Mentalization Made Easy—The Art of Reading Minds

Why Understanding Minds Matters More Than You Think
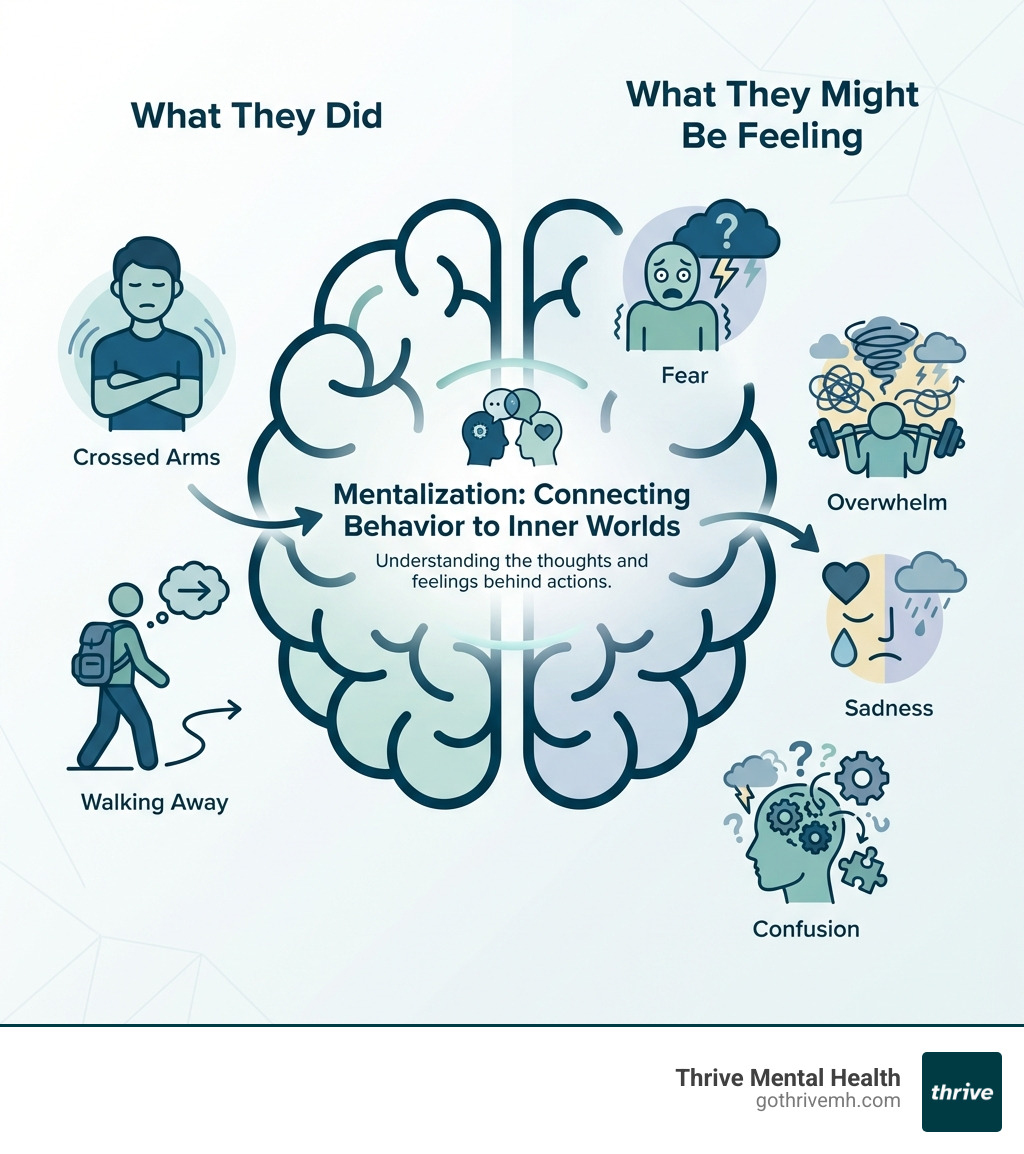
Mentalization definition: the ability to understand the mental states—thoughts, feelings, beliefs, and intentions—of yourself and others that underlie behavior.
In simple terms:
- What it is: Imagining what someone might be thinking or feeling, not just reacting to what they do
- Why it matters: It’s the foundation of healthy relationships, emotional control, and self-awareness
- Where it comes from: Developed in childhood through secure, responsive caregiving
- When it breaks down: Leads to misunderstandings, emotional chaos, and relationship conflict
Ever feel like you’re speaking a different language from the people you care about? Like you can see what someone did, but have no idea why they did it? That’s a breakdown in mentalization—the mental process that lets us “read minds” and decode the hidden reasons behind actions.
Mentalization isn’t magic. It’s a learnable skill that lets you step back from raw emotion and ask: What’s really going on in their head? What’s going on in mine? Without it, relationships feel like walking through a minefield. With it, you gain clarity, connection, and control over your reactions.
This matters because impaired mentalization is at the heart of many mental health struggles—especially borderline personality disorder (BPD), anxiety, and relationship trauma. When you can’t accurately read your own or others’ intentions, every interaction becomes a potential crisis. The good news? Mentalization can be rebuilt.
I’m Nate Raine, CEO of Thrive Mental Health, where we’ve spent years helping clients strengthen their mentalization and rebuild emotional stability through evidence-based programs like Mentalization-Based Treatment (MBT). Our virtual and in-person Intensive Outpatient (IOP) and Partial Hospitalization (PHP) programs in Florida are designed for people who need more than once-a-week therapy but less than inpatient care. This guide will show you exactly what mentalization is, why it breaks down, and how to repair it.
Mentalization definition vocab explained:
- mentalization-based therapy activities
- mentalization based family therapy
- mentalization based group therapy
What Is the Real Mentalization Definition? [Beyond the Textbook]

At its core, mentalization is the ability to see the mind behind the behavior. It’s how you interpret what people do based on what they might be thinking or feeling—their needs, desires, beliefs, and goals. When we mentalize, we’re not just reacting to actions; we’re inferring the minds that drive them.
Peter Fonagy, a key figure in the field, defines mentalization as the imaginative ability to understand the thoughts and feelings of others by imagining their inner experiences. It’s an “imaginative mental activity” because we can never truly know another’s mind, only make educated guesses. This same imaginative leap is needed to understand our own emotionally charged internal experiences. This capacity is often described as “thinking about thinking” or even “understanding misunderstanding.”
A common misconception is to equate mentalization with empathy, but they are distinct. Empathy is about feeling with someone—sharing their emotional state. Mentalization, however, is about understanding why they feel that way. It’s the cognitive process that often precedes and enables empathy. Without mentalization, empathy might be shallow or misplaced.
The concept of Theory of Mind (ToM) is closely related to mentalization and refers to the ability to attribute mental states to oneself and others. Crucial elements of a “full Theory of Mind,” such as understanding other people’s true beliefs and false beliefs, are typically developed by about the fourth year of life. For instance, early research empirically tested this by observing when children could understand that someone might hold a false belief about the world, such as thinking a toy is in one box when they saw it moved to another. This developmental milestone is critical for social interaction. You can explore more about this foundational research on false-belief understanding in children.
The 4 Dimensions of Mentalizing
Mentalization isn’t a single, monolithic skill; it operates along four interconnected dimensions, as outlined in the American Psychiatric Association’s Handbook of Mentalizing in Mental Health Practice. A healthy ability to mentalize involves navigating and balancing these dimensions.
-
Automatic vs. Controlled: This dimension describes the speed and effort involved.
- Automatic mentalization is our quick, intuitive read of social cues—a gut instinct about someone’s mood. It’s fast and efficient, like instinctively knowing someone is upset by their tone of voice.
- Controlled mentalization is a more deliberate, conscious process. It involves stepping back, reflecting, and actively analyzing a situation to understand complex motivations, especially when emotions are high or initial interpretations are unclear. For example, pausing to consider why your partner snapped, rather than just reacting to the snap.
- Real-world example: When a friend suddenly goes quiet, an automatic mentalizer might immediately assume they’re angry. A controlled mentalizer would consciously consider if they might be tired, preoccupied, or sad.
-
Self vs. Other: This dimension highlights whether we are reflecting on our own mental states or those of others.
- Self-mentalization involves understanding our own feelings, thoughts, and intentions. It’s about introspection and self-awareness.
- Other-mentalization involves understanding the internal world of another person. It’s crucial for effective communication and relationships.
- Real-world example: After an argument, reflecting on “Why did I get so angry?” (self) versus “What was my boss trying to achieve when she said that?” (other).
-
Inner vs. Outer: This dimension refers to the focus of our attention.
- Inner-mentalization focuses on internal experiences—emotions, sensations, subjective thoughts.
- Outer-mentalization focuses on observable behavior and external cues, interpreting them in terms of underlying mental states.
- Real-world example: Noticing a knot in your stomach and realizing it’s anxiety (inner) versus seeing a colleague fidgeting and concluding they’re nervous (outer).
-
Cognitive vs. Affective: This dimension distinguishes between the “thinking” and “feeling” aspects of mental states.
- Cognitive mentalization involves understanding beliefs, intentions, and logical reasoning. It’s about “what they think.”
- Affective mentalization involves understanding emotions and feelings. It’s about “what they feel.”
- Real-world example: Understanding that a friend declined an invitation because they had a prior commitment (cognitive) versus understanding that they felt disappointed about missing out (affective).
When these dimensions are unbalanced, it can lead to difficulties. For instance, being stuck in automatic mentalization can lead to simplistic, rigid views, while being overly in controlled mentalization can lead to rumination and overthinking. Similarly, an imbalance between cognitive and affective mentalization can make us either too analytical or too overwhelmed by emotions.
How Your Past Shapes Your Ability to Mentalize

Our capacity for mentalization isn’t something we’re born with fully formed. It’s deeply rooted in our earliest experiences, particularly the quality of our attachment relationships. Attachment theory, pioneered by John Bowlby, posits that the bond we form with our primary caregivers profoundly shapes our ability to regulate emotions and understand ourselves and others.
-
Secure Attachment: When caregivers are consistently responsive, sensitive, and accurately interpret a child’s needs and emotional states, they foster secure attachment. This consistent “mind-mindedness”—the parent’s capacity to mentalize their child—provides a safe base for the child to develop their own mentalizing abilities. Securely attached individuals often have had primary caregivers with more complex and sophisticated mentalizing abilities themselves. This early exposure to genuine parental mentalization can protect individuals from psychosocial adversity and foster the development of mentalizing capabilities in the child. Research on parental reflective functioning highlights this crucial link.
-
Insecure Attachment: Conversely, inconsistent, unresponsive, or frightening caregiving can lead to insecure attachment styles. Children in these environments may struggle to develop robust mentalizing capacities, leading to what is often called “reflective functioning (RF) deficits.” Insecure attachment is related to RF deficits, which together increase the risk for developing various psychopathological conditions, including anxiety and depressive disorders.
The parental capacity to mentalize their child is a strong predictor of the child’s own ability to mentalize. When parents reflect and name a child’s emotional states—”You seem angry because your toy broke,” or “You’re sad that mommy is leaving”—they provide a “social biofeedback” mechanism. This helps the child differentiate and understand their own internal experiences, laying the groundwork for emotional self-regulation and a coherent sense of self. Without this, a child might struggle to recognize their own feelings as distinct mental states, impacting their personality development and future relationships.
If gaps in this early foundation are still affecting you as an adult, structured support like Intensive Outpatient Programs (IOP) or Partial Hospitalization Programs (PHP) can help you relearn and strengthen mentalization skills in a safe, guided setting.
When Mentalizing Fails: The Link to BPD and Emotional Chaos
Crisis Disclaimer Callout Box
If you or a loved one are in crisis or considering self-harm, please call or text 988 immediately. Help is available 24/7, and you are not alone.
When mentalization breaks down, it can feel like the world loses its meaning, and relationships become a source of intense pain and confusion. We see this acutely in conditions like Borderline Personality Disorder (BPD), where a temporary or chronic loss of mentalizing is a core feature. Individuals with BPD often struggle to differentiate between their own emotional state and that of others, and they may have difficulty understanding how mental states influence behavior. This impaired mentalization can lead to:
- Misreading intentions: Interpreting neutral cues as hostile or benign cues as threatening.
- Black-and-white thinking: An inability to see shades of gray in situations or people, leading to rapid shifts between idealization and devaluation.
- Emotional storms: Intense, overwhelming feelings that are difficult to regulate, often triggered by interpersonal events.
- Unstable relationships: A cycle of intense closeness followed by dramatic ruptures, driven by misunderstandings and emotional dysregulation.
Before a full capacity for mentalization develops, children might operate in what are called “pre-mentalistic modes” of thought. These modes, while normal in early development, can persist or re-emerge under stress when mentalizing fails, especially in individuals with BPD:
- Psychic Equivalence Mode: In this mode, the internal world is equated with external reality. If I feel it, it must be true and real for everyone. For example, if I feel abandoned, then I am being abandoned, regardless of the objective situation. My thoughts are facts.
- Pretend Mode: Here, mental states are acknowledged but are seen as having no connection to reality. Thoughts and feelings are like a game, separate from real-world consequences. This can manifest as superficial conversations about feelings without genuine emotional engagement, or fantasizing that bears no relation to reality.
- Teleological Mode: In this mode, only concrete actions and physical outcomes matter. Intentions and feelings are disregarded; behavior is interpreted solely by its observable effects. “If you loved me, you would do X.” If X isn’t done, then love is absent, regardless of the other person’s internal experience.
When mentalizing fails and these pre-mentalistic modes dominate, the consequences for individuals can be severe: intense emotional dysregulation, a fragmented sense of identity, and chaotic interpersonal patterns. This is particularly challenging for those with BPD, where the inability to mentalize during moments of high emotional arousal can lead to impulsive actions, self-harm, and profound relationship difficulties.
At Thrive Mental Health, we understand these challenges. Our Intensive Outpatient (IOP) and Partial Hospitalization (PHP) programs in Florida are designed to help individuals regain their mentalizing capacity. We offer structured, supportive environments that provide more than once-a-week therapy, focusing on evidence-based treatments like MBT and DBT-informed care to help you steer these emotional storms. Many clients use insurance plans such as Cigna, Optum, Florida Blue, and other major carriers to access care. Learn more about our IOP programs for BPD or explore our virtual IOP options if you need flexible support from home.
How Mentalization-Based Treatment (MBT) Rebuilds Your Inner World
Mentalization-Based Treatment (MBT) is a specialized, psychodynamically-oriented psychotherapy specifically developed to address these mentalization deficits, particularly in patients with Borderline Personality Disorder (BPD). It’s built on the understanding that many psychological difficulties stem from an impaired ability to mentalize—to understand one’s own and others’ mental states. MBT aims to restore and stabilize this crucial capacity.
The primary goal of MBT is to help clients improve their ability to mentalize, especially during moments of intense emotional arousal when this capacity is most likely to break down. By strengthening mentalization, clients can better regulate their emotions, develop a more stable sense of self, and steer interpersonal relationships with greater clarity and resilience. As research published in World Psychiatry indicates, MBT is an effective treatment for BPD, helping to reduce symptoms like impulsivity, self-harm, and relational conflicts. The therapy also helps foster a more secure sense of self and improves overall psychological well-being.
A core tenet of MBT is the therapist’s “not-knowing” stance. Instead of positioning themselves as an expert who has all the answers, the therapist approaches the client’s experience with genuine curiosity and humility. They don’t claim to know what the client is thinking or feeling, but rather encourage the client to explore their own mind and consider alternative perspectives. This fosters a safe environment for exploration and helps the client learn to become curious about their own and others’ internal worlds.
Thrive Mental Health integrates MBT principles into our IOP and PHP programs, both in-person across Florida and through virtual IOP options, so you can access this approach even if you are in a busy season of life or live far from a treatment center.
Core Techniques and the Mentalization Definition in Practice
MBT uses a variety of techniques that bring the mentalization definition to life within the therapy session:
- Stop and Rewind: When a client describes a difficult interaction, the therapist might ask them to “stop and rewind” to a specific moment. The goal isn’t to rehash the event, but to deconstruct it by exploring the mental states involved: “What were you thinking right before that happened? What do you imagine the other person might have been feeling or intending?” This helps clients slow down and consider multiple perspectives.
- Exploring the Affective Moment: Emotions are powerful, and in MBT, they’re not avoided but explored as they happen in the therapy session. If a client expresses anger or sadness, the therapist might gently inquire, “What’s happening in your mind right now as you feel that anger? What thoughts are going along with it?” This helps clients connect their emotions to underlying mental states.
- Challenging Non-Mentalizing: Therapists gently challenge instances where clients fall into pre-mentalistic modes of thinking (psychic equivalence, pretend, teleological). For example, if a client says, “She hates me because she didn’t text back immediately,” the therapist might respond, “It sounds like you’re certain of her feelings. Could there be another reason she hasn’t texted yet?” This encourages flexibility in thinking.
- The Therapist’s Role: Crucially, the therapist actively models mentalization. They consistently demonstrate curiosity about the client’s internal world, reflect on their own understanding (and potential misunderstandings), and show a genuine interest in the client’s unique subjective experience. This provides a live example of healthy mentalizing, which the client can internalize and learn from. The therapist essentially holds the client’s mind in mind, creating a secure base within the therapeutic relationship.
MBT vs. DBT: What’s the Difference?
Both Mentalization-Based Treatment (MBT) and Dialectical Behavior Therapy (DBT) are highly effective, evidence-based therapies for BPD, but they approach the disorder from different theoretical angles.
| Feature | Mentalization-Based Treatment (MBT) | Dialectical Behavior Therapy (DBT) |
|---|---|---|
| Primary Focus | Enhancing the capacity to mentalize (understanding self and others’ mental states). | Teaching skills to manage intense emotions, improve relationships, and tolerate distress. |
| Core Approach | Exploratory, psychodynamic, relational. Focuses on the “why” behind feelings and behaviors, fostering curiosity about internal states. | Skills-based, cognitive-behavioral. Focuses on “how” to change problematic behaviors and emotional responses. |
| Theoretical Roots | Attachment theory, psychoanalysis, developmental psychopathology, cognitive neuroscience. | Behaviorism, mindfulness, dialectics. |
| Therapist Role | Collaborative, curious, “not-knowing” stance, models mentalization, helps client explore mental states. | Coaching, directive, teaches specific skills, balances acceptance and change. |
| Key Techniques | Stop and Rewind, Exploring Affective Moment, Challenging Non-Mentalizing, mentalizing the transference. | Mindfulness, Distress Tolerance, Emotion Regulation, Interpersonal Effectiveness skills. |
| Application | Addresses underlying deficits in understanding self and others, leading to more stable sense of self and relationships. | Directly targets behavioral dysregulation (self-harm, suicidality, impulsivity) and emotional instability through skill acquisition. |
While DBT focuses on skill acquisition to manage symptoms, MBT digs deeper into the fundamental processes of understanding minds, aiming for a more profound and stable change in how individuals relate to themselves and the world. Both are valuable, and the choice often depends on individual needs and clinical presentation. Many individuals benefit from elements of both or from therapies that integrate these insights.
At Thrive Mental Health, we offer comprehensive virtual and in-person programs across Florida, from Miami and Orlando to Jacksonville and Tampa Bay. Our virtual therapy options can incorporate elements of both MBT and DBT, custom to your specific needs. To see how your insurance benefits (including Cigna, Optum, Florida Blue, and others) may help cover care, you can start a quick insurance verification online.
Frequently Asked Questions about Mentalization
What is an example of mentalization?
Imagine a friend cancels plans last minute. Instead of immediately concluding they’re angry with you (a non-mentalizing thought), you pause. You consider other possibilities: maybe they’re stressed from work, feeling unwell, or have a family emergency. This act of generating multiple explanations for their internal state, rather than jumping to one conclusion, is an example of mentalization.
Can you improve your ability to mentalize?
Absolutely. Mentalizing is a skill, not a fixed trait. It can be strengthened at any age through self-reflection, practicing curiosity about others, and engaging in targeted therapies like MBT. Structured support such as IOP or PHP can accelerate this growth by giving you daily practice in a safe setting.
What is the opposite of mentalization?
The opposite of mentalization is often referred to as non-mentalizing or “pre-mentalistic thinking.” This occurs when we lose the ability to see the mind behind the behavior, especially under stress or intense emotion. It leads to misunderstandings, rigid interpretations, and often, intense emotional reactions because we react to behavior as if it is the mental state, rather than a representation of it.
Is mentalization the same as empathy?
No. Empathy is feeling with someone—sharing their emotional state. Mentalization is understanding why they feel or act a certain way by considering their beliefs, history, and context. In treatment, both matter: MBT strengthens mentalization so empathy becomes more accurate and less overwhelming.
How does mentalization-based treatment fit into IOP or PHP?
In programs like Thrive’s Intensive Outpatient Program and PHP, MBT principles are woven into individual therapy, groups, and skills work. You repeatedly practice slowing down, checking assumptions, and exploring your own and others’ minds, which helps stabilize emotions and relationships between sessions.
For a deeper dive on using MBT skills day-to-day, you can also read our related guide on mentalization-based therapy activities.
Take the Next Step: From Understanding to Healing
Mentalization—the ability to understand the minds behind behavior—is a fundamental human capacity crucial for healthy relationships and emotional stability. This guide has explored the mentalization definition in depth, showing that while this ability can be disrupted by trauma, BPD, or attachment difficulties, it is not a life sentence; it can be improved with the right support.
Thrive Mental Health’s Intensive Outpatient (IOP) and Partial Hospitalization (PHP) programs, available in-person across Florida or virtually nationwide, are designed to help clients rebuild mentalization, regulate emotions, and stabilize relationships. Many clients use major insurance plans like Cigna, Optum, Florida Blue, and others to reduce out-of-pocket costs, making expert care more accessible.
Whether you are in Miami, Orlando, Jacksonville, Tampa, or anywhere else in Florida, our virtual IOP and hybrid programs bring evidence-based treatment to you with flexible scheduling, including evening options.
Ready for support? Thrive offers virtual and hybrid IOP/PHP programs with evening options. Verify your insurance in 2 minutes (no obligation) → Start benefits check or call 561-203-6085. If you’re in crisis, call/text 988.