Everything You Need to Know About Adult Dissociative Disorder Treatments

Dissociating, Losing Time, Feeling Unreal? [Here’s What Actually Helps You Recover]
Which treatment approaches help adults with dissociative disorders recover? For most adults, real progress comes from a targeted mix of:
- Phase-oriented psychotherapy (stabilize → process trauma → integrate and rebuild life)
- Trauma-focused therapies like CBT, DBT, or EMDR
- Grounding and distress tolerance skills to stop spirals in real time
- Medication for depression, anxiety, panic, or mood swings that make recovery harder
- Specialized care from therapists trained in trauma and dissociation
When these pieces line up, adults often cut symptom severity, reduce self-harm, and get back to work, school, and relationships—sometimes after years of feeling stuck.
Dissociative disorders affect roughly 1.5% of American adults—over 3 million people. If you’re one of them, you know how brutal it is:
- You lose time and can’t explain what you did.
- You feel detached from your body or like the world isn’t real.
- You struggle to trust your own memories.
It’s scary. It’s expensive in time, energy, and often money. And it can feel like you’re impossible to treat.
You’re not. You are not broken. Dissociation was a survival mechanism. With the right treatment approach, it stops running your life and becomes something you understand and can control.
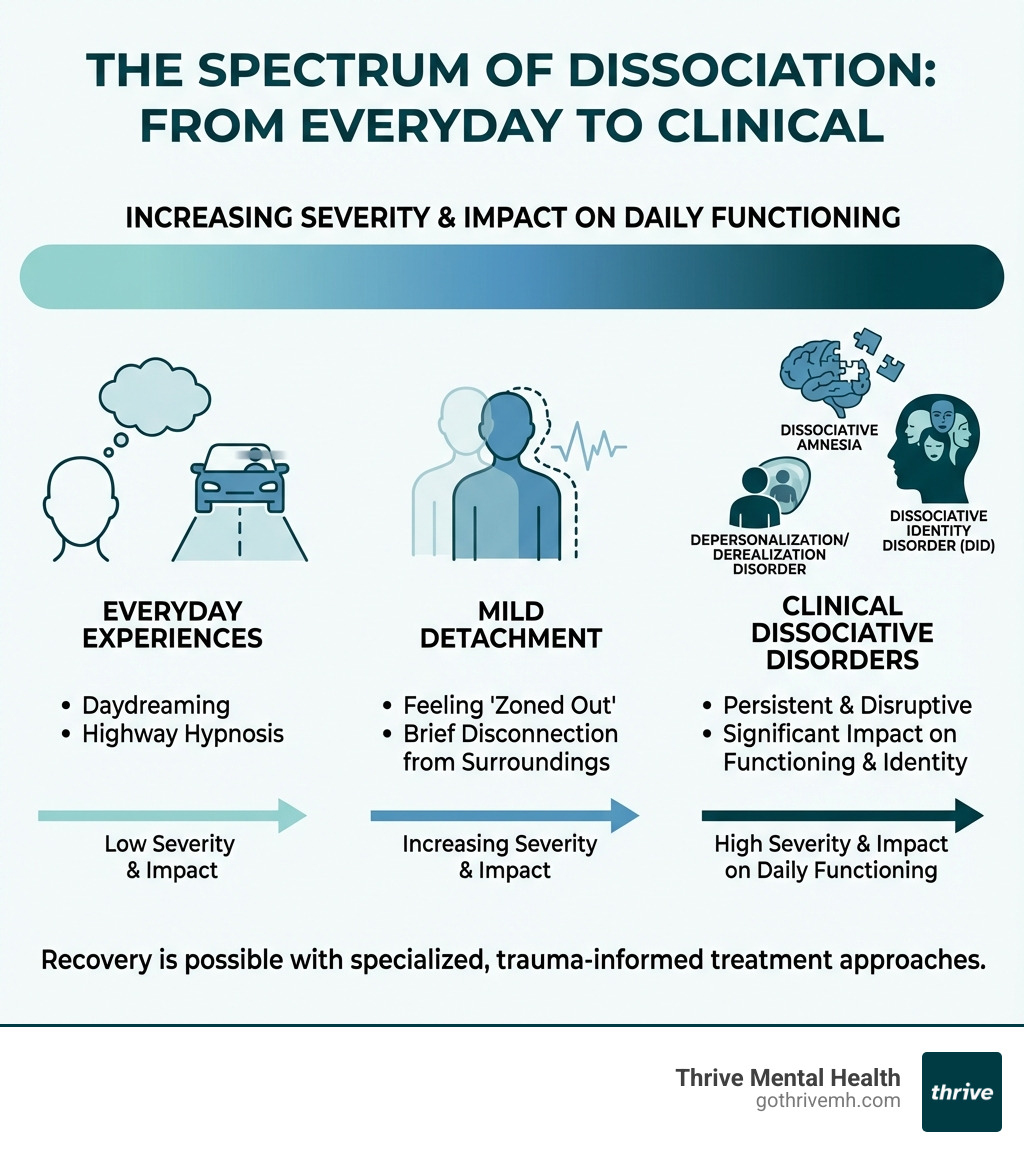
Dissociation exists on a spectrum. Everyone zones out sometimes. But when it disrupts your memory, identity, work, or relationships, it becomes a clinical dissociative disorder—like Dissociative Identity Disorder (DID), dissociative amnesia, or depersonalization/derealization disorder.
The upside: Trauma-informed, phase-based treatment works. Research and real-world programs show that many adults:
- Achieve full integration of identity, or
- Build solid skills to control symptoms, keep jobs, and maintain relationships—even if some symptoms remain.
I’m Nate Raine, CEO of Thrive Mental Health. For over a decade, I’ve built data-driven treatment models for complex trauma. Knowing which treatment approaches help adults with dissociative disorders recover is at the core of how we design our Intensive Outpatient Programs (IOP) and Partial Hospitalization Programs (PHP)—both virtual and in-person—across Florida.
This guide shows you, step by step, what actually works, how long it takes, and how to find high-quality, insurance-friendly care that doesn’t waste your time.
Must-know Which treatment approaches help adults with dissociative disorders recover? resources:
- Eggshell Parenting: Causes, Signs & How to Heal
- What Are Signs of Abandonment Issues in Adults?
- Virtual mental health counseling: complete guide
- Remote IOP/PHP and insurance options
The 3-Phase Treatment Model: Your Roadmap to Stability and Integration
If you’re thinking about suicide or self-harm, pause reading and call or text 988 right now. You are not alone, and help is available 24/7.
CALLOUT BOX: If you’re in crisis, call/text 988 right now. You are not alone.
When you’re dealing with dissociative disorders—especially Dissociative Identity Disorder (DID)—you can’t just “jump into trauma work” and hope for the best. That approach backfires, increases hospitalizations, and burns people out.
The International Society for the Study of Trauma and Dissociation (ISSTD) recommends a 3-phase treatment model. We use this as our blueprint at Thrive. It prioritizes safety first, then careful trauma processing, then long-term integration and rebuilding your life.
Phase 1: Build Safety and Control Before Anything Else
The first phase is not optional. It’s about staying alive, out of the hospital, and in control enough to handle real life.
Over 70% of outpatient DID patients report at least one suicide attempt. That’s why we focus first on:
- Suicide and self-harm risk management
- Stabilizing daily routines (sleep, food, meds, structure)
- Reducing dangerous dissociation (losing time, risky behavior)
What is the importance of psychoeducation in the treatment of dissociative disorders?
Psychoeducation explains why you dissociate in plain language: your brain used dissociation to survive trauma. When you understand that, you:
- Feel less ashamed and “crazy”
- Can explain your condition to loved ones
- Know what to expect from each phase of treatment
That understanding immediately lowers fear and resistance—and makes every other tool more effective.
What are grounding skills, and how do they help manage dissociative symptoms?
Grounding skills keep you in the present moment when you start to float away, numb out, or feel unreal. They’re fast, practical, and you can use them anywhere.
Two types we teach in our virtual and in-person IOP/PHP programs:
-
Cognitive grounding
- Describe the room in detail (colors, shapes, objects).
- Count 5 things you see, 4 you feel, 3 you hear, 2 you smell, 1 you taste.
- Do quick math in your head (e.g., count backward by 7s).
-
Sensory grounding
- Hold an ice cube or splash cool water on your face.
- Grip the arms of a chair, noticing texture and pressure.
- Slowly drink tea or water, paying close attention to taste and temperature.
Used consistently, grounding reduces episodes of “losing time” and helps you stay oriented in therapy and daily life.
How do distress tolerance skills contribute to the recovery process for dissociative disorders?
Distress tolerance skills—often pulled from Dialectical Behavior Therapy (DBT)—help you survive emotional storms without self-harm, substance use, or dangerous dissociation.
Key tools we teach include:
-
TIPP skills:
- Temperature: cold water, ice packs, or a cool cloth to reset your nervous system.
- Intense exercise: brief bursts (jumping jacks, fast walking).
- Paced breathing: slow exhale-focused breathing.
- Paired muscle relaxation: tensing and releasing muscles.
-
ACCEPTS:
- Activities, Contributing, Comparisons, opposite Emotions, Pushing away, Thoughts, Sensations.
-
IMPROVE the moment:
- Imagery, Meaning, Prayer/values, Relaxation, One thing in the moment, brief “Vacation,” Encouragement.
These skills help you get through the worst moments without making them worse, so you can stay in treatment and keep your life on track.
What is the significance of emotion regulation skills in managing dissociative disorders?
Emotion regulation skills help you:
- Name what you feel instead of shutting down
- Spot emotional triggers early
- Choose safer behaviors when overwhelmed
As your ability to manage emotions grows, dissociation often decreases because your system no longer “needs” to check out as quickly.
How do interpersonal skills training and development aid in the recovery from dissociative disorders?
Trauma and dissociation often wreck trust, boundaries, and communication. Interpersonal effectiveness skills help you:
- Say no without guilt
- Ask for what you need clearly
- Walk away from unsafe people faster
Better relationships mean more practical support and less relational chaos, which directly improves stability and speeds recovery.
At Thrive Mental Health, our Intensive Outpatient Programs (IOP) and Partial Hospitalization Programs (PHP) are built around this Phase 1 work. We offer virtual and hybrid options across Florida, and accept many plans (including Cigna, Optum, and Florida Blue) so you can get high-level care without relocating.
Phase 2: Process Traumatic Memories Safely—Without Falling Apart
Once you’re reasonably stable—less suicidal, fewer dangerous dissociative episodes, basic life structure in place—we move into Phase 2: trauma processing.
How does trauma-focused therapy help individuals with dissociative disorders?
Trauma-focused therapy helps you face what happened without reliving it 24/7.
We use tools like:
- Careful titration (small doses of memory instead of full exposure)
- Pacing that respects your nervous system
- Linking past events to current triggers and symptoms
The work includes:
- Remembering: Bringing fragments of memory together.
- Tolerating: Staying present with tough emotions in small, manageable pieces.
- Processing: Making sense of events instead of blaming yourself or staying confused.
- Grieving and mourning: Allowing sadness and loss that’s been blocked for years.
Done well, this phase reduces flashbacks, body memories, and shame, and makes your story coherent instead of shattered.
Phase 3: Integration, Rehabilitation, and Building a Life You Actually Want
In Phase 3, you’re not just surviving—you’re rebuilding.
What are the key stages and goals in treating Dissociative Identity Disorder (DID)?
For DID, Phase 3 means:
- More internal cooperation and less internal conflict
- Better coordinated functioning in work, parenting, school, and relationships
- For many, integration/unification of parts into a more cohesive self
You’ll focus on:
- Revisiting your history from a more unified perspective
- Strengthening a stable adult identity that can lead your life
- Applying relationship skills to build healthier, more mutual connections
- Turning energy from “putting out fires” to planning the future
The goal: you can handle everyday stress, make decisions, and maintain relationships without needing to dissociate as your main coping tool.
Which Treatment Approaches Help Adults with Dissociative Disorders Recover? [Core Therapies That Actually Work]
Psychotherapy is the core treatment for dissociative disorders. Medication can support, but it cannot replace therapy.
A strong plan usually combines phase-oriented treatment with one or more of these trauma-informed approaches.

Here’s a quick breakdown of which therapies help adults with dissociative disorders recover, what they focus on, and who they’re best for:
| Therapy Type | What It Focuses On | Key Techniques | Best For |
|---|---|---|---|
| Psychodynamic Therapy | How past experiences and unconscious conflicts (often childhood trauma) shape current emotions, relationships, and identity. | Exploring early relationships and trauma; understanding defenses; working through transference; integrating fragmented self-states. | Adults with complex trauma who want deep insight into patterns and identity, and can commit to longer-term work. |
| Cognitive-Behavioral Therapy (CBT) | How thoughts drive feelings and behavior, especially around trauma, identity, and safety. | Identifying and challenging distorted beliefs; behavioral experiments; careful exposure to trauma-related cues; building metacognitive skills. | Stabilized adults ready to target specific fears, avoidance, or “I’m crazy/unsafe” beliefs. Strong for PTSD with dissociation and adaptable for DID. |
| Dialectical Behavior Therapy (DBT) | Managing extreme emotions, impulses, and relationship chaos that fuel dissociation. | Mindfulness; distress tolerance (e.g., TIPP, ACCEPTS); emotion regulation; interpersonal effectiveness; validating and coordinating internal parts. | Adults with dissociation plus self-harm, suicidal thoughts, or Borderline Personality Disorder (BPD). Often a Phase 1/2 foundation before deeper trauma work. |
| Eye Movement Desensitization and Reprocessing (EMDR) | Safely reprocessing traumatic memories so they lose their intense emotional charge. | Bilateral stimulation (eye movements, tapping); 8-phase protocol; targeting specific memories or themes; modified pacing to avoid flooding. | Adults who are relatively stable, have strong coping skills, and work with a clinician trained in EMDR for dissociation/DID. |
How Does Trauma-Focused Therapy Help Individuals with Dissociative Disorders?
Trauma-focused therapy directly targets the events that drove your nervous system to rely on dissociation.
Done well, it helps you:
- Remember without being overwhelmed
- Make sense of “random” triggers
- Reduce shame and self-blame
- Turn terrifying memories into part of your story, not the whole story
At Thrive, we:
- Build safety and skills before trauma exposure
- Let you set the pace
- Use clear backup plans if you start to feel flooded or dissociate in session
What is the Role of Psychodynamic Therapy in Treating Dissociative Disorders?
Psychodynamic therapy is especially useful when your symptoms are tied to long-term, complex childhood trauma.
It helps you:
- See how early experiences shaped your current triggers
- Understand why certain parts formed and what they protect
- Bring hidden conflicts into the open, so they no longer control you from the background
Over time, this can lead to a more unified identity and less internal fighting.
How is Cognitive-Behavioral Therapy (CBT) Adapted to Help Adults with Dissociative Disorders Recover?
CBT is adapted for dissociation by focusing on:
- Core beliefs like “If I remember, I’ll die,” “I’m dangerous,” or “No one is safe”
- Thought patterns that lock in avoidance and dissociation
- Gradual testing of new beliefs in real life
We also use CBT to:
- Build awareness of shifts in state (“parts”) and related thoughts
- Create farewell or transition rituals when an alter no longer needs to carry a specific job (like self-harm or protection)
Result: less catastrophic thinking, more choice, and lower dissociation as fear decreases.
What are the Principles of Dialectical Behavior Therapy (DBT) for Dissociative Disorders?
DBT balances acceptance and change. For dissociative disorders, that means:
- Accepting that all parts/identities formed to help you survive
- Teaching them new, safer skills so they don’t have to use extreme behaviors
Core DBT skills for dissociation:
- Mindfulness: noticing shifts in awareness without judgment
- Distress Tolerance: getting through urges to self-harm or dissociate
- Emotion Regulation: staying in the window of tolerance
- Interpersonal Effectiveness: asking for help, setting limits, leaving unsafe situations
This often reduces self-harm, ER visits, and hospital stays, clearing the way for deeper trauma work.
How Does EMDR Therapy Work for Dissociative Disorders (and Its Limits)?
EMDR helps your brain reprocess traumatic memories so they feel like something that happened, not something that’s still happening.
We use:
- Bilateral stimulation (eye movements, tapping, alternating sounds)
- Careful targeting of memories
- Shorter, tightly contained sets for people who dissociate easily
Limits for dissociative disorders:
- EMDR must never be rushed for DID or severe dissociation.
- It should only be used when you’re relatively stable and have strong grounding and distress tolerance skills.
- Your therapist needs specific training in EMDR for dissociative disorders, or it can increase dissociation instead of reducing it.
In our programs, EMDR is one option among others—not a one-size-fits-all solution.
For more information about different types of dissociative disorders and their symptoms, the International Society for the Study of Trauma and Dissociation provides comprehensive resources and treatment guidelines.
Beyond Talk Therapy: Medication, Support, and Finding the Right Help
Recovery from dissociative disorders is not “just talk about your childhood and hope it works.” You need a full plan: targeted therapy, smart medication use, solid support, and practical logistics like insurance and scheduling.
What is the Role of Medication in Managing Dissociative Disorders?
There is no pill that cures dissociation, but medication can:
- Lower depression that keeps you in bed
- Calm anxiety and panic that trigger dissociation
- Stabilize mood swings that sabotage work, school, or relationships
Common options your psychiatrist might use:
- Antidepressants for depression, anxiety, and PTSD symptoms
- Anti-anxiety medications for short-term, acute anxiety or panic
- Mood stabilizers when there’s Bipolar Disorder or severe mood shifts
At Thrive, medication management is used to support therapy, not replace it—so you can fully engage in IOP/PHP groups, individual sessions, and skills practice.
What Should You Look for When Choosing a Therapist?
If you have a dissociative disorder, a generalist therapist is often not enough. You need someone who knows what they’re doing so you don’t waste years and money on the wrong approach.
Look for a therapist who:
- Specializes in trauma and dissociation (including DID)
- Is trauma-informed and respects pacing
- Can talk about ISSTD treatment guidelines in plain language
- Is comfortable with long-term work
- Feels like a good fit—calm, direct, and nonjudgmental
Good questions to ask in a consult:
- “What is your experience treating dissociative disorders and DID?”
- “What treatment model do you use (e.g., 3-phase, DBT, EMDR)?”
- “How do you keep clients safe when trauma work gets intense?”
- “Are you familiar with ISSTD guidelines?”
- “Do you accept my insurance (Cigna, Optum, Florida Blue, etc.)?”
If you’re in Florida, our virtual and hybrid IOP/PHP programs can often start within days, and we’ll help you verify coverage quickly.
How Do Cultural Factors Influence Dissociative Disorder Treatment?
Culture shapes how you understand and express distress. What looks like a dissociative disorder in one setting might be seen as:
- Spirit possession
- Trance states
- Culturally accepted rituals
A culturally competent therapist will:
- Ask about your beliefs and spiritual background
- Avoid pathologizing culturally normal experiences
- Adapt language and tools to fit your values and community
That cultural fit matters. When you feel understood, you’re more likely to stay in treatment long enough to get real results.
Frequently Asked Questions About Dissociative Disorder Treatment
Can adults fully recover from dissociative disorders?
Some adults do reach full integration and minimal to no symptoms. Others still have some dissociation but gain strong control, fewer crises, and stable work and relationships. With the right diagnosis and long-term, specialized care, recovery is very possible.
How long does treatment for dissociative disorders usually take?
Most people need years, not months. It takes time to build trust, stabilize safety, learn skills, and carefully process trauma. A lot of adults move through different levels of care—weekly therapy, then IOP/PHP, then back to weekly—to match what they need at each stage.
Which treatment approaches help adults with dissociative disorders recover the fastest?
There is no shortcut, but people tend to improve faster with:
- Phase-oriented therapy (safety → trauma work → integration)
- Skills-based approaches like DBT
- Carefully adapted CBT or EMDR
- Higher levels of care like IOP/PHP, especially when weekly therapy hasn’t been enough
How do I know if I need IOP or PHP instead of just weekly therapy?
Consider IOP/PHP if you:
- Have frequent dissociation, self-harm urges, or suicidal thoughts
- Can’t keep up with work, school, or parenting
- Keep landing in the ER or hospital
- Feel like weekly therapy isn’t moving the needle
Our remote mental health support page explains program options, schedules, and insurance in detail.
Is treatment for dissociative disorders covered by insurance?
Often yes. Many Cigna, Optum, Florida Blue, and other commercial plans cover IOP, PHP, and outpatient therapy when medically necessary. Coverage varies by state and plan, so it’s worth having us check benefits for Florida.
Conclusion: Which Treatment Approaches Help Adults With Dissociative Disorders Recover—And What You Can Do Today
The treatment approaches that help adults with dissociative disorders recover aren’t random. They follow a clear pattern:
- Phase-based psychotherapy to stabilize, process trauma, and integrate
- Skills-first work (DBT, grounding, distress tolerance) to cut crises
- Targeted trauma therapies (CBT, EMDR, psychodynamic) at the right time
- Medication support for depression, anxiety, and mood swings
- Specialized, trauma-informed providers who understand dissociation
Used together, these tools can mean:
- Fewer hospitalizations and ER trips
- Less time lost to dissociation
- More steady work, school, and relationships
- A life driven by choice, not just survival
If you’re in Florida, you don’t have to move states or sit on a waitlist for months to get serious help. Thrive offers virtual and hybrid IOP/PHP programs, accepts many major insurers (including Cigna, Optum, and Florida Blue), and is built specifically for adults dealing with complex trauma and dissociation.
Ready for support? Thrive offers virtual and hybrid IOP/PHP programs with evening options. Verify your insurance in 2 minutes (no obligation) → Start benefits check or call 561-203-6085. If you’re in crisis, call/text 988.