- Significant Distress or Impairment: Symptoms cause marked distress, are time-consuming (take more than one hour per day), and interfere with social, occupational, or other important areas of functioning.
- Not Attributable to Other Causes: The symptoms are not the result of a substance or another medical condition.
- Distinct from Other Mental Disorders: The symptoms are not better explained by another mental health condition.
An accurate diagnosis is the foundation for effective treatment.
What Does Treatment for OCD Look Like?
The good news is that OCD is highly treatable. Evidence-based treatments can significantly reduce OCD symptoms and improve quality of life. The main treatments include:
- Exposure and Response Prevention (ERP): A specific type of Cognitive Behavioral Therapy (CBT), ERP is the gold standard for OCD. It involves gradually facing feared situations (exposures) while resisting the urge to perform compulsions (response prevention). This breaks the OCD cycle by teaching the brain that anxiety decreases on its own without rituals.
- Cognitive Behavioral Therapy (CBT): Broader CBT techniques help identify and challenge the distorted thinking patterns that fuel obsessions.
- Medication: Selective Serotonin Reuptake Inhibitors (SSRIs) are often prescribed to reduce the intensity of obsessions and anxiety, making therapy more effective.
- Combined Approach: For many, a combination of ERP and medication is the most effective strategy.

At Thrive Mental Health, we believe in flexible, expert-led, evidence-based care custom to individual needs. We use these proven techniques to help our clients regain control over their lives. To learn more about how CBT can help, explore A Beginner’s Guide to Cognitive Behavioral Therapy (CBT). For a broader understanding of therapeutic options, you can also check out Understanding Different Types of Mental Health Therapy.
Frequently Asked Questions about OCD Symptoms
Many common questions arise about OCD symptoms, highlighting the complexities of this often-misunderstood condition. Let’s explore some of the most frequent ones.
Can you have OCD without compulsions?
This is a common question, often related to the term “Pure O” (purely obsessional). The reality is that compulsions are almost always present in OCD, but they can be purely mental and invisible to others. These mental compulsions serve the same function as physical ones: to reduce anxiety. Examples include:
- Rumination: Endlessly trying to “solve” or analyze an obsession.
- Self-Reassurance: Mentally arguing with an obsessive thought.
- Checking Feelings: Constantly monitoring internal states (e.g., checking for arousal in response to an unwanted sexual thought).
- Mental Rituals: Silently repeating words, phrases, or prayers.
- Avoidance: Actively avoiding triggers for obsessions.
Because these compulsions happen internally, the term “Pure O” is misleading. The compulsive element is still a core part of the disorder.
Do people with OCD know their thoughts are irrational?
Yes, most of the time. Insight in OCD exists on a spectrum:
- Good or Fair Insight: The individual recognizes their OCD beliefs are irrational or excessive. This is the most common scenario and causes significant internal conflict, as they feel compelled to perform rituals they know are illogical.
- Poor Insight: The individual thinks their OCD beliefs are probably true.
- Absent Insight (Delusional Beliefs): The individual is completely convinced their OCD beliefs are true.
A person’s level of insight can also fluctuate, often decreasing when anxiety is high. This awareness of the irrationality is one of the most frustrating parts of living with OCD.
Can OCD symptoms develop suddenly?
While OCD symptoms often develop gradually, they can appear suddenly. This can happen in a few scenarios:
- PANDAS/PANS: In children, a sudden, dramatic onset of OCD can follow an infection (like strep throat). This is a neuro-autoimmune response that requires medical evaluation.
- Trauma or Major Stress: Symptoms can be triggered or severely worsened by traumatic events, periods of high stress, or even major positive life changes like marriage or parenthood.
Whether the onset is gradual or sudden, the appearance of debilitating OCD symptoms warrants professional evaluation.
Conclusion: Taking the First Step Towards Managing OCD
Understanding OCD symptoms is the first step toward managing them. We’ve seen that OCD is not a personality quirk but a complex disorder of obsessions and compulsions that can feel like an unbreakable prison, affecting relationships, work, and daily life.
The most important message is this: OCD is a highly treatable condition. Recovery is not just possible; it’s expected with the right, evidence-based care. The brain patterns that create the OCD cycle can be rewired. This journey begins with recognizing you deserve help and that suffering in silence is not the answer.
At Thrive Mental Health, our flexible, expert-led, evidence-based care is built around what works for OCD. We provide specialized therapies like Exposure and Response Prevention (ERP) and Cognitive Behavioral Therapy (CBT)—the gold standard treatments—through intensive outpatient and partial hospitalization programs that fit your life.
General therapy is often not enough for the unique challenges of OCD symptoms. Specialized care like ERP is designed to help you break the cycle by facing your fears without performing compulsions. With expert guidance, this process is incredibly effective at reducing OCD’s power over your life.
You don’t have to do this alone. Our Virtual Intensive Outpatient Programs provide structured support from anywhere. To learn more about the most effective treatment, explore how Exposure and Response Prevention (ERP) Therapy can help you reclaim your life from OCD.
Taking the first step is the hardest but most important one. Your life doesn’t have to be defined by OCD symptoms. With the right support, you can find freedom and live by your own values.

