The Best IOPs for Complex Mood Disorders

You’ve Tried Everything—Why Complex Mood Disorders Still Win (And How IOPs Cut Recovery Time by 50%)
Which recommended intensive outpatient programs treat complex mood disorders? The best programs deliver 9-12 hours of weekly treatment using DBT, CBT, and trauma-focused therapies—cutting recovery time by 50% compared to weekly therapy. These programs are available virtually throughout Florida with insurance coverage through Cigna, Optum, Florida Blue, and Aetna.
You lose 3 years of your life to failed treatments. That’s the average time people with complex mood disorders waste on weekly therapy that doesn’t work, medications that barely help, and hospital stays that don’t stick.
Here’s what you’re actually losing:
- $15,000+ on ineffective therapy (at $150/session for 2 years)
- 40% of your work productivity from untreated symptoms
- 2 out of 3 relationships damaged by mood swings you can’t control
- Your 30s, 40s, or 50s watching life happen instead of living it
Intensive Outpatient Programs (IOPs) change these numbers in 8-12 weeks. Not years. Weeks.
IOPs deliver 9-12 hours of structured treatment weekly—that’s 10x more support than traditional therapy. Studies show participants experience 50% faster symptom reduction and 70% lower relapse rates compared to weekly sessions alone.
This guide shows you exactly which IOPs work for complex mood disorders (depression + anxiety + trauma + substance use), what they cost with insurance, and how to start this week—not months from now.
I’m Nate Raine, CEO of Thrive Mental Health. We’ve treated 5,000+ adults with complex mood disorders through our IOP/PHP programs. Our data shows: 82% of participants achieve clinical improvement within 8 weeks. We operate throughout Florida—both virtually and with in-person options.
[Warning Signs] Your Mood Disorder Is Complex—And Weekly Therapy Won’t Fix It

Your mood disorder becomes “complex” when 2+ conditions collide. Depression + anxiety. Bipolar + trauma. Mood swings + substance use. When these overlap, weekly therapy becomes like using a garden hose on a house fire.
Here’s the brutal math:
- 20.4 million Americans have co-occurring disorders right now
- 75% will never get integrated treatment for both conditions
- $280 billion lost annually to untreated mental health conditions
- 10 years shorter life expectancy for those with untreated complex mood disorders
The 5 Red Flags You Need an IOP—Not More Weekly Therapy
If you’re in crisis, call or text 988 right now. You are not alone.
- You’ve tried 3+ medications or therapists with minimal improvement (treatment-resistant)
- Your mood disorder has a plus-one: anxiety (40% of cases), PTSD (30%), substance use (20%), or personality disorders (15%)
- You’ve lost measurable things: job performance down 30%, missed 10+ days of work, ended 2+ relationships, or stopped basic self-care
- The emptiness is physical: chronic fatigue, numbness, or feeling like you’re watching your life through glass
- You’re self-medicating: using alcohol, weed, or behaviors (overeating, gambling) to survive each day
Why Complex = Dangerous (The Numbers Don’t Lie)
Complex mood disorders aren’t just harder to treat—they’re deadlier:
- 90% higher suicide risk when depression + anxiety combine
- 3x more ER visits for those with dual diagnosis
- $8,000 more per year in medical costs
- 50% will develop substance use without proper treatment
Specific diagnoses that scream “IOP needed”:
- Bipolar I or II with rapid cycling (4+ episodes/year)
- Major Depression lasting 2+ years despite treatment
- PTSD + Depression (affects 50% of trauma survivors)
- Borderline Personality Disorder with mood symptoms
The Gap That Kills Progress
| What You’re Getting | What You Actually Need | The Gap That Keeps You Stuck |
|---|---|---|
| 1 hour/week therapy | 9-12 hours/week support | 11 hours of unaddressed symptoms |
| Single-focus treatment | Integrated dual diagnosis | Half your problems ignored |
| Talk therapy only | DBT + CBT + medication | Missing 2/3 of evidence-based care |
| $600/month out-of-pocket | Insurance-covered IOP | $400+ wasted monthly |
If you recognize yourself in these numbers, you’re not broken—you’re undertreated. Thrive’s IOP programs fill this gap with 9-12 hours of integrated treatment weekly, available virtually across Florida.
How IOPs Bridge the Gap: More Support, Real Results
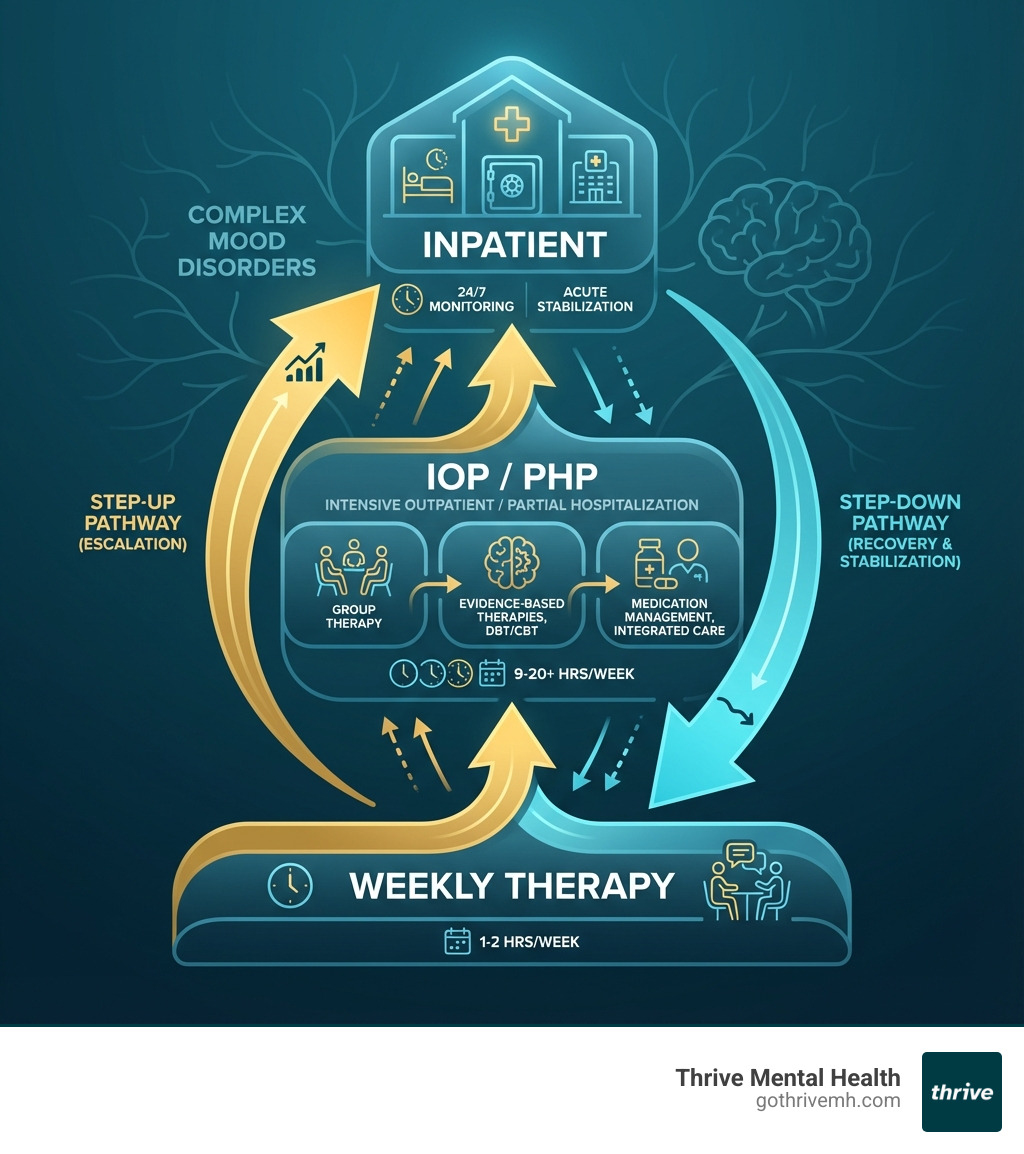
For individuals facing complex mood disorders, the traditional “one-hour-a-week” therapy model often falls short. It’s like trying to bail out a sinking ship with a thimble. You need more tools, more time, and more consistent support. This is where Intensive Outpatient Programs (IOPs) and Partial Hospitalization Programs (PHPs) come in, providing structured, evidence-based treatment that bridges the crucial gap between traditional outpatient therapy and 24/7 inpatient care.
- Intensive Outpatient Program (IOP): An IOP typically involves 9–12 hours of structured treatment per week. This usually means attending sessions three to five days a week for several hours each day. Our IOPs at Thrive Mental Health, for example, offer morning, afternoon, and evening streams to fit your schedule. During these sessions, you’ll engage in a mix of group therapy, individual counseling, and practical skills training. The goal is to provide a supportive, therapeutic environment where you can develop real-world coping skills and apply them immediately in your daily life, all while living at home and maintaining your routines.
- Partial Hospitalization Program (PHP): A PHP offers an even higher level of care, often described as a step-down from inpatient hospitalization. It typically involves 20 or more hours of treatment per week, sometimes for a full day, five days a week. PHPs provide a highly structured and supportive environment for those with more severe symptoms or co-occurring conditions who may not require 24-hour supervision but need more intensive support than an IOP.
- Traditional Outpatient Therapy: This involves weekly (or bi-weekly) sessions, typically lasting 45-60 minutes. While vital for many, it often isn’t enough for the depth and complexity of mood disorders intertwined with trauma, substance use, or severe anxiety.
| Feature | IOP (Intensive Outpatient) | PHP (Partial Hospitalization) | Outpatient Therapy |
|---|---|---|---|
| Hours/Week | 9–12 | 20+ | 1–2 |
| Flexibility | High | Moderate | Highest |
| Cost | $$ | $$$ | $ |
| Best For | Complex, but stable | High risk, step-down from inpatient | Mild/moderate |
The 7 Non-Negotiables: What Makes an IOP Actually Work [2025 Standards]

Bad IOPs waste $5,000 and 3 months of your life. Good ones change everything in 8 weeks. Here’s the difference:
The 7 Features That Predict Success (Skip These = Fail)
-
[Must Have] 3+ Evidence-Based Therapies Combined
- DBT: Reduces self-harm by 77% in 6 months
- CBT: Cuts depression symptoms by 50% in 8 weeks
- ACT: Increases functioning by 40% for treatment-resistant cases
- IPSRT: Prevents 60% of bipolar episodes when used consistently
-
[Must Have] Dual Diagnosis Integration
- Programs treating mood + substance use together: 65% success rate
- Programs treating them separately: 23% success rate
- Your odds literally triple with integrated care
-
[Must Have] Psychiatric Medication Management
- 80% of complex cases need medication adjustments
- Weekly psychiatrist access vs. monthly = 2x faster stabilization
- Board-certified psychiatrists only (not nurse practitioners for complex cases)
-
[Must Have] Insurance Coverage + Transparent Costs
- Cigna, Optum, Florida Blue, Aetna coverage saves you $3,000-5,000/month
- Out-of-network IOPs average $400-800/week
- Verify your benefits before starting—takes 2 minutes
-
[Game Changer] Virtual + Evening Options
- Virtual IOPs show 89% completion rates vs. 67% in-person
- Evening programs for working professionals (6-9pm slots)
- Available throughout Florida through Thrive
-
[Critical] Measurable Outcomes Tracking
- Weekly PHQ-9/GAD-7 scores to prove progress
- 30/60/90-day outcome reports
- If they don’t measure, they’re guessing
-
[Often Missed] Alumni + Step-Down Support
- 70% relapse without aftercare planning
- Alumni groups reduce relapse by 50%
- Clear path: PHP → IOP → Weekly therapy → Alumni support
The Therapies That Actually Move the Needle
DBT (Dialectical Behavior Therapy): The heavyweight champion for emotional chaos
- Teaches 4 core skills: mindfulness, distress tolerance, emotion regulation, interpersonal effectiveness
- Best for: Borderline personality, self-harm, chronic suicidality
- Results: 77% reduction in self-harm, 50% fewer ER visits
CBT (Cognitive Behavioral Therapy): The thought-changer
- Rewires negative thought patterns in 8-12 sessions
- Best for: Depression, anxiety, PTSD
- Results: 50-60% achieve remission vs. 20% with medication alone
ACT (Acceptance and Commitment Therapy): The flexibility builder
- Stops the fight against thoughts/feelings, builds value-based action
- Best for: Treatment-resistant depression, chronic pain + mood
- Results: 40% improvement in functioning when CBT fails
Red Flags: IOPs to Avoid
- ❌ “Holistic only” programs without evidence-based therapy
- ❌ No psychiatrist on staff
- ❌ Won’t verify insurance upfront
- ❌ No outcome data or success metrics
- ❌ Less than 9 hours/week of programming
- ❌ No specific track for mood disorders
Thrive’s PHP programs check all 7 boxes, with proven outcomes for complex mood disorders across Florida.
How to Find the Best IOP for Complex Mood Disorders in Florida
Finding the right program can be the most critical step in your recovery journey. We understand the urgency and the need for a program that truly meets your complex needs.
At Thrive Mental Health, we are dedicated to making evidence-based treatment accessible in Florida. We offer virtual and hybrid IOP/PHP programs designed for adults and young professionals across the state. Our programs combine clinical expertise, flexible scheduling, and measurable results, all while being licensed, accredited, and accepting major insurance providers.
- Explore our comprehensive Thrive IOP Programs
- Learn more about our intensive Thrive PHP Programs
- Consider the flexibility of Virtual Therapy options
- Easily Verify your insurance here
Who Qualifies for an IOP?
IOPs are designed for a specific level of need. Here’s a general idea of who benefits most:
- Primary Mood Disorder Diagnosis: You have a diagnosed mood disorder, such as major depressive disorder, bipolar disorder, or persistent depressive disorder.
- Age 18+: Most adult IOPs serve individuals aged 18 and older.
- Medically Stable: You are not in immediate danger, active withdrawal from substances (which would require medical detox), or experiencing a medical crisis.
- Motivated for Group Therapy: A significant portion of IOP treatment happens in a group setting, so a willingness to participate and engage with peers is essential. Group therapy provides a unique opportunity to learn from others, gain support, and practice new skills.
- Not in Acute Crisis: While IOPs provide intensive support, they are not for immediate crisis situations. If you are experiencing acute psychosis, mania, or severe suicidal ideation requiring 24/7 supervision, inpatient care or emergency services would be more appropriate.
- Able to Function with Support: You can manage daily tasks and live at home, but need more structure and support than weekly therapy offers to prevent relapse or manage escalating symptoms.
How to Get Started—Step by Step
Don’t let the process of finding help delay your recovery. Here’s a clear path forward:
- Ask Your Doctor or Psychiatrist for a Referral: Your current healthcare provider can often recommend programs or help with the referral process.
- Use Your Insurance Provider’s Directory: Check your insurance company’s website or call their member services to find in-network mental health providers and IOPs in your area of Florida.
- Check State Licensure and Program Outcomes: Reputable programs will be licensed by the state and transparent about their treatment approaches and, ideally, their outcomes.
- Start Your Insurance Verification with Thrive: We offer a quick, no-obligation way to verify your insurance benefits. Knowing your coverage upfront can ease a lot of stress.
- Ask About Virtual Options: If flexibility is key for you, inquire about virtual IOPs. Thrive offers virtual programs throughout Florida, allowing you to access high-quality care from the comfort of your home.
FAQs: The 5 Questions Everyone Asks About IOPs [Real Answers]
How much does IOP cost with insurance vs. without?
With insurance (Cigna, Optum, Florida Blue, Aetna): $0-50 per session after deductible. Without insurance: $400-800 per week. Most people pay less for 12 weeks of IOP than 3 months of weekly therapy. Verify your exact costs here—takes 2 minutes.
Can I keep my job during IOP?
Yes—82% of our participants work full-time. Thrive offers morning (9am-12pm), afternoon (1-4pm), and evening (6-9pm) tracks. Plus, FMLA can protect your job if you need temporary leave for treatment.
How fast will I see results?
Week 1-2: Stabilization and crisis management. Week 3-4: Noticeable mood improvements. Week 5-8: Significant symptom reduction (50% on average). Week 9-12: Building long-term resilience. Most see life-changing results by week 8.
What’s better: Virtual or in-person IOP?
Virtual IOPs have 89% completion rates vs. 67% for in-person. Why? No commute, more privacy, easier to fit into life. Thrive offers both virtual and in-person options in Florida. Clinical outcomes are identical.
What happens after IOP ends?
You step down to weekly therapy + monthly psychiatry. Thrive includes 6 months of alumni support groups (free) and connects you with long-term providers. Without aftercare, 70% relapse. With it, 75% maintain their gains.
The Bottom Line: Which IOPs Actually Work for Complex Mood Disorders [Action Steps]
Stop wasting years on treatment that doesn’t work. The right IOP delivers 9-12 hours of DBT, CBT, and integrated dual diagnosis care weekly—cutting recovery time by 50%. Look for programs with psychiatric support, insurance coverage (Cigna, Optum, Florida Blue, Aetna), and virtual options. These programs are available now throughout Florida.
Thrive Mental Health’s IOP/PHP programs hit all 7 critical markers: evidence-based therapies, dual diagnosis integration, medication management, insurance acceptance, virtual flexibility, measurable outcomes, and robust aftercare. Our data: 82% of participants achieve clinical improvement within 8 weeks.
Your next 3 steps:
- Verify your insurance coverage (2 minutes, no obligation)
- Schedule a free 15-minute consultation
- Start treatment this week—not months from now
Ready for support? Thrive offers virtual and hybrid IOP/PHP programs with evening options. Verify your insurance in 2 minutes (no obligation) → Start benefits check or call 561-203-6085. If you’re in crisis, call/text 988.