Your Checklist for Mental Health IOP Enrollment

Is Weekly Therapy Not Enough? Here’s What’s Next.
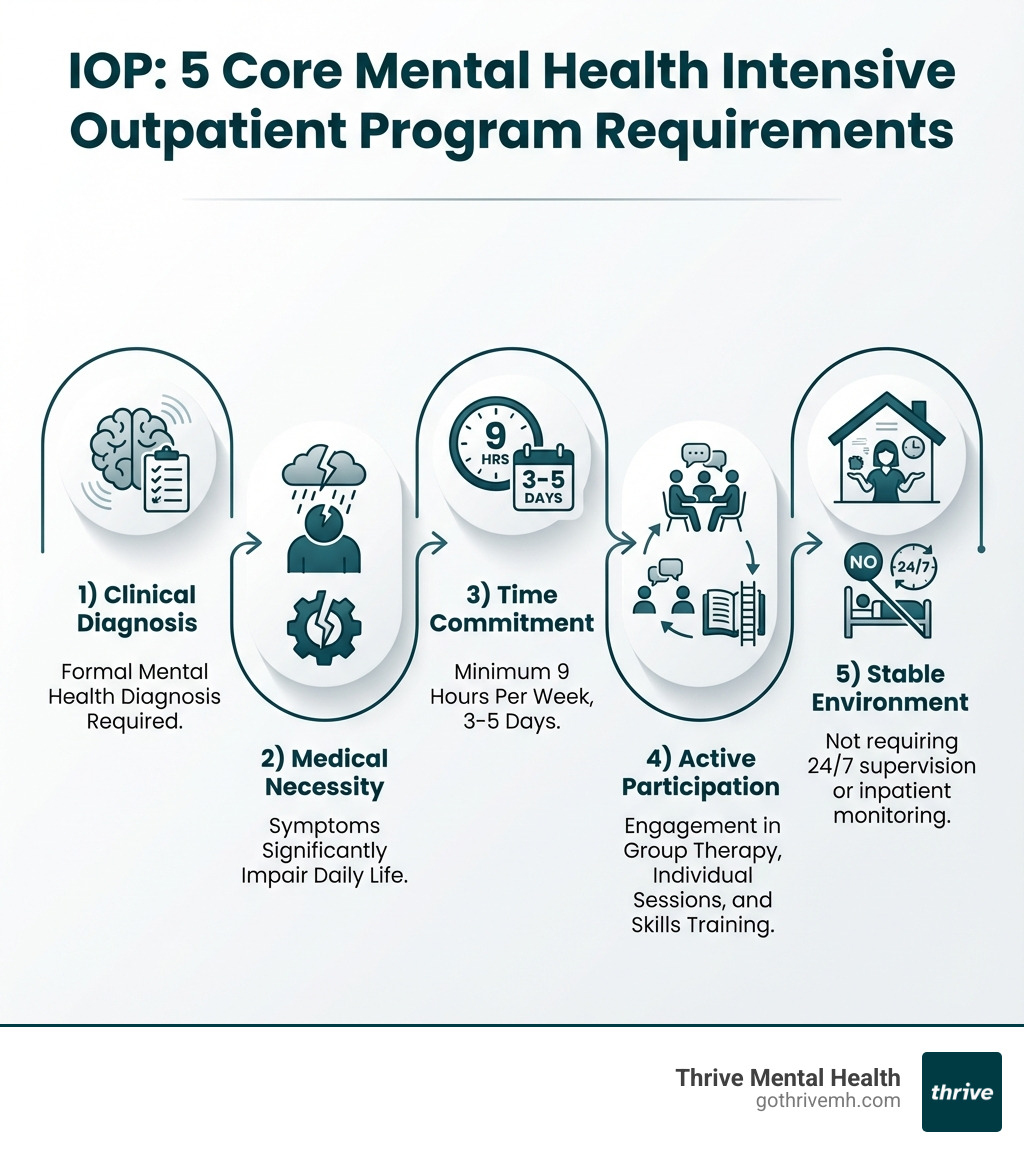
Mental health intensive outpatient program requirements vary by provider, but most programs share five core eligibility standards:
- Clinical Diagnosis – A formal mental health diagnosis from a licensed clinician (such as depression, anxiety, PTSD, or bipolar disorder)
- Medical Necessity – Symptoms that significantly impair daily functioning and require more than weekly therapy
- Time Commitment – Ability to attend at least 9 hours of structured treatment per week (typically 3-5 days)
- Active Participation – Willingness to engage in group therapy, individual sessions, and skills training
- Stable Environment – Not requiring 24/7 supervision or inpatient-level medical monitoring
If you’ve been doing weekly therapy for months but still feel stuck—waking up anxious, avoiding work, or barely holding it together—you’re not failing. You just need more support than one hour a week can provide.
That’s where an Intensive Outpatient Program (IOP) comes in.
An IOP is a structured, evidence-based treatment program that offers multiple therapy sessions per week. It’s designed for people who need more than traditional outpatient care but don’t require round-the-clock supervision in a hospital or residential facility. You attend therapy sessions several times a week—often in the evening—while continuing to work, go to school, or manage daily responsibilities.
IOPs treat conditions like depression, anxiety, PTSD, bipolar disorder, and co-occurring substance use issues. They combine group therapy, individual counseling, skills training, and medication management into a comprehensive treatment plan. The goal is simple: stabilize your symptoms, build coping skills, and help you get back to living your life.
But before you can enroll, you need to meet certain requirements. These aren’t barriers—they’re guardrails to make sure an IOP is the right level of care for where you are right now.
As Nate Raine, CEO of Thrive Mental Health, I’ve spent over a decade building programs that meet mental health intensive outpatient program requirements while delivering measurable outcomes for people who need fast, flexible, evidence-based care. At Thrive, we’ve designed our IOPs to fit the lives of working professionals, students, and anyone balancing recovery with real-world responsibilities, with specialized programs available throughout Florida.
This guide breaks down exactly what you need to know—from clinical eligibility to insurance coverage to what your daily schedule will actually look like—so you can decide if an IOP is your next step toward recovery.
If you’re seeking to understand how do intensive outpatient programs work, how long are intensive outpatient programs, or if a program like ours can treat complex mood disorders, this guide is for you.
Are You a Candidate for an IOP? [The Initial Screen]
Feeling overwhelmed by daily life, even with regular therapy? You’re not alone. Many individuals find themselves in a mental health “middle ground”—they need more support than a weekly therapy session but don’t require the 24/7 supervision of an inpatient facility. If this sounds like you, an Intensive Outpatient Program (IOP) might be your ideal solution.
We often see individuals thrive in our IOPs who are struggling with moderate to severe mental health challenges that significantly impact their daily functioning. These are people who haven’t found adequate relief from traditional outpatient therapy or those transitioning from a higher level of care, like inpatient hospitalization. An IOP provides the structured support needed to prevent relapse and build sustainable coping mechanisms.
Our IOPs are designed to help with a wide array of conditions, including:
- Depression: When persistent sadness, loss of interest, and energy drain your life.
- Anxiety Disorders: From generalized anxiety to panic attacks, when worry becomes debilitating.
- PTSD: For those struggling with the aftermath of trauma, seeking to process experiences and regain control.
- Bipolar Disorder: Managing mood swings and maintaining stability within a supportive environment.
- Co-occurring Disorders: Addressing both mental health conditions and substance use issues simultaneously.
If you’re wondering what your options are for mental health treatment that’s more intensive than weekly therapy, but doesn’t require living at a facility, an IOP could be the bridge you need.
You might be a good fit for an IOP if:
- You need more support than once-a-week therapy. If your symptoms are worsening despite regular sessions, it’s a clear sign you need a step-up in care.
- You are on leave from work or school and want to focus on recovery. Many of our programs, including virtual options, are designed to accommodate your schedule, allowing you to prioritize your well-being without completely disrupting your life. More on taking work leave for mental health.
- Your symptoms are getting worse despite current treatment. This is a critical indicator that your current level of care is insufficient.
- You were recently discharged from a hospital and need to prevent relapse. IOPs offer a crucial step-down, providing continued structure and support as you reintegrate into daily life.
- You are stable and not a danger to yourself or others. IOPs are for individuals who can maintain safety in an outpatient setting, even if they’re struggling. If you’re experiencing active suicidal ideation or severe self-harm, a higher level of care might be recommended initially.
The Core Mental Health Intensive Outpatient Program Requirements You Must Meet
Once you’ve determined that an IOP might be the right fit, the next step is understanding the specific mental health intensive outpatient program requirements for admission. These criteria ensure that you receive the most appropriate and effective care for your needs.
Our intake process at Thrive Mental Health is designed to be comprehensive yet compassionate, guiding you through each step. For a general overview, you can also refer to our IOP Program Requirements page.
Clinical and Diagnostic Requirements
At the heart of IOP admission is a thorough clinical assessment. We need to understand your unique situation to tailor a treatment plan that truly works.
- Formal Diagnosis: You must have a formal mental health diagnosis from a licensed clinician. This diagnosis, such as severe depression, anxiety disorder, PTSD, or bipolar disorder, provides the foundation for your treatment plan.
- Medical Necessity: Your symptoms must demonstrate “medical necessity.” This means your mental health condition significantly impairs your daily functioning, and you require a higher level of care than traditional outpatient therapy can provide. It’s about showing that without intensive intervention, your condition would likely worsen or require a more restrictive environment. For a deeper understanding, explore what is medical necessity?.
- Psychosocial Assessment: A comprehensive psychosocial assessment will be conducted to understand your full history, current challenges, strengths, and potential barriers to recovery. This helps us determine where you are and how we can best support you.
- Stable Living Environment: You must have a stable living situation that allows you to safely participate in an outpatient program. This means you are not at imminent risk of harm to yourself or others and can manage daily responsibilities outside of program hours.
- Not Requiring 24/7 Supervision: IOPs are for individuals who do not require continuous supervision or intensive medical monitoring. If you’re experiencing a mental health crisis, we can help you connect with crisis intervention mental health services to ensure your immediate safety first.
Documentation and Admission Paperwork
Getting started with an IOP involves some essential paperwork. This process is straightforward and ensures we have all the necessary information to provide you with the best care.
- Initial Consultation: Your journey begins with an initial consultation with a licensed clinician. This is where we discuss your needs, assess your suitability for an IOP, and answer any questions you may have.
- Government-Issued ID: We’ll need a valid government-issued identification for verification purposes.
- Insurance Card: Your insurance information is crucial for verifying coverage and handling billing.
- Medical Records: Providing relevant medical records, especially those pertaining to your mental health history and any previous treatments, helps us understand your journey and inform your personalized treatment plan.
- Signed Consent Forms: You’ll sign consent forms for treatment, privacy practices, and other necessary agreements.
- Treatment Plan Agreement: We’ll work with you to develop an individualized treatment plan, outlining your goals, therapies, and expected outcomes. You’ll agree to this plan, which may also include your stated goals for therapy.
Insurance and Financial Mental Health Intensive Outpatient Program Requirements
Navigating insurance and financial aspects can feel daunting, but we’re here to help. Our goal is to make high-quality mental healthcare accessible.
- Verifying Benefits: We assist you in verifying your insurance benefits to understand your coverage for IOP services. This includes checking for deductibles, co-pays, and out-of-pocket maximums.
- Prior Authorization: Many insurance providers, including major carriers like Cigna, Aetna, Florida Blue, and UnitedHealthcare, require prior authorization for IOP services. Our team handles this process, submitting clinical documentation to demonstrate medical necessity.
- Co-pays and Deductibles: Like most medical services, you may be responsible for co-pays and deductibles, depending on your plan. We’ll help you understand these costs upfront.
- Medicare Part B Coverage: Good news for Medicare beneficiaries: Medicare Part B covers intensive outpatient program services. After meeting your Part B deductible, you typically pay 20% of the Medicare-approved amount. Our programs are designed to meet Medicare’s rigorous standards for covered services.
- In-network Providers: To ensure our programs are accessible, Thrive Mental Health is an in-network provider with a wide range of insurance plans across Florida. Understanding your coverage is key, and our Virtual IOP Insurance guide can offer more insights. For a comprehensive look at how to maximize your benefits, refer to how to read mental health insurance benefits.
Your Commitment: What Active Participation in an IOP Looks Like
An IOP isn’t a passive experience; it’s an active partnership in your recovery. Your commitment to engaging with the program is a crucial mental health intensive outpatient program requirement for success. We provide the structure and expert guidance, and you bring your willingness to learn, grow, and heal.

Our programs in Florida, whether virtual or in-person, are designed to integrate seamlessly into your life. To get a clearer picture of what your days might look like, explore what to expect in an intensive outpatient program.
Attendance: The 9-Hour Weekly Minimum
Consistency is key in an IOP. The intensity and frequency are what make these programs so effective.
- Time Commitment: IOPs typically require participants to attend at least 9 hours of therapeutic services per week. This usually translates to 3-5 days a week, with sessions lasting 2-4 hours per day. Some programs, particularly for substance use disorders, can range from 9 to 19 hours a week.
- Flexible Schedules: We understand you have a life outside of treatment. That’s why many of our IOPs offer evening and weekend options, specifically designed to accommodate work, school, and family commitments. We pride ourselves on offering intensive outpatient programs with flexible scheduling to fit your needs.
- Consistent Attendance: Regular attendance is non-negotiable. It’s how you build rapport with your peers and therapists, absorb new skills, and make consistent progress. Our programs typically last for 8-12 weeks, providing a focused, time-limited intervention.
Therapeutic Engagement: What’s Included in an IOP?
Our IOPs combine a variety of evidence-based therapies and services to provide holistic care.
- Group Therapy: This is often the cornerstone of an IOP, providing a powerful sense of community and shared experience. Led by trained therapists, these sessions allow you to learn from others, practice new skills, and receive invaluable peer support. Effective groups typically have 6-15 participants, creating a safe, intimate environment.
- Individual Therapy: Alongside group sessions, you’ll engage in one-on-one therapy. This provides a space for deeper exploration of personal issues, processing insights from group, and tailoring strategies to your unique needs.
- Dialectical Behavior Therapy (DBT) and Cognitive Behavioral Therapy (CBT): We use proven modalities like DBT, which focuses on emotional regulation, distress tolerance, interpersonal effectiveness, and mindfulness, and A Beginner’s Guide to Cognitive Behavioral Therapy (CBT), which helps you identify and change unhelpful thought patterns.
- Medication Management: For many, medication is a vital component of mental health treatment. Our IOPs include psychiatric evaluations and medication management, ensuring your mental health needs are addressed holistically. Psychiatrist visits usually occur 1-2 times a month, with more frequent check-ins if needed, to monitor symptoms and adjust prescriptions.
- Skills Training: You’ll learn practical coping strategies, communication skills, and life skills to manage symptoms, steer challenges, and build resilience in your daily life.
- Progress Monitoring: Your progress is continuously monitored and evaluated. We work with you to set measurable goals and adjust your treatment plan as needed, ensuring you’re always moving forward.
Sobriety and Family Involvement
For many, mental health and substance use are intertwined. IOPs often address both.
- Co-occurring Disorders: If you’re dealing with both a mental health condition and a substance use disorder (often called a dual diagnosis), our IOPs provide integrated treatment. We understand that these conditions often feed into each other, and addressing both simultaneously is crucial for lasting recovery. Learn more about Areas of Care: Virtual IOP/Dual Diagnosis.
- Maintaining Sobriety: For individuals with co-occurring substance use disorders, maintaining sobriety is a critical mental health intensive outpatient program requirement. This commitment ensures you can fully engage with the therapeutic process without the interference of active substance use.
- Family Therapy Sessions: Your support system plays a vital role in your recovery. We encourage family involvement through education and therapy sessions, helping your loved ones understand your journey and learn how to provide effective support. This can include Treatment Modalities: Virtual IOP/Family Therapy and Coaching Virtual IOP.
IOP vs. PHP: Is This the Right Level of Care for You?
Choosing the right level of care can feel like Goldilocks searching for the perfect bed: not too little, not too much, but just right. Intensive Outpatient Programs (IOPs) and Partial Hospitalization Programs (PHPs) are both crucial steps on the continuum of care, bridging the gap between traditional outpatient therapy and inpatient hospitalization. The key is understanding their differences to find your “just right.”
Both IOPs and PHPs offer intensive, structured treatment where you return home at the end of the day. The primary distinction lies in the intensity and time commitment. If you’re exploring PHP vs IOP, here’s a breakdown to help you find the right fit for your needs.
Key Differences: IOP vs. Partial Hospitalization (PHP)
| Feature | Intensive Outpatient Program (IOP) | Partial Hospitalization Program (PHP) |
|---|---|---|
| Time Commitment | 9-19 hours/week | 20+ hours/week |
| Schedule | Typically 3-5 days/week (often evenings) | Typically 5 days/week (daytime hours) |
| Focus | Integrating skills into daily life | Stabilization and intensive skill-building |
| Medical Support | Coordinated with outside providers | Often includes on-site medical/psychiatric staff |
| Best For | Step-down from PHP/inpatient or step-up from weekly therapy | Alternative to inpatient hospitalization or step-down from inpatient |
An IOP is often the choice for those who need more support than weekly therapy but can maintain some daily responsibilities. It’s also an excellent step-down option after a PHP or inpatient stay, allowing you to gradually reintegrate into your routine while still receiving significant therapeutic support.
A PHP, on the other hand, is a more intensive option. It’s ideal if you need a high level of care to stabilize acute symptoms but don’t require 24/7 inpatient supervision. PHPs are often considered an alternative to inpatient hospitalization or a direct step-down from inpatient care. The higher number of hours (20+ per week) and often on-site medical and psychiatric staff provide a more comprehensive and supervised environment for rapid stabilization and intensive skill-building.
Choosing between an IOP and a PHP depends entirely on your individual clinical needs, the severity of your symptoms, and your ability to function safely outside of program hours. Our clinical team at Thrive will conduct a thorough assessment to recommend the level of care that will best support your recovery journey.
Life After IOP: Your Next Steps to Lasting Wellness
Completing an IOP is a significant achievement, but it’s not the end of your journey—it’s a powerful new beginning. A crucial aspect of our programs at Thrive Mental Health is robust discharge planning, ensuring you have a clear path forward for lasting wellness.
We work with you from day one to develop a comprehensive aftercare plan. This plan is custom to your individual needs and focuses on relapse prevention, continuing care, and connecting you to ongoing resources. Your aftercare might involve transitioning to less intensive outpatient therapy, connecting with support groups, or continuing medication management with an outside psychiatrist. We want you to feel confident and supported as you apply the skills you’ve learned in your daily life. Reading My Experience with an Intensive Outpatient Program: A Personal Journey can offer personal insights into this transition.
Finding the right program is the first step, and knowing where to look is half the battle. Organizations like the National Alliance on Mental Illness (NAMI) are excellent resources for general information. At Thrive, we proudly offer both virtual and in-person IOPs across Florida, ensuring access to high-quality, evidence-based care.
Whether you’re looking for Virtual Intensive Outpatient Program Near Me (VIOP) or prefer an in-person setting, we have options in:
- Florida: Tampa Bay, St. Petersburg, Miami, Orlando, Boca Raton, West Palm Beach, Jacksonville, Fort Lauderdale, Naples, Sarasota.
Our expert-led virtual programs make treatment accessible anywhere, anytime, providing flexibility that fits modern life. We’re committed to measurable results, with 94% of our clients not requiring readmission to a higher level of care after completing our IOP. Your long-term well-being is our ultimate goal.
Frequently Asked Questions about IOP Requirements
How long does an IOP program typically last?
Most IOPs last between 8-12 weeks, but the exact duration depends on your individual progress and treatment plan. Some programs may be as short as 5 weeks or extend up to 12 weeks. The goal is to stabilize your symptoms and equip you with coping skills, not to keep you in treatment indefinitely. Your clinical team will continuously assess your progress to determine the most appropriate length of stay.
Can I work while attending an IOP?
Yes! Many IOPs, especially virtual programs like ours at Thrive Mental Health, offer evening or flexible schedules specifically designed to accommodate work, school, or family commitments. This flexibility is a key benefit of IOPs, allowing you to apply the skills you learn in therapy to your real-life situations immediately and maintain your daily responsibilities. Many individuals even take a temporary leave from work or school to fully immerse themselves in the recovery process, knowing they can return with renewed strength.
What if I have a substance use issue along with my mental health condition?
This is called a co-occurring disorder or dual diagnosis, and it’s very common. Most IOPs that treat co-occurring disorders will require a commitment to sobriety during the program. They will provide integrated treatment that addresses both the mental health symptoms and the substance use together, recognizing that treating one without the other often leads to challenges in long-term recovery.
What happens if I don’t meet the mental health intensive outpatient program requirements?
If an IOP isn’t the right fit after a comprehensive assessment, our clinical team will recommend a more appropriate level of care. This could mean a Partial Hospitalization Program (PHP) for more intensive support and structure if your symptoms are more severe, or traditional outpatient therapy if less structure is needed. The goal is always to guide you to the right place for your recovery journey, ensuring you receive the care that best suits your needs.
Your Path to Recovery Starts with the Right Support
Understanding the mental health intensive outpatient program requirements is the first step toward getting the structured support you need to heal. These programs bridge the gap between weekly therapy and inpatient care, offering an effective, flexible path to recovery. Thrive Mental Health provides expert-led virtual and in-person IOPs designed for real life across Florida. Our programs combine clinical expertise, flexible scheduling, and measurable results—designed for people who need more than once-a-week therapy but less than inpatient care.
Ready for support? Thrive offers virtual and hybrid IOP/PHP programs with evening options. Verify your insurance in 2 minutes (no obligation) → Start benefits check or call 561-203-6085. If you’re in crisis, call/text 988.