From Hurt to Healing – Overcoming Childhood Trauma

How to Heal from Childhood Trauma [6 Steps That Actually Work]
Learning how to heal from childhood trauma starts with this truth: you are not broken, and you are not too far gone. The ways you learned to survive chaos, abuse, or neglect were intelligent adaptations. But if those same survival skills are now wrecking your relationships, health, or career, it’s time to upgrade them.
Left untreated, childhood trauma silently drains you for decades: chronic anxiety, burnout, failed relationships, health issues, and a constant sense that you’re “not enough.” With the right support, you can lower your daily stress, stabilize your mood, and feel safe in your own body again—often in months, not years.
Below is a clear, no-fluff roadmap to healing, plus how structured programs like IOP and PHP (including virtual options) can speed up recovery compared to once-a-week therapy.
The 6 Core Steps to Heal from Childhood Trauma
-
Acknowledge Your Experience (Stop Minimizing It)
If you grew up hearing “it wasn’t that bad” or “other people had it worse,” you probably gaslight yourself. Healing starts when you name what really happened: abuse, neglect, addiction in the home, mental illness, violence, or constant chaos.
Acknowledgment doesn’t trap you in the past—it gives you an accurate starting point so you can finally change the future. -
Get Trauma-Informed Treatment (Not Generic Talk Therapy)
Trauma isn’t a DIY project or something you “just get over.” You need treatment that targets how trauma lives in your brain and body. Look for:- CBT (Cognitive Behavioral Therapy) – challenges the beliefs trauma wired into you (“I’m unsafe,” “I’m unlovable”).
- EMDR – helps your brain reprocess traumatic memories so they stop hijacking you.
- Somatic therapies – help your body release the tension and threat response it’s been holding for years.
Weekly therapy can help, but it’s often too slow when symptoms are intense. That’s why a lot of adults with complex or developmental trauma do better in Intensive Outpatient Programs (IOP) or Partial Hospitalization Programs (PHP) that offer multiple sessions per week, structured groups, and coordinated care.
→ Learn how Thrive’s IOP and PHP programs support trauma recovery: https://gothrivemh.com
-
Process Emotions Safely (Without Getting Flooded)
Unprocessed trauma keeps you stuck in loops: shutdown, rage, panic, or numbness. In trauma-informed care, you don’t just “tell your story and cry it out.” You:- Learn grounding skills first.
- Slowly approach painful memories in small, tolerable pieces.
- Build the ability to feel big emotions without collapsing or exploding.
Done right, this reduces flashbacks, emotional outbursts, and shutdowns instead of re-traumatizing you.
-
Build a Support System That Actually Feels Safe
Trauma often teaches you that people are dangerous or unreliable. You may isolate or choose unsafe partners and friends because that’s what’s familiar. Healing requires new kinds of connection:- One or two safe people who listen instead of fixing or judging.
- Peer or therapy groups where others get complex trauma.
- Boundaries with people who minimize or dismiss your past.
In our trauma-focused IOP/PHP and virtual therapy options, adults build these skills in real time—with coaching, feedback, and support.
-
Regulate Your Nervous System (So You’re Not on Edge All Day)
Childhood trauma keeps your body in survival mode. You might:- Snap at small things.
- Feel constantly exhausted but unable to relax.
- Struggle with sleep, digestion, or chronic pain.
Simple daily practices help teach your body that it’s safe now:
- Slow, deep breathing (longer exhale than inhale).
- Grounding (notice 5 things you can see, 4 you can feel, 3 you can hear, etc.).
- Rhythmic movement (walking, light exercise, dancing).
In structured programs, we pair these tools with therapy so your brain and body learn new patterns faster.
-
Practice Relentless Self-Compassion (Not Self-Improvement Hype)
Healing from childhood trauma is not linear. You will have days where symptoms spike. That doesn’t mean you’re failing; it means your nervous system is learning something new.Replace “What’s wrong with me?” with:
- “What happened to me?”
- “What do I need right now to feel 5% safer?”
Over time, this shift reduces shame, which is one of the biggest blocks to progress.
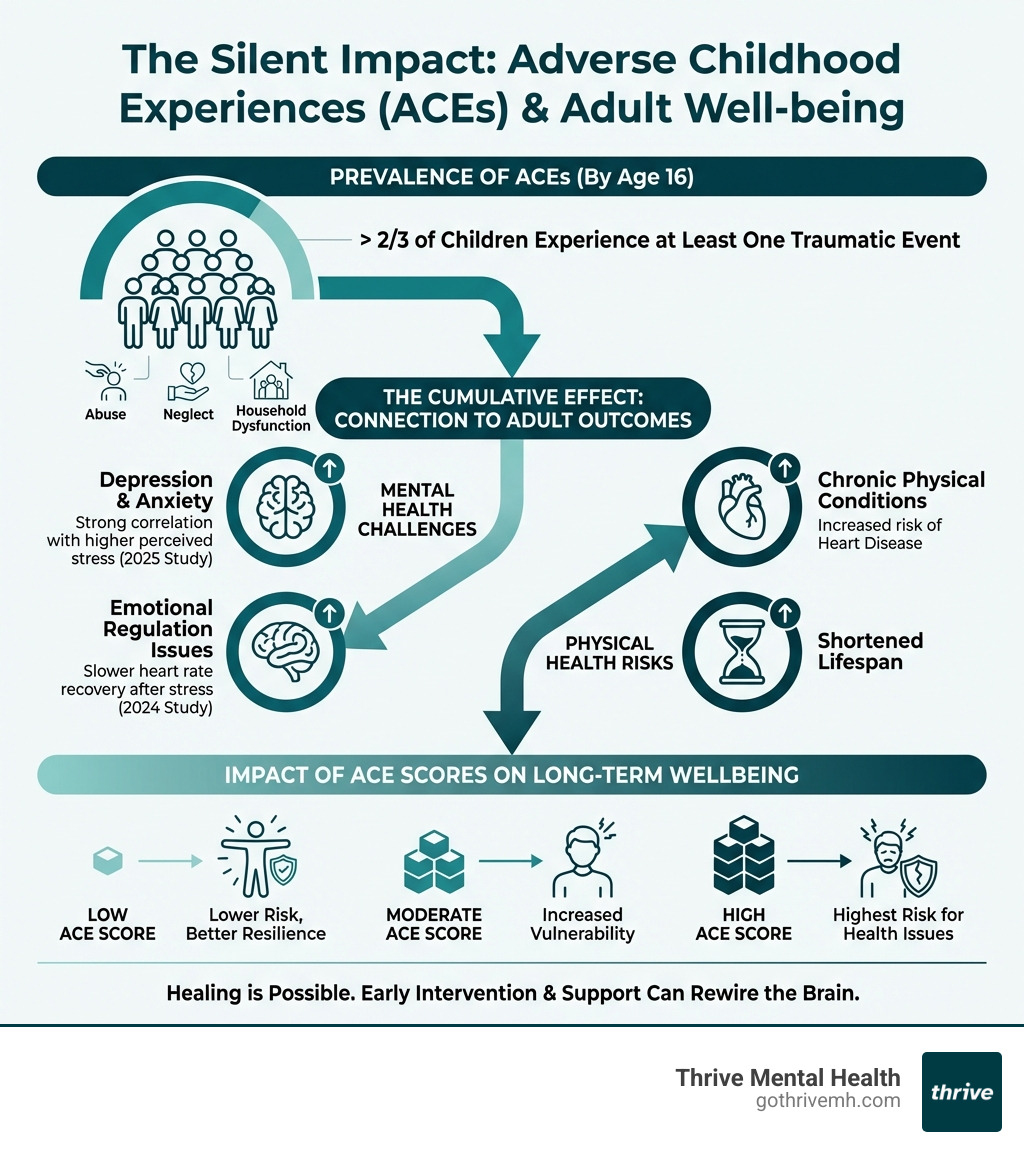
The numbers are clear: over two-thirds of children experience at least one traumatic event by age 16. High Adverse Childhood Experiences (ACE) scores are linked to higher rates of depression, anxiety, chronic illness, and even a shorter lifespan.
The hopeful part: your brain can rewire. Neuroplasticity means the pathways built under trauma aren’t permanent. With consistent, evidence-based treatment—especially in focused settings like IOP/PHP—you can:
- Lower your daily stress level.
- Improve sleep and emotional control.
- Build healthier, more secure relationships.
As Nate Raine, CEO of Thrive Mental Health, I’ve seen adults who felt “broken beyond repair” reclaim their lives in a matter of months once they stepped into the right level of care. Our virtual and hybrid trauma-focused programs are built for busy adults in Florida who need more than weekly therapy but can’t disappear from work or family.
We’re in-network with many major plans—including Cigna, Optum/UnitedHealthcare, Florida Blue, Aetna, and others—so you can actually use the benefits you’re paying for.
How to heal from childhood trauma vocab explained:
FAQs: How to Heal from Childhood Trauma
1. Can you really heal from childhood trauma, or do you just learn to cope?
You can do more than cope. With the right treatment (often IOP/PHP plus ongoing therapy), your symptoms can drop significantly: fewer flashbacks, less anxiety, better sleep, and healthier relationships. You may always remember what happened, but it no longer has to run your life.
2. How long does it take to heal from childhood trauma?
It varies, but many adults notice meaningful changes within 8-12 weeks of consistent, intensive treatment (like IOP), especially when combined with medication management and aftercare. Deep healing is ongoing, but you don’t have to wait years to feel relief.
3. Is once-a-week therapy enough for complex childhood trauma?
For some people, yes. But if you’re dealing with constant crises, intense emotions, or unsafe coping (self-harm, substance use), weekly therapy is usually too little. That’s when IOP or PHP is more effective because you’re getting several hours of focused help each week.
4. Does insurance cover trauma treatment like IOP or PHP?
Often, yes. At Thrive, we work with major insurers such as Cigna, Optum, UnitedHealthcare, Florida Blue, and others. Coverage depends on your plan and medical necessity, which we help you verify in a few minutes.
5. Is virtual trauma treatment as effective as in-person?
For many adults, virtual IOP and therapy are just as effective—and easier to stick with. You can join from home in Florida, avoiding commute time and keeping your routine more stable.
Summary: How to Heal from Childhood Trauma and What to Do Next
If you grew up in chaos, abuse, or neglect, struggling as an adult is not a personal failure—it’s a predictable outcome of what your brain and body went through. The good news: with trauma-informed care, structured support (often IOP/PHP), and consistent nervous system regulation, you can break old patterns, feel safer in your skin, and build a life that isn’t controlled by your past.
If you want a deeper dive into how trauma rewires your brain, read this related guide: Trauma and Your Brain: Understanding the Neurological Impact.
Ready for support? Thrive offers virtual and hybrid IOP/PHP programs with evening options. Verify your insurance in 2 minutes (no obligation) → https://gothrivemh.com/verify-insurance/ or call 561-203-6085. If you’re in crisis, call/text 988.
The Hidden Wounds: How Childhood Trauma Rewires Your Brain and Body
Childhood trauma isn’t “just bad memories.” It can be chronic stress, constant fear, emotional neglect, or outright abuse that changes how your brain and body work. If you’re wondering why you’re always on edge, exhausted, or sabotaging relationships, this is likely why.

Trauma doesn’t just live in your thoughts—it embeds in your nervous system. It disrupts the brain’s stress response (fight–flight–freeze), often leading to:
- An overactive amygdala (your internal alarm system).
- An underactive prefrontal cortex (the part that helps you think clearly, plan, and regulate emotions).
This is why you might:
- React to small triggers.
- Shut down or go numb in conflict.
- Feel like your body is stuck in high alert—even when you “know” you’re safe.
A 2024 neuroimaging study on trauma’s brain impact by Hendrikse et al. showed visible microstructural changes in white matter tracts in people who experienced childhood trauma. These “neural highways” connect brain areas responsible for emotion, memory, and stress regulation. When they’re disrupted, it explains why survivors often feel:
- Perpetually anxious or on guard.
- Emotionally unstable or reactive.
- Disconnected from their bodies or feelings.
“The body keeps the score” is not just a phrase—it’s a medical reality. Even when you don’t consciously remember everything, your nervous system remembers. That’s why effective trauma treatment must involve both brain and body, not just talking about what happened.
The hopeful news: your brain is plastic. With targeted, evidence-based care—including CBT, EMDR, somatic work, and structured programs like IOP or PHP—you can build new neural pathways that:
- Calm your baseline anxiety.
- Improve emotional control.
- Help you feel more present and grounded.
What Are the Different Forms of Trauma?
Naming what you went through helps you find the right kind of treatment. Here are the main types:
- Acute Trauma: A single overwhelming event (serious accident, assault, natural disaster).
- Chronic Trauma: Repeated stress or harm over time (domestic violence, long-term bullying, community violence).
- Complex Trauma (C-PTSD): Ongoing trauma in relationships—usually in childhood—such as abuse, neglect, or living with caregivers who are unpredictable, addicted, or violent.
- Developmental Trauma: Trauma during the earliest years of life that disrupts attachment, emotional regulation, and sense of self.
- Secondary or Vicarious Trauma: The impact of being repeatedly exposed to other people’s trauma (common in therapists, first responders, medical staff, and family members of survivors).
It’s important to distinguish trauma from PTSD:
| Feature | Trauma | Post-Traumatic Stress Disorder (PTSD) |
|---|---|---|
| Definition | The emotional and physical response to a deeply distressing event or series of events. | A specific mental health diagnosis that can follow trauma. |
| Duration | Symptoms often ease in days or weeks. | Symptoms last more than one month and cause major problems at work, home, or in relationships. |
| Core Symptoms | Shock, fear, anger, guilt, numbness, physical tension, sleep problems. | Re-experiencing (flashbacks, nightmares), avoidance, negative beliefs/mood, and hyperarousal (jumpy, irritable, on guard). |
| Universality | Most people will experience trauma. | Only a portion of trauma survivors develop PTSD or C-PTSD. |
If symptoms are intense or long-lasting, weekly therapy alone may not be enough. Many adults benefit from trauma-focused IOP or PHP, which offer multiple therapy hours per week, skills groups, and medication support. Thrive offers virtual and hybrid options in Florida, so you can access higher-level care without relocating.
How Do Adverse Childhood Experiences (ACEs) Fuel Long-Term Health Crises?
The Adverse Childhood Experiences (ACE) Study by the CDC and Kaiser Permanente showed just how costly untreated childhood trauma can be.
What are ACEs? (CDC) ACEs include 10 categories of adversity before age 18:
- Physical, emotional, or sexual abuse.
- Physical or emotional neglect.
- Household substance use, mental illness, domestic violence, parental separation/divorce, or incarceration.
Your ACE score is simply how many of these you experienced. The higher the score, the greater your risk for serious problems later in life.
- Mental Health: With an ACE score of 4+, your risk of depression is about 4.6x higher, and your risk of suicide attempts can be 10-12x higher.
- Chronic Disease: High ACEs are linked with increased risk of heart disease, cancer, COPD, liver disease, and autoimmune conditions.
- Behavioral Issues: ACEs raise the chances of smoking, heavy drinking, and drug use—often as attempts to self-medicate.
- Lifespan: Severe, unaddressed ACEs can shorten life expectancy by up to 20 years.
This isn’t about blaming your childhood. It’s about understanding the biology you’re working with so you can get the right level of care now. Trauma-informed treatment—especially structured, intensive options like IOP and PHP—is not a luxury. It’s preventive healthcare that can:
- Reduce ER visits and hospitalizations.
- Lower reliance on substances to cope.
- Help stabilize mood and functioning so you can actually use your potential.
If you want to explore evidence-based options, see: Evidence-Based Trauma Treatment.
Ready for support? Thrive offers virtual and hybrid IOP/PHP programs with evening options. Verify your insurance in 2 minutes (no obligation) → https://gothrivemh.com/verify-insurance/ or call 561-203-6085. If you’re in crisis, call/text 988.