Detailed Reviews of the Top 10 Dual-Diagnosis Services

If you or a loved one are in crisis or considering self-harm, please call or text 988 to reach the Suicide & Crisis Lifeline. You are not alone.
Which Premier Services Support Dual-Diagnosis Treatment? [The 2025 Guide]
Which premier services support dual-diagnosis mental health treatment? The answer matters more than you think—because treating mental health or addiction separately leads to relapse rates as high as 60-90%. Here’s what you need to know right now:
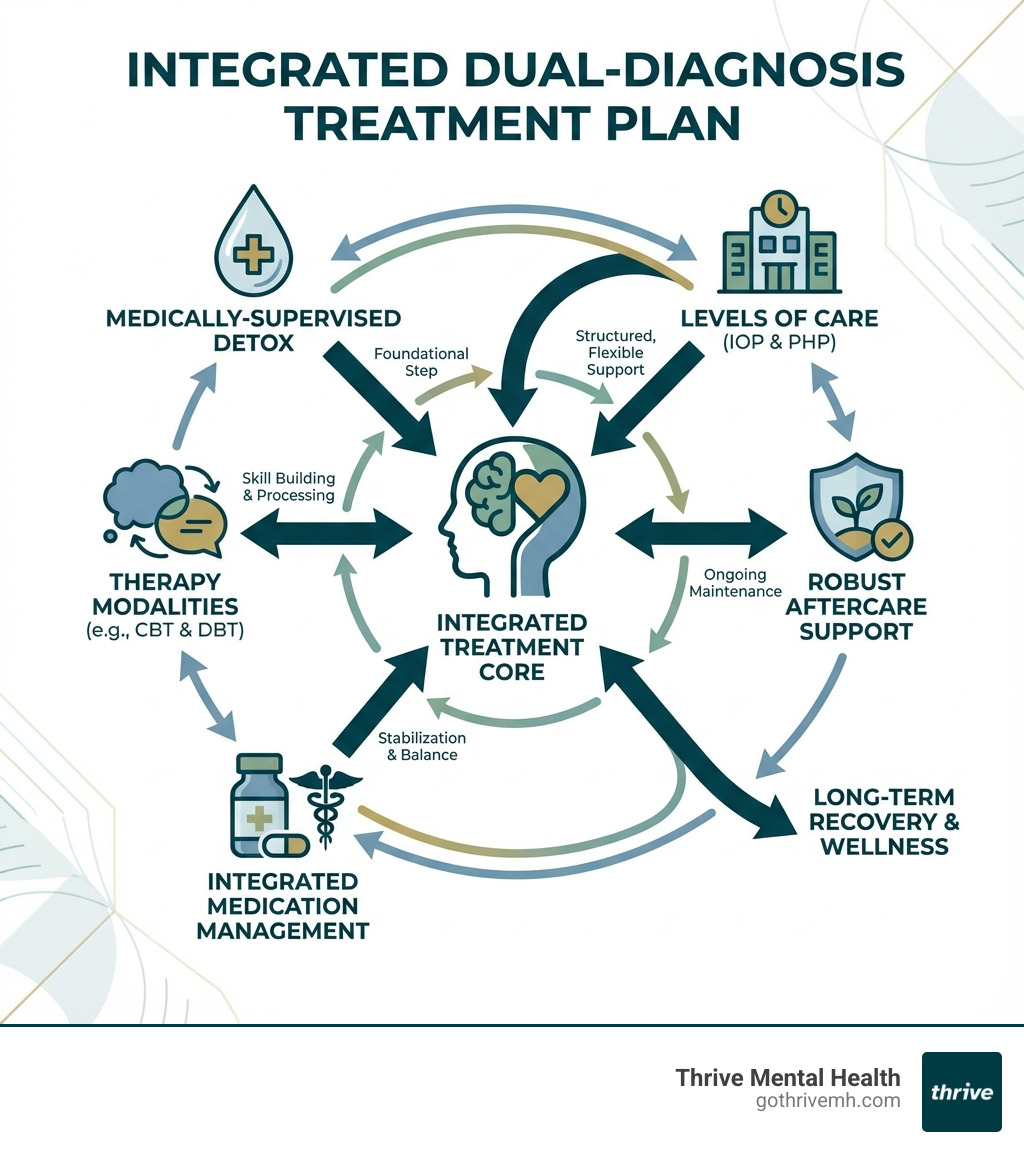
Top 7 Premier Dual-Diagnosis Services (2025):
- Medically-Supervised Detox – Safe withdrawal with 24/7 medical oversight
- Inpatient Rehab – Immersive, round-the-clock care for severe cases
- Partial Hospitalization (PHP) – Intensive day treatment without residential stay
- Intensive Outpatient (IOP) – Flexible care that fits work and family schedules
- Virtual IOP/PHP – Elite care delivered remotely across state lines
- Integrated Medication Management – Psychiatric care coordinated with addiction treatment
- Robust Aftercare Programs – Long-term support to prevent relapse
The hard truth: only 12.7% of people with dual diagnosis receive treatment for both conditions. The rest get stuck in a cycle where untreated depression fuels substance use, which worsens anxiety, which triggers more use. It’s a loop that kills progress—and sometimes people.
Dual diagnosis means you’re battling both a mental health disorder (like depression, anxiety, PTSD, or bipolar disorder) and a substance use disorder at the same time. Research shows these conditions share root causes—trauma, genetics, brain chemistry—and they amplify each other. Trying to treat just one is like bailing water from a sinking boat without patching the hole.
The good news? Integrated treatment—where one team addresses both your mental health and addiction simultaneously—delivers better long-term outcomes than fragmented care. Studies confirm it. Patients confirm it. The data is clear.
But not all “dual-diagnosis programs” are created equal. Some facilities slap the label on basic services without the structure, staffing, or evidence-based protocols that actually work. This guide cuts through the noise and shows you which premier services support dual-diagnosis mental health treatment with measurable results—not just promises.
I’m Nate Raine, CEO of Thrive Mental Health, and over the past decade I’ve built integrated behavioral health programs across Florida, combining clinical excellence with data-driven outcomes. My focus on which premier services support dual-diagnosis mental health treatment comes from seeing what works in real time—personalized IOP/PHP programs that blend virtual access, medication management, and trauma-informed care into one coordinated plan.
What is Dual Diagnosis? (And Why Treating Just One Fails Every Time)
If you’re reading this, chances are you or someone you care about is struggling with more than one battle. That’s where the term dual diagnosis comes in. It refers to the simultaneous presence of a mental health disorder and a substance use disorder (SUD) in an individual. Think of it this way: it’s not just about battling depression, anxiety, or PTSD, but also struggling with an alcohol dependency, opioid addiction, or stimulant misuse at the same time. This is also often referred to as co-occurring disorders.
Why is this so critical? Because these conditions don’t exist in isolation; they feed each other. Mental health symptoms can often drive substance use, as individuals might turn to drugs or alcohol to “self-medicate” their pain, anxiety, or emotional distress. This temporary relief, however, often leads to a worsening of the mental health condition and the development of an SUD. Conversely, substance use can trigger or exacerbate mental health disorders, creating a vicious cycle that’s incredibly hard to break. Research by the National Institute on Drug Abuse (NIDA) highlights this complex interplay, emphasizing that mental and substance use disorders often occur together, sharing common risk factors like genetics, stress, and trauma.
Consider these sobering facts:
- In 2020, 6.7% of U.S. adults (17 million people) suffered from co-occurring mental illness and substance use disorder.
- More than 25% of people who experience SUDs also struggle with mental health disorders.
The core problem with treating just one condition is that you’re leaving the other untreated, which inevitably undermines any progress made. If you treat the addiction but ignore the underlying anxiety, that anxiety will likely trigger a relapse. If you treat the depression but don’t address the alcohol use, the alcohol will continue to interfere with your mood and medication, making sustained recovery impossible. This is why integrated care, which addresses both conditions simultaneously, is not just preferred, but essential for long-term healing and stability. Studies confirm that integrated treatment leads to significantly better long-term outcomes than treating each disorder separately. It’s about patching all the holes in the boat, not just one.
The 7 Non-Negotiable Features of a “Premier” Dual-Diagnosis Program
When we talk about which premier services support dual-diagnosis mental health treatment, we’re not just looking for any program that claims to help. We’re looking for those that embody a specific, effective philosophy backed by science and real-world results. Here are the non-negotiable features:
- Integrated Care Philosophy: This is the cornerstone. A premier program treats both mental health and substance use disorders as interconnected parts of a single challenge, not two separate problems. This means you have one treatment team working collaboratively, ensuring all aspects of your well-being are addressed in a unified, coordinated approach.
- Comprehensive Assessment and Diagnosis: Before any treatment begins, a premier service conducts an in-depth, multidisciplinary assessment. This includes using diagnostic criteria from the DSM-5 for both SUDs and mental health conditions. They’ll use tools like DAST-10 or AUDIT for substance use and MMSE or DASS for mental health, gathering a full picture of your history, symptoms, and needs. This ensures an accurate diagnosis and a truly personalized treatment plan.
- Evidence-Based Therapies: Effective treatment relies on proven methods. Premier programs offer a range of therapeutic modalities shown to be effective for co-occurring disorders, including:
- Cognitive Behavioral Therapy (CBT): Helps you identify and change negative thought patterns and behaviors that contribute to both conditions.
- Dialectical Behavior Therapy (DBT): Focuses on emotional regulation, distress tolerance, interpersonal effectiveness, and mindfulness, particularly helpful for individuals with intense emotional swings and impulsive behaviors.
- Trauma-Informed Therapy (like EMDR): Addresses underlying trauma, which is often a significant factor in dual diagnosis. This approach recognizes the widespread impact of trauma and integrates this understanding into all aspects of treatment.
- Motivational Interviewing: Helps you explore and resolve ambivalence about change, strengthening your commitment to recovery.
- Psychiatric Medication Management: For many with dual diagnosis, medication is a critical component. Premier services include board-certified psychiatrists or psychiatric nurse practitioners who can prescribe and manage medications (antidepressants, mood stabilizers, anti-anxiety meds) to stabilize mental health symptoms, as well as Medication-Assisted Treatment (MAT) for addiction. This coordinated approach ensures medications work synergistically with therapy.
- Full Continuum of Care: Recovery isn’t a single event; it’s a journey. A premier program offers a seamless transition between different levels of care, including:
- Detoxification: Safe, medically supervised withdrawal.
- Inpatient Rehab: Intensive, 24/7 care.
- Partial Hospitalization Programs (PHP): Day treatment with strong clinical support.
- Intensive Outpatient Programs (IOP): Flexible treatment allowing you to live at home.
- Aftercare Planning: Ongoing support to prevent relapse.
- Family Therapy and Support: Dual diagnosis impacts the entire family system. Premier programs involve family members in the treatment process through education, communication skill-building, and support sessions. This promotes understanding, reduces conflict, and builds a stronger support network crucial for long-term recovery.
- Measurable Outcomes and Personalized Plans: No two individuals are alike. Premier programs create highly individualized treatment plans based on your unique needs, strengths, and goals. They also track outcomes to ensure the treatment is effective and make adjustments as needed. This data-driven approach ensures you’re on the most efficient path to lasting wellness.
Which premier services support dual-diagnosis mental health treatment? [Our 2025 Top 7]
Navigating the landscape of dual-diagnosis treatment can feel overwhelming. To cut through the noise, we’ve identified the top 7 premier services that consistently deliver effective, integrated care. These services represent the gold standard in supporting individuals battling co-occurring mental health and substance use disorders.

1. Medically-Supervised Detox: The Foundation for Safe Recovery
For many, especially those with significant physical dependence, detox is the essential first step. A medically-supervised detox provides a safe and controlled environment to manage withdrawal symptoms, which can range from uncomfortable to life-threatening. This service includes 24/7 medical care from doctors and nurses who monitor your vital signs and administer Medication-Assisted Treatment (MAT) to ease discomfort and prevent complications.
Why it’s premier: It’s not just about getting substances out of your system; it’s about doing it safely and preparing you mentally and physically for the therapeutic work ahead.
Common substances requiring detox:
- Alcohol
- Opioids (heroin, fentanyl, prescription painkillers)
- Benzodiazepines (Xanax, Valium, Klonopin)
- Sedatives and Hypnotics
2. Inpatient Rehab: For Immersive, 24/7 Healing
Inpatient rehabilitation offers an immersive, structured environment removed from the daily triggers and stressors of life. It’s ideal for individuals with severe symptoms, a high risk of relapse, or those needing crisis stabilization.
Why it’s premier: You’re completely focused on healing, with 24/7 structure and support. This level of care provides intensive daily therapy—both individual and group—peer support, and constant clinical oversight. It’s a powerful way to break negative patterns and build a strong foundation for recovery.
3. Partial Hospitalization (PHP): Intensive Care Without Living In
Partial Hospitalization Programs (PHPs) provide the intensity of inpatient care without requiring an overnight stay. Often referred to as “day treatment,” PHPs involve several hours of therapy and clinical services each day, typically five days a week.
Why it’s premier: PHPs are a crucial step-down from residential treatment or a starting point for those needing significant support but who have a stable home environment. You return home in the evenings, allowing you to gradually reintegrate into your life while still receiving robust clinical care. Our PHPs at Thrive Mental Health, available in Florida locations like Tampa Bay and Orlando, offer this intensive support, combining individual and group counseling to address both mental health and substance use concurrently.
4. Intensive Outpatient (IOP): Real-World Recovery That Fits Your Schedule
Intensive Outpatient Programs (IOPs) offer a flexible yet structured approach to dual diagnosis treatment. You attend several hours of therapy per week (typically 9-15 hours), allowing you to live at home and continue with work, school, or family responsibilities.
Why it’s premier: IOPs are designed for real-world application. You learn coping skills and strategies in therapy sessions and then immediately apply them in your daily life. This level of care is more affordable than inpatient options and helps you build a sustainable recovery while maintaining your commitments. At Thrive Mental Health, we offer flexible IOP schedules, including evening programs, across our locations throughout Florida, making it easier to prioritize your healing without putting your life on hold.
5. Virtual IOP/PHP: Get Elite Care from Anywhere
The rise of telehealth has revolutionized access to premier dual-diagnosis treatment. Virtual IOP/PHP programs deliver the same high-quality, evidence-based care as in-person programs, but from the comfort and privacy of your own home.
Why it’s premier: This option offers unparalleled accessibility and flexible scheduling, making it ideal for professionals, parents, or individuals in rural areas who might otherwise struggle to access specialized care. We’ve seen how virtual programs remove barriers, allowing people to engage deeply in their recovery journey. Our virtual IOP/PHP services at Thrive Mental Health extend across the state of Florida, ensuring you can receive elite care regardless of your physical location.

6. Integrated Medication Management: Treating Mind and Body Together
For many with dual diagnosis, medication is a vital tool for stabilizing mental health symptoms and supporting sobriety. Premier services include comprehensive integrated medication management.
Why it’s premier: This holistic approach involves psychiatric oversight, where qualified professionals (psychiatrists, psychiatric nurse practitioners) prescribe and monitor medications. This might include:
- Antidepressants for depression
- Mood stabilizers for bipolar disorder
- Anti-anxiety medications for anxiety disorders
- Medication-Assisted Treatment (MAT) for substance use disorders, such as Vivitrol (for alcohol and opioid dependence) or Suboxone (for opioid dependence).
The key is coordinated care, ensuring that all medications work together and with your therapy to achieve the best possible outcomes, as highlighted by resources like Dual Diagnosis.
7. Robust Aftercare Programs: Your Plan for Lasting Sobriety
Treatment doesn’t end when a program concludes. Premier dual-diagnosis services understand that long-term recovery requires ongoing support.
Why it’s premier: A robust aftercare plan is your roadmap for maintaining sobriety and managing mental health symptoms post-treatment. This includes:
- Relapse prevention strategies
- Access to alumni groups and a supportive community
- Recommendations for sober living arrangements
- Guidance on step-down therapy (e.g., transitioning from IOP to weekly individual therapy)
- Connections to local support groups like Dual Diagnosis Anonymous (DDA) or Double Trouble in Recovery (DTR).
This continuous support is crucial for preventing relapse and fostering sustained wellness.
How to Choose a Program That Actually Works for You
Choosing the right dual-diagnosis treatment program is one of the most important decisions you’ll make. With so many options, how do you ensure you’re picking a “premier” service that genuinely meets your needs and sets you up for success?
How do I know which premier services support dual-diagnosis mental health treatment best for my needs?
Here’s a checklist of what to look for and questions to ask:
- Accreditation Matters: Look for programs accredited by reputable organizations like The Joint Commission (JCAHO) or the Commission on Accreditation of Rehabilitation Facilities (CARF). These accreditations signify that the facility meets rigorous standards for quality and safety.
- Insurance Verification & Cost: Don’t let cost be a barrier. Most major insurance providers, including Cigna, Optum, Aetna, and Florida Blue (common in our service areas), offer coverage for dual-diagnosis treatment thanks to federal parity laws. Always verify your specific benefits with the provider. Many premier services also offer self-pay options or can help you explore financing.
- Location vs. Virtual Access: Consider whether an in-person program or a virtual program best fits your lifestyle.
- In-person: For those who thrive in a structured, physical environment, our centers in Florida (including Tampa Bay, Miami, Orlando, Boca Raton, West Palm Beach, Jacksonville, Fort Lauderdale, Naples, and Sarasota) offer dedicated spaces for healing.
- Virtual: If flexibility, privacy, and accessibility are key, our virtual IOP/PHP programs allow you to receive top-tier care from anywhere in Florida. This is especially beneficial for individuals balancing work, family, or other commitments.
- Staff Qualifications: A truly premier program employs a multidisciplinary team of highly qualified professionals. This often includes psychiatrists, psychologists, licensed therapists (LCSW, LMFT, LPCC), addiction counselors, and medical staff. Ask about their experience in treating co-occurring disorders.
- Personalized Treatment, Not One-Size-Fits-All: Your journey is unique. A premier program will conduct a thorough assessment and develop a treatment plan custom specifically to your dual diagnosis, co-occurring medical conditions, and life circumstances. Avoid programs that offer a generic approach.
- Family Involvement: Does the program offer family sessions or educational resources for loved ones? Strong family support significantly improves long-term outcomes.
- Aftercare Planning: A good program doesn’t just treat you; it prepares you for life after treatment. Inquire about their aftercare planning process and ongoing support options.
Frequently Asked Questions about Premier Dual-Diagnosis Treatment
How long does dual-diagnosis treatment take?
There’s no single answer, as the duration of dual-diagnosis treatment is highly individualized. It depends on the severity of your conditions, your response to treatment, and the level of care you’re receiving.
- Detox: Typically lasts 5-7 days.
- Inpatient Rehab: Can range from 30 to 90 days, sometimes longer.
- PHP (Partial Hospitalization): Often lasts 2-4 weeks, or longer if needed, before stepping down.
- IOP (Intensive Outpatient): Can be 4-12 weeks, with some individuals benefiting from longer-term participation.
Recovery from dual diagnosis is a lifelong process. The initial treatment phases build a strong foundation, but ongoing self-care, support groups, and sometimes continued therapy are crucial for sustained wellness.
Which premier services support dual-diagnosis mental health treatment for teens vs. adults?
While the core principles of integrated care remain the same, premier services often offer specialized programs custom to specific age groups.
- Adult Programs: For adults and young professionals, programs like our IOP/PHP at Thrive Mental Health are designed with an understanding of adult responsibilities, career demands, and the complexities of adult relationships. They focus on developing coping strategies relevant to adult life and maintaining work/school commitments.
- Teen Programs: Teen-specific dual-diagnosis programs address developmental considerations, peer pressure, family dynamics unique to adolescence, and academic needs. Family involvement is key for all ages, but it’s especially critical in adolescent treatment to ensure a supportive home environment.
It’s important to find a program that specifically caters to the age group, as their therapeutic approaches, group dynamics, and overall environment will be optimized for that demographic.
Can I use my insurance for dual-diagnosis treatment?
Yes, in most cases, you can use your insurance for dual-diagnosis treatment! Thanks to federal laws like the Mental Health Parity and Addiction Equity Act (MHPAEA) and the Affordable Care Act (ACA), most major insurance plans are required to cover mental health and substance use disorder treatment at the same level as medical or surgical care. This means your plan should cover integrated dual-diagnosis services.
We work with many major insurance providers, including Aetna, Cigna, Optum, Blue Cross Blue Shield, and Florida Blue. However, coverage can vary depending on your specific plan and benefits. That’s why we always recommend you verify your specific benefits with the treatment provider before starting. Our team can help you steer this process to understand your in-network vs. out-of-network options and minimize out-of-pocket costs.
Your Next Step: Getting Real Support That Fits Your Life
Navigating dual diagnosis is challenging, but with the right premier services, recovery is not just a possibility—it’s a reality we see every day. Integrated treatment is essential, providing a path to lasting hope and healing by addressing both your mental health and substance use disorders concurrently.
At Thrive Mental Health, we are dedicated to offering premier virtual and in-person IOP/PHP programs designed for adults and young professionals who need more than once-a-week therapy but less than inpatient care. Our flexible evening options, combined with clinical expertise and a focus on measurable results, ensure you get the support you need, when and where you need it.
Ready for support? Thrive offers virtual and hybrid IOP/PHP programs with evening options. Verify your insurance in 2 minutes (no obligation) → Start benefits check or call 561-203-6085. If you’re in crisis, call/text 988.