When Life Feels Heavy but Plans Stay Lighthearted – Passive Suicidal Ideation
Understanding the Weight of Passive Suicidal Ideation
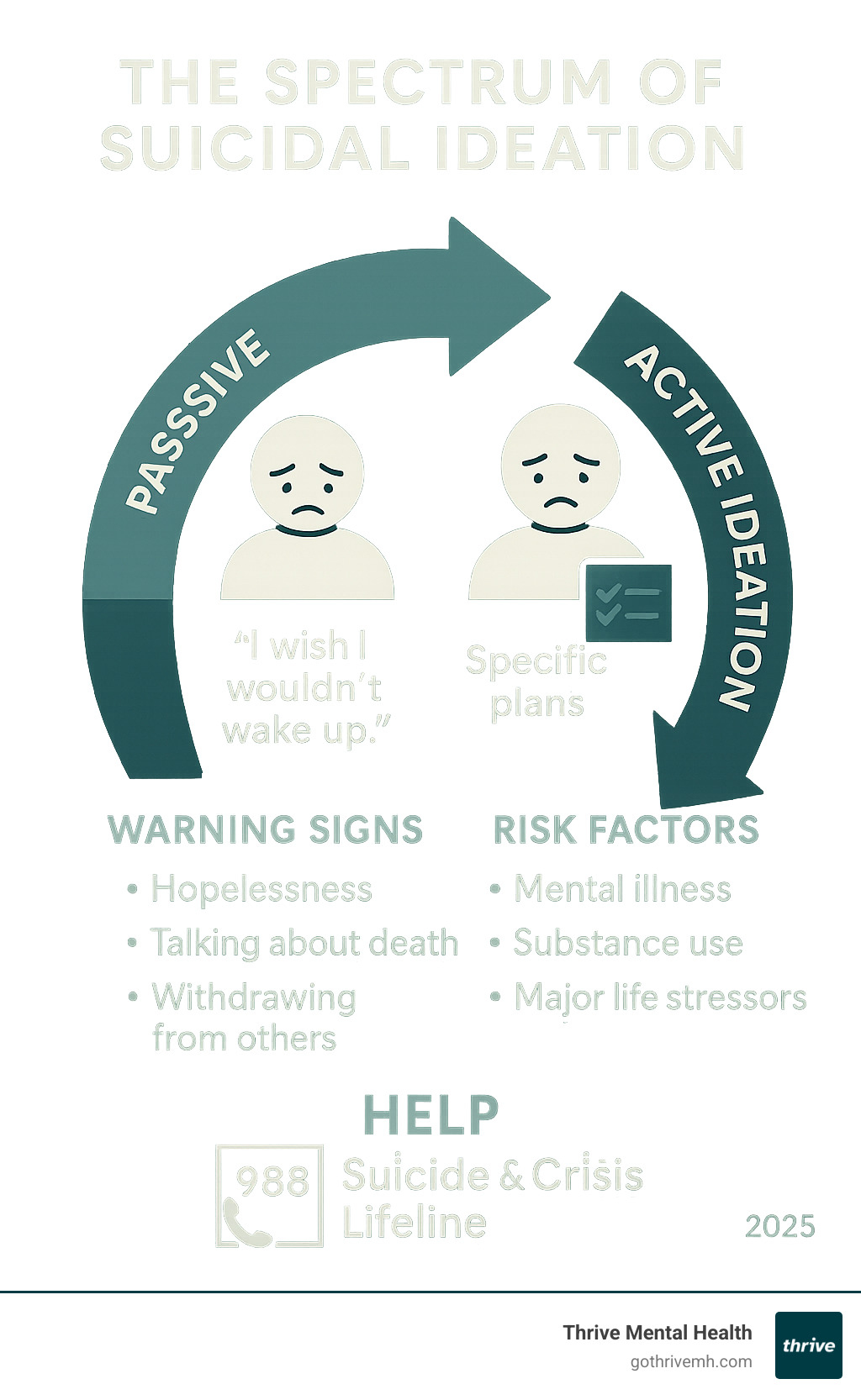
Passive Suicidal Ideation refers to thoughts about dying or wishing to be dead without a specific plan or intent to act. Unlike active suicidal ideation, which involves concrete plans, passive ideation is a more general wish to escape life’s pain.
Key characteristics of Passive Suicidal Ideation:
- Thoughts of death without specific plans
- Wishing to “not wake up” or “disappear”
- Feeling indifferent about living or dying
- No active intent to harm oneself
- Often accompanied by hopelessness and feeling like a burden
Common expressions include thoughts like “I wish I was never born” or “I hope I die in my sleep.” These thoughts signal significant emotional distress and require attention.
Research shows that passive suicidal ideation affects approximately 5.8% of the general population annually. While these thoughts don’t involve immediate plans, they are a serious warning sign.
The spectrum of suicidal ideation exists on a continuum, and passive thoughts can escalate to active planning. Studies show people with passive thoughts are at an equal risk of attempting suicide as those with active thoughts, making early intervention crucial.
If you’re experiencing these thoughts, help is available through the 988 Suicide & Crisis Lifeline (call or text 988). Professional support can help address underlying causes and develop healthy coping strategies.
I’m Nate Raine, CEO of Thrive Mental Health. I’ve dedicated my career to creating innovative mental health solutions, including comprehensive approaches to Passive Suicidal Ideation. I’ve seen how proper recognition and treatment can transform lives and provide hope.
What is Passive Suicidal Ideation and How Does It Feel?
When life feels overwhelming, thoughts of dying or not existing—without a plan to act—can arise. This is Passive Suicidal Ideation.
Passive Suicidal Ideation is fundamentally different from active suicidal ideation. While active thoughts involve a clear intent to act and a specific plan, passive ideation is more like a wish that death would happen naturally. It’s the difference between planning to harm yourself and simply wishing you wouldn’t wake up.
Those with Passive Suicidal Ideation often feel trapped by overwhelming emotional pain, feel like a burden, or experience deep hopelessness. This can lead to emotional numbness and a sense of detachment from life. The experience often includes fantasizing about not existing for the relief it might bring. Many feel indifferent about living or dying, which can be just as frightening as active thoughts.
Defining Passive Suicidal Ideation and Its Common Expressions
Passive Suicidal Ideation shows up in thoughts that reveal significant emotional distress that deserves attention. These thoughts don’t include planning or preparation.
Common expressions include “I wish I wouldn’t wake up,” “I wish a car would hit me,” or “I just want the pain to stop.” These thoughts reflect a desire for relief, not a plan for action.
It often involves apathy and an indifference to life. People may stop making future plans or lose interest in things they once enjoyed. This lack of future-oriented thinking can feel like living in a gray fog where nothing matters.
Emotional numbness is also common. Instead of sadness or anger, many feel nothing at all, as if disconnected from their own lives.
Comparing Passive vs. Active Suicidal Ideation
| Feature | Passive Suicidal Ideation | Active Suicidal Ideation |
|---|---|---|
| Presence of a Plan | No specific plan to end one’s life. | A concrete, often detailed plan (method, time, place). |
| Intent to Act | No active intention to take one’s own life; wishing death would happen naturally. | Clear intention and motivation to carry out the plan. |
| Preparatory Behaviors | May engage in risky behaviors (e.g., not wearing a seatbelt) but not directly suicidal. | May engage in behaviors like researching methods, acquiring means, giving away possessions. |
| Immediacy of Risk | Serious, but not typically an immediate, acute emergency. Can escalate. | High, immediate risk; considered a mental health emergency. |
| Example Thoughts | “I wish I wouldn’t wake up.” “I hope I die in my sleep.” “I just want it all to stop.” | “I will take [method] on [date] at [place].” “I’m going to kill myself.” |
Understanding these differences is crucial. Passive Suicidal Ideation is a warning sign of serious emotional pain that needs support, even without immediate danger.
Key Risk Factors and Underlying Causes
Passive Suicidal Ideation rarely appears overnight. It’s usually the result of multiple factors creating a storm of emotional distress.

The most significant risk factor is an underlying mental health condition. Depression can lead to thoughts of not wanting to exist. Overwhelming worry from anxiety disorders can make death seem like an escape. Bipolar disorder creates vulnerability during depressive episodes, and PTSD can make the present feel unlivable by trapping someone in past trauma.
Childhood trauma leaves lasting scars that increase the risk of suicidal thoughts. Research shows that adverse childhood experiences create a foundation of emotional pain that can resurface during stress.
Chronic pain or illness can wear down a person’s will to live. When physical suffering is constant, wishing for it to stop is understandable. Substance use is often a way to numb pain but typically creates a vicious cycle that worsens the situation.
Social isolation is a major contributor. Feeling disconnected can amplify dark thoughts. Major life stressors like financial problems, relationship issues, or grief can also trigger passive suicidal thinking in those already struggling. A family history of suicide also increases risk.
Vulnerable Populations and Unique Stressors
Certain groups face additional challenges that put them at higher risk.
LGBTQIA+ youth face higher risk due to discrimination, rejection, and lack of acceptance. Data from The Trevor Project shows alarming rates of suicidal thoughts in this group, often stemming from a lack of support.
Veterans carry unique burdens like combat trauma and difficulty adjusting to civilian life. The warrior mentality can make it harder to ask for help.
Older adults face challenges like chronic illness, loss of loved ones, and social isolation, which can contribute to thoughts of wanting to die.
Individuals with neurodevelopmental disorders like ADHD or autism may struggle with emotional regulation and feeling different, which can be exhausting and lead to thoughts of giving up.
At Thrive Mental Health, our flexible, evidence-based approach recognizes these risk factors and tailors treatment to each individual’s challenges.
Why It’s Critical to Address Passive Suicidal Ideation
It’s dangerous to view Passive Suicidal Ideation as less urgent than active ideation. These thoughts are a serious warning sign that shouldn’t be ignored.
The primary reason to take PSI seriously is the escalation of risk. Passive wishes can shift toward active planning, and since this progression is unpredictable, early intervention is crucial.
Research confirms this. Over two-thirds of patients with death wishes later developed more intense suicidal thoughts. Furthermore, research on the risk of repetition after ideation reveals that people with passive versus active thoughts face an equal risk of attempting suicide, making PSI a top risk factor for suicide attempts.
Beyond this risk, PSI takes a heavy toll on daily life. The constant thoughts are mentally and emotionally exhausting, like carrying an invisible weight. This burden affects everything: relationships suffer from withdrawal, work or school performance drops, and self-care declines as motivation fades.
The good news is that early intervention works. Addressing PSI before it escalates allows for treating the underlying causes and learning healthier coping strategies.
Observable Signs in Yourself or Others
Recognizing PSI is tricky, as people often keep these thoughts private out of fear of judgment. However, observable changes can signal internal struggles.
- Social withdrawal and expressing feelings of hopelessness or being trapped.
- Neglecting personal care and responsibilities at work or school.
- Giving away meaningful possessions or an increase in substance use.
- Dramatic shifts in sleep and eating patterns.
- Talking or writing about death, even in abstract ways.
- Loss of interest in hobbies and a pervasive sense of emotional numbness.
- Risky behavior, like careless driving or not taking medication.
- Unexplained mood shifts that don’t match their circumstances.
If you notice these signs in yourself or someone else, approach the situation with compassion. Listening without judgment can be the first step. Recognizing signs isn’t about diagnosing; it’s about caring enough to encourage professional support.
The Path to Healing: Assessment, Treatment, and Support
Recognizing Passive Suicidal Ideation in yourself or a loved one is the first crucial step toward healing. These thoughts aren’t a sign of weakness; they’re a signal that something deeper needs attention.

Stigma often prevents people from seeking help, but PSI is a symptom of emotional pain, not a character flaw. Reaching out for mental health support is a sign of courage.
Recovery is possible. With the right support, people can find relief and meaning. At Thrive Mental Health, we’ve seen many individuals move from being trapped by their thoughts to building hopeful futures. Learn more about our treatment programs and how we can support you.
Professional Assessment of Passive Suicidal Ideation
A mental health professional will conduct a thorough, non-judgmental assessment to create an effective treatment plan. The process usually starts with a clinical interview to understand the context of your thoughts and identify contributing factors. Clinicians may use psychological evaluation tools, like the PHQ-9 or the Beck Scale for Suicidal Ideation, to measure the frequency and intensity of your thoughts.
Assessing your risk level is crucial. A therapist will evaluate all factors to watch for any signs of escalation toward active ideation. The assessment also involves differentiating from other conditions that may require different treatment approaches.
A key outcome is creating a safety plan: a personalized roadmap for managing difficult moments. It outlines coping strategies, triggers, support contacts, and crisis resources.
Evidence-Based Treatments and Management
Passive Suicidal Ideation responds well to treatment. Several proven, customized approaches can help you manage these thoughts and improve your well-being.
Psychotherapy is the foundation of treatment. Cognitive Behavioral Therapy (CBT) is highly effective, helping you identify and change negative thought patterns and learn practical coping skills. Dialectical Behavior Therapy (DBT) is also powerful, especially for intense emotions. It teaches skills in mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness.
Medication, such as antidepressants or mood stabilizers, can address underlying conditions like depression. A provider will work with you to find the right medication and dosage, with careful monitoring, as some can initially increase suicidal thoughts in people under 25.
For more intensive support, Intensive Outpatient (IOP) and Partial Hospitalization (PHP) programs offer structured care with several hours of therapy per week. At Thrive Mental Health, our flexible programs are designed to fit into your life while providing this level of support.
Lifestyle changes also support recovery. Prioritizing sleep, a balanced diet, regular physical activity, and meaningful hobbies are powerful tools for emotional well-being. Building a strong support system of friends, family, or support groups is also crucial to reduce isolation.
As SAMHSA’s treatment guide for suicidal ideation emphasizes, there’s no one-size-fits-all approach. At Thrive Mental Health, we work collaboratively with you to find the healing path that fits your unique needs. Recovery is possible, and you don’t have to face this journey alone.
How to Find Immediate and Ongoing Support
When you or a loved one experiences Passive Suicidal Ideation, knowing where to turn can feel overwhelming. The good news is that trained help is available now.
If you’re having these thoughts, reaching out is a sign of strength, not weakness. It means you’re taking care of yourself. These thoughts signal you’re carrying too much pain to handle alone. If you’re supporting a loved one, your concern and presence are powerful. Knowing someone cares can make all the difference.
Immediate Help Resources
- The 988 Suicide & Crisis Lifeline is available 24/7 by calling or texting 988. This free, confidential service connects you with trained counselors. You don’t need to be in immediate danger to reach out; these thoughts deserve attention.
- The Crisis Text Line is another option: text HOME to 741741. Trained crisis counselors are available 24/7 to text with you.
- The National Alliance on Mental Illness (NAMI) HelpLine provides information and support at 1-800-950-NAMI (6264) or via email at info@nami.org.
- For immediate life-threatening emergencies, call local emergency services (911).
Supporting a Loved One
Learning a loved one has Passive Suicidal Ideation can be scary. You might worry about saying the wrong thing, but your willingness to be supportive is what matters most.
- Listen without judgment. Let them share without trying to fix things. Avoid minimizing their pain with phrases like “just think positive.”
- Express your concern directly. Say, “I’ve been worried about you” or “I care about you.” Let them know their life matters to you.
- Encourage professional help gently. Offer to help them find a therapist or make an appointment. At Thrive Mental Health, our flexible programs are designed to make that first step easier.
- Remove potential means of self-harm if you’re concerned about escalation. Safely store medications, sharp objects, or firearms to create a safer environment.
- Follow up regularly. Recovery isn’t linear. Consistent check-ins, even small gestures, remind them they’re not alone.
- Practice self-care. Supporting someone is emotionally draining. Ensure you have your own support system so you can be there for them long-term.
Frequently Asked Questions about Passive Suicidal Ideation
Is it normal to have passive suicidal thoughts?
While common during times of high stress or depression, Passive Suicidal Ideation isn’t “normal” in the sense of being healthy. These thoughts are a signal of significant emotional distress that needs attention.
Like a fever, these thoughts are a sign that something needs care. They should never be dismissed and are a clear signal to reach out for support.
Can passive suicidal ideation go away on its own?
Passive Suicidal Ideation is unlikely to resolve on its own without addressing the underlying causes. Ignoring these thoughts can make them more intense or escalate to active ideation. They often stem from deeper issues like mental health conditions, trauma, or chronic stress.
The good news is that professional help is the most effective way to overcome these thoughts. A therapist can help you find the root causes and develop healthy coping strategies. At Thrive Mental Health, we help individuals work through these challenges and find their way back to a life they want to live.
How do I talk to someone I’m worried about without making things worse?
Approaching this conversation with empathy and genuine concern is key. It can feel scary, but it shows you care.
Choose a private, calm setting. Start with “I” statements like, “I’ve been worried about you lately,” or “I care about you, and I’ve noticed some changes that concern me.”
Listen more than you talk. It’s about being present, not finding solutions. Validate their feelings with phrases like, “That sounds incredibly difficult.”
Gently suggest seeking professional help, and offer to assist them. Avoid minimizing their pain with phrases like “snap out of it.” Your goal is to show support and encourage professional help. Just having the conversation can be the first step toward healing.
Conclusion
Passive Suicidal Ideation is a common but misunderstood aspect of mental health. Understanding it helps us respond with more compassion and urgency.
These thoughts are a serious warning sign of unbearable emotional pain. While PSI doesn’t involve concrete plans, the risk of escalation is significant. A wish to “not wake up” can signal real danger.
Although common, these experiences can feel isolating due to shame and stigma. Remember: experiencing Passive Suicidal Ideation is not a character flaw or a sign of weakness. It’s a sign that the pain is too much to bear alone.
The good news is that help is available and effective. Through therapy, medication, or intensive programs, recovery is possible. People who once felt trapped go on to live full, meaningful lives.
Taking the first step is crucial. Reaching out for yourself or a loved one is a moment of courage that can change everything.
At Thrive Mental Health, our flexible, expert-led, evidence-based care is custom to you. Our virtual and in-person IOP and PHP programs offer comprehensive support for adults and young professionals that fits into their daily lives.
You don’t have to face this alone. Recovery is possible, and it starts with reaching out.
Learn more about our flexible and expert-led mental health programs.
