Hyperarousal Explained: Why Your Fight-or-Flight Won’t Quit

Introduction: Why You’re Always On Edge—and How to Break Free
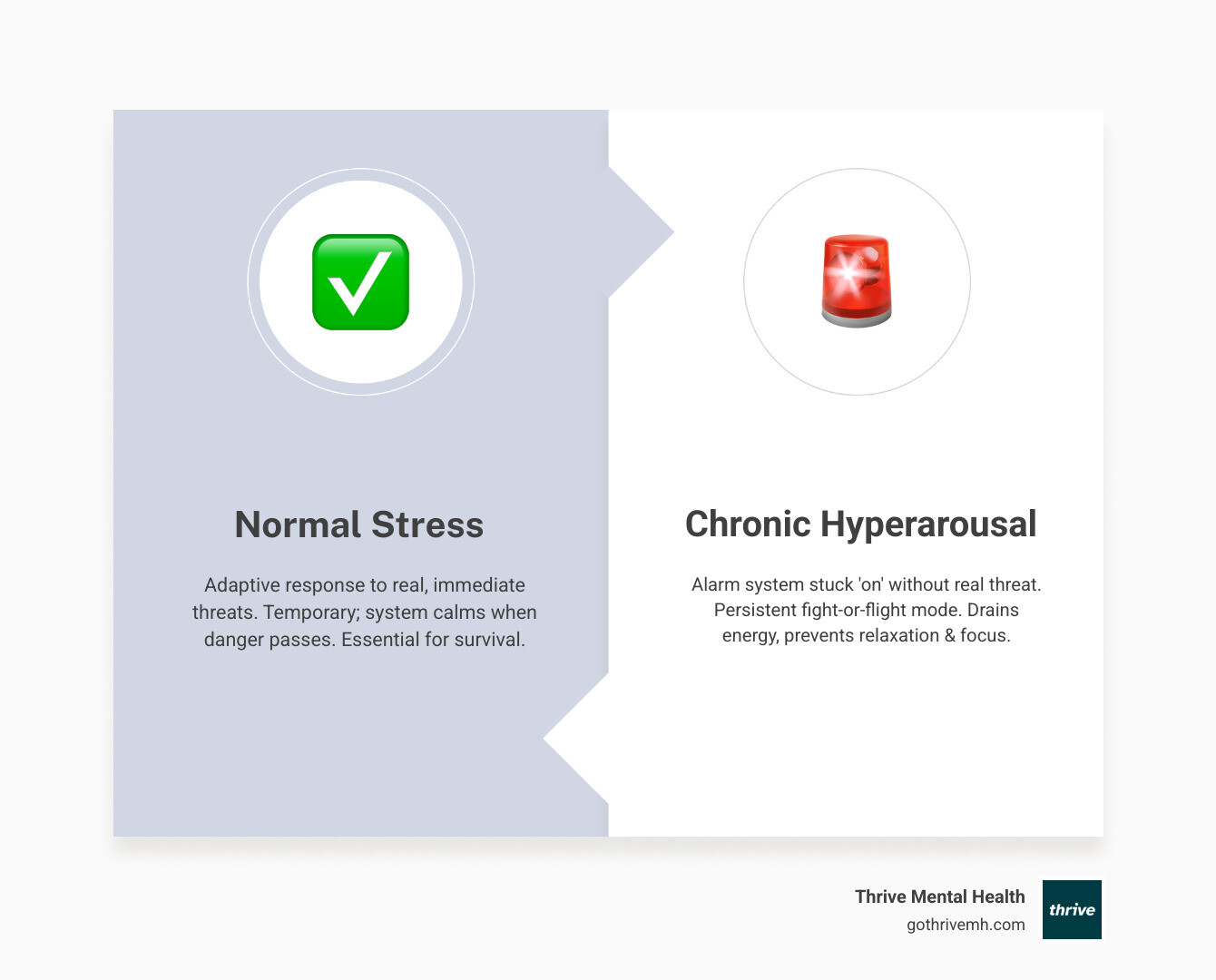
Ever feel like your body is always on high alert? Hyperarousal is when your internal alarm system gets stuck in “on” mode. It’s your body’s fight-or-flight response constantly active, even when there’s no real danger. This state leaves you feeling jumpy, irritable, and unable to relax.
Here’s what hyperarousal means:
- Your body’s “fight-or-flight” response is always on.
- You feel constantly on high alert, even when safe.
- It’s a core symptom of trauma, anxiety, and insomnia.
- It can show up as irritability, sleep problems, and trouble focusing.
This constant state of readiness drains your energy, makes sleep nearly impossible, and sabotages your focus. It’s exhausting, but you can learn to calm your nervous system and regain control. This guide will show you how.
I’m Nate Raine, CEO of Thrive Mental Health. With a decade of leadership in mental health and digital change, I’ve seen how crucial it is to understand and effectively manage conditions like hyperarousal for true wellness. I’m here to help you steer this challenging experience with clarity and practical steps.
If you live in Florida, you can access Thrive’s expert-led IOP (Intensive Outpatient) and PHP (Partial Hospitalization) programs virtually or at our trusted local centers.
What is Hyperarousal? (And Why Won’t It Stop?)
Imagine your body’s natural alarm system, designed to protect you from immediate danger, suddenly getting stuck in the “on” position. That’s hyperarousal in a nutshell. It’s a physiological and psychological state where your nervous system is perpetually activated, priming you for a threat that isn’t actually there. This can leave you feeling jumpy, tense, and unable to truly relax, no matter how hard you try. It’s more than just feeling stressed; it’s a persistent, pervasive state of liftd alertness that can impact every aspect of your life.
Hyperarousal is a key symptom of anxiety, stress-related disorders, and insomnia. While it has been conceptualized in many ways—from physiological markers like cortisol levels to subjective feelings of tension—the core idea remains the same: your system is overstimulated. This constant state of readiness consumes immense energy, preventing your body and mind from returning to a calm, balanced state.
The Symptoms You Can’t Ignore
The signs of hyperarousal can be both physical and emotional, often making daily life a constant battle.
Physical Symptoms:
- Pounding heart and rapid breathing: Your cardiovascular system is working overtime, preparing for action.
- Sweating: A common stress response, even without physical exertion.
- Muscle tension: Muscles are perpetually braced, leading to chronic aches and pains.
- Fatigue: Despite being on high alert, the constant energy drain leads to exhaustion.
- Insomnia and other sleep problems: Difficulty falling asleep, staying asleep, or experiencing restless, unrefreshing sleep. Your mind might race at 2 a.m., making sleep feel impossible.
- Exaggerated startle response: You might jump at unexpected noises or movements.
- Jittery feelings: A pervasive sense of restlessness or unease.
Emotional & Cognitive Symptoms:
- Irritability and angry outbursts: Small annoyances can trigger disproportionate reactions. Hyperarousal may lead to outbursts or behaviors you later regret or feel ashamed of.
- Anxiety and panic attacks: Constant worry or sudden, intense episodes of fear.
- Racing thoughts: Your mind struggles to quiet down, often cycling through worries or past events.
- Trouble focusing and concentrating: Sustaining attention becomes difficult, affecting work and daily tasks.
- Paranoia: A persistent feeling that something bad is about to happen, or that others are a threat.
- Feeling on edge: A general sense of unease and hyper-vigilance.
How is Hyperarousal Diagnosed?
Hyperarousal is not a symptom that can be self-diagnosed or self-treated. If you suspect you are experiencing it, especially if it’s persistent and affecting your quality of life, consulting a healthcare provider is crucial. A thorough diagnosis typically involves:
- Clinical assessment by a mental health professional: This includes a detailed interview about your symptoms, medical history, and life experiences. Professionals like psychiatrists and psychologists are trained to identify patterns consistent with hyperarousal and related conditions.
- Often part of PTSD or anxiety diagnosis: Hyperarousal is a core component of Post-Traumatic Stress Disorder (PTSD) and is frequently seen in various anxiety disorders. For instance, it is one of the key symptoms doctors look for when diagnosing PTSD. To be diagnosed with PTSD, you will typically have to experience two hyperarousal symptoms over a one-month period, alongside other criteria.
- Ruling out medical causes: Before a mental health diagnosis is made, your doctor may perform tests to rule out any underlying physical conditions that could be causing similar symptoms.
- Insurance coverage available: We understand that seeking help can feel daunting, especially when considering costs. The good news is that most insurance plans, including Cigna, Optum, Florida Blue, and many others, offer coverage for mental health treatment, including therapy and intensive outpatient (IOP) or partial hospitalization (PHP) programs. Thrive Mental Health proudly serves communities across Florida, working with a wide range of providers to make care accessible.
If you are ready to explore treatment options or confirm your benefits, you can verify your insurance with Thrive in just a couple of minutes, with no obligation.
What Triggers Hyperarousal? (And How Does It Start?)
Hyperarousal often stems from situations that overwhelm our natural coping mechanisms, flipping our stress switch and keeping it stuck. The primary triggers usually involve:
- Trauma: Experiencing or witnessing traumatic events, such as accidents, abuse, combat, or natural disasters, is a major cause. The body’s response to these events can become dysregulated. Approximately 70% of people will experience a traumatic event in their lifetime, but only a smaller percentage will develop PTSD, suggesting a complex interplay of factors.
- Chronic stress: Prolonged periods of high stress, even without a single traumatic event, can wear down the nervous system, leading to a constant state of alert.
- Anxiety disorders: Conditions like generalized anxiety disorder, panic disorder, and social anxiety disorder often involve heightened physiological arousal.
- Insomnia: The inability to sleep can both be a symptom and a cause of increased hyperarousal, creating a vicious cycle.
- Substance use: Alcohol, caffeine, nicotine, and recreational drugs can activate the nervous system, contributing to feelings of arousal and exacerbating existing hyperarousal.
Hyperarousal in PTSD: The Core Symptom You Can’t Ignore
When diagnosing post-traumatic stress disorder (PTSD), doctors typically look for several key symptoms, and hyperarousal is prominent among them. It’s not just an adjunct symptom; it’s a central feature that significantly impacts a person’s life.
In PTSD, hyperarousal manifests as a persistent feeling of being under threat, even when objective danger is absent. This includes:
- Hypervigilance: Being constantly on guard and excessively watchful for signs of danger. Research shows approximately 70% of individuals who have experienced trauma, including sexual assault, report symptoms of hypervigilance and hyperarousal. This heightened state of sensitivity to our senses makes us react strongly to potential threats.
- Exaggerated startle response: Reacting strongly to sudden noises or movements.
- Difficulty concentrating: The mind is too busy scanning for threats to focus on tasks.
- Sleep disturbances: Trouble falling or staying asleep, and restless sleep, often plagued by nightmares.
- Irritability and angry outbursts: A low tolerance for frustration, leading to sudden bursts of anger.
- Self-destructive or reckless behavior: Some individuals might engage in risky activities, perhaps as a way to feel something other than fear, or to escape their internal state.
These aren’t just “bad habits”; they’re deeply ingrained responses stemming from a nervous system that believes it’s still in danger. The chronic nature of these symptoms can be incredibly debilitating. For more in-depth information on how hyperarousal plays a role in PTSD, you can read more about PTSD and hyperarousal in our related article: PTSD Symptoms: Hyperarousal, Nightmares, and Feeling On Edge.
The molecular underpinnings of hyperarousal in PTSD are complex, involving imbalances in neurochemical systems and structural changes in the brain. For example, the hypothalamic-pituitary-adrenal (HPA) axis, responsible for stress response, can become dysregulated, leading to abnormal cortisol levels. Neurotransmitters like glutamate and GABA, which regulate excitatory and inhibitory signals in the brain, can also be imbalanced. Additionally, genetic factors, such as polymorphisms in genes like COMT (Catechol-O-Methyltransferase), can influence an individual’s susceptibility to hyperarousal and other PTSD symptoms after trauma. This indicates that our biology significantly interacts with environmental stressors to shape our vulnerability and response to trauma.
The Hyperarousal-Insomnia Trap

Can’t fall asleep? Mind racing at 2 a.m.? You’re caught in the hyperarousal-insomnia trap, and it’s a brutal cycle. Hyperarousal is considered the core symptom of insomnia disorder, affecting about 10% of the general population. Our research shows that people with insomnia score significantly higher on the hyperarousal factor than controls at all times of the day. This isn’t just about being “stressed before bed”; it’s a 24-hour phenomenon.
Here’s how it works: your body, stuck in that fight-or-flight mode, perceives bedtime not as a time for rest, but as another potential threat. Your brain won’t shut down, leading to:
- Difficulty initiating sleep: You lie awake, thoughts swirling, unable to quiet your mind.
- Difficulty maintaining sleep: You wake frequently, easily startled, and struggle to return to sleep.
- Non-restorative sleep: Even if you get some hours, you wake feeling unrefreshed because your body was still on high alert.
What’s particularly insidious is how hyperarousal changes throughout the day. In both individuals with insomnia and controls, the hyperarousal factor score tends to peak in the morning and wane throughout the day. However, for people with insomnia, the overnight increase in hyperarousal is significantly stronger. This means they wake up feeling even more keyed up than controls, setting the stage for another day of liftd stress and another night of poor sleep.
This overnight surge in hyperarousal is strongly linked to subjective sleep quality. The worse an individual perceives their sleep to be, the stronger the increase in hyperarousal they experience by morning. This highlights a critical insight: improving sleep quality isn’t just about feeling rested; it’s a direct pathway to reducing daytime hyperarousal.
The Real Cost: How Hyperarousal Wrecks Your Life
When your body is constantly primed for danger, it’s not just uncomfortable—it actively sabotages your life. The pervasive nature of hyperarousal means it infiltrates every corner of your existence, slowly eroding your well-being.

- Work and productivity: Constant tension and difficulty concentrating make it nearly impossible to perform at your best. Deadlines become impossible, focus is a distant dream, and your professional life suffers.
- Relationships: Your irritability and quick temper can push loved ones away. Paranoia makes trust difficult, and your inability to relax makes genuine connection feel impossible. Hyperarousal can affect relationships and how individuals respond to others, often leading to regrettable outbursts.
- Social life: Avoiding social situations feels safer, leading to isolation. The energy required to “mask” your internal state is too much, so you withdraw.
- Emotional well-being: You might feel “broken” or fundamentally flawed, leading to feelings of shame, guilt, and hopelessness. This constant internal battle is mentally exhausting.
If you are juggling demanding work or school in Florida cities like Tampa, Miami, Orlando, or Jacksonville, this impact can feel even more intense. That is why many adults and young professionals in these areas seek structured support through programs like Virtual IOP or PHP at Thrive.
Long-Term Health Risks If You Ignore It
Ignoring chronic hyperarousal isn’t just about feeling bad; it has serious physical consequences. Your body wasn’t designed for perpetual fight-or-flight, and the strain takes a toll.
- Chronic pain: Persistent muscle tension can lead to widespread, unexplained pain.
- Cardiovascular issues: The constant liftd heart rate and blood pressure increase your risk for high blood pressure and other heart problems.
- Metabolic disorders: Prolonged high levels of stress due to hyperarousal can contribute to an increased risk for Type 2 diabetes.
- Emotional burnout: Your emotional reserves are depleted, leading to exhaustion, detachment, and an inability to cope with even minor stressors.
For individuals in high-stress jobs throughout Florida, these risks can be even more pronounced. The combination of occupational demands and underlying hyperarousal creates a perfect storm for long-term health complications. Early, evidence-based treatment can significantly lower these risks and improve quality of life.
7 Ways to Take Back Control from Hyperarousal—Starting Now
If you’re in crisis, call or text 988 right now. You are not alone.
You don’t have to live with the constant drain and distress of hyperarousal. There are proven strategies and treatments that can help you calm your nervous system, reclaim your peace, and live a fuller life.
Professional Treatment: Get Expert Help That Works
While self-management is important, hyperarousal often requires the guidance of mental health professionals. Effective treatment approaches often combine:
- Trauma-focused therapy: These therapies are specifically designed to help you process traumatic experiences and retrain your brain’s response to stress.
- Cognitive Behavioral Therapy (CBT): Helps you identify and change negative thought patterns and behaviors contributing to hyperarousal.
- Exposure Therapy: Gradually exposes you to trauma-related memories or situations in a safe, controlled environment to reduce fear responses. Virtual reality programs can be effectively used in exposure therapy.
- Eye Movement Desensitization and Reprocessing (EMDR): Combines exposure therapy with guided eye movements to help reprocess traumatic memories.
- Medication management: A psychiatrist can prescribe medications to help manage specific hyperarousal symptoms.
- Antidepressants (SSRIs/SNRIs): Can ease anxiety, depression, and improve sleep and concentration. Sertraline and paroxetine are FDA-registered for PTSD treatment.
- Anti-anxiety medications: Can provide short-term relief for extreme anxiety, though long-term use is typically avoided due to abuse potential.
- Prazosin (Minipress): Can specifically help reduce or stop nightmares in people with PTSD.
- Novel agents: Research is ongoing into treatments like ketamine, which shows promise in rapidly reducing symptoms by acting on NMDA receptors, and glutamate-modulating drugs like lamotrigine and memantine, which can help stabilize brain activity. These are cutting-edge options that your provider may discuss with you.
At Thrive Mental Health, we offer comprehensive virtual and hybrid IOP (Intensive Outpatient) and PHP (Partial Hospitalization) programs, as well as flexible Virtual Therapy for ongoing support. These programs provide a higher level of care than traditional weekly therapy, combining clinical expertise with flexible scheduling, including evening options, to fit your life. Our programs are designed for people who need more than once-a-week therapy but less than inpatient care. We serve individuals across Florida, and our services are often covered by major insurance providers such as Cigna, Optum, and Florida Blue.
To explore your options and begin your journey to recovery, verify your insurance in 2 minutes on our website.
Self-Help Strategies You Can Start Today
While professional support is vital, there are many actionable steps you can take at home to manage hyperarousal symptoms:
- Breathing exercises: Slowing down your breath directly impacts your nervous system, moving you away from the fight-or-flight response. Techniques like diaphragmatic breathing can be incredibly calming. Breathing exercises are a powerful tool to help your body calm down.
- Meditation for grounding: In hyperarousal, thoughts, emotions, and sensations can clutter your mind. Meditation helps clear this clutter, allowing you to stay present and reduce the intensity of internal distress. Meditation can help you find clarity.
- Stress management tips: Everyone experiences stress, but with hyperarousal, its effects linger long after the trigger. Learning and implementing effective stress management techniques is crucial for long-term relief. Stress management is an important part of feeling better.
- Sensory stimulation for short-term relief: When you feel overwhelmed by hyperarousal, powerful sensory input can “reset” your nervous system.
- Suck on a very sour candy or strong mint.
- Drink very cold liquid, like ice water.
- Place an icepack or cool washcloth on your face, the back of your neck, or the inside of your wrist.
- Take a cool shower.
- Cut back on stimulants: Substances like caffeine and nicotine activate your nervous system, directly contributing to feelings of arousal. Limiting or avoiding them can significantly reduce your baseline hyperarousal.
- Avoid recreational drugs and alcohol: While they might offer temporary escape, these substances can worsen hyperarousal and impede long-term healing.
- Regular exercise: Physical activity is a natural stress reliever and can help discharge pent-up energy from your activated nervous system.
- Sleep hygiene: Establish a consistent sleep schedule, create a relaxing bedtime routine, and ensure your sleep environment is conducive to rest. Addressing the hyperarousal-insomnia trap is key to restorative sleep.
- Build a strong support system: Spend time with supportive people and consider joining a PTSD support group. Connection can be a powerful antidote to isolation.
Planning ahead with self-management items for known stressful events, like carrying sour candy or a small ice pack for a concert or a challenging family gathering, can empower you to manage symptoms as they arise.
FAQs: Hyperarousal—What People Like You Ask Most
Can hyperarousal go away on its own?
Rarely. While occasional stress responses might fade, chronic hyperarousal typically doesn’t resolve without intervention. Without action, it usually gets worse, becoming deeply ingrained. Professional help combined with consistent self-care strategies are key to managing and reducing symptoms.
Is hyperarousal the same as anxiety?
No. Hyperarousal is a physiological state of heightened alertness and reactivity, a physical manifestation of your body’s stress response. Anxiety, on the other hand, is primarily an emotional state characterized by worry, unease, and fear. While hyperarousal is a core component and symptom of anxiety disorders and PTSD, they are not the same thing. You can experience hyperarousal without consciously feeling anxious, and vice versa.
How does hyperarousal ruin sleep?
Hyperarousal keeps your body and mind on high alert, making it nearly impossible to fall or stay asleep. Your brain perceives bedtime as a threat, preventing it from shutting down. This leads to racing thoughts, physical tension, and an exaggerated startle response, all of which disrupt the natural sleep cycle. Studies show that people with insomnia experience a stronger overnight increase in hyperarousal compared to those without sleep issues, demonstrating this direct link.
Does insurance cover treatment for hyperarousal?
Yes, most insurance plans, including major providers like Cigna, Optum, and Florida Blue, cover treatment for mental health conditions that involve hyperarousal, such as PTSD and anxiety disorders. This often includes psychotherapy, medication management, and structured programs like Intensive Outpatient (IOP) and Partial Hospitalization (PHP). We encourage you to check your coverage now to understand your benefits.
Can virtual therapy or IOP help with hyperarousal?
Absolutely. Thrive Mental Health’s virtual and hybrid programs, including Virtual IOP, PHP, and Virtual Therapy, are highly effective in treating hyperarousal and related conditions. Our programs offer evidence-based therapies like CBT and EMDR, medication management, and skill-building for stress management, all delivered by expert clinicians. The virtual format provides flexibility and accessibility, allowing you to engage in treatment from the comfort of your home anywhere in Florida, often with evening options to fit your schedule.
Conclusion: You Don’t Have to Live in Fight-or-Flight Mode
Living with hyperarousal is exhausting, feeling like you’re constantly running a marathon without moving. But it’s crucial to remember that this isn’t a permanent state. Your internal alarm system can be recalibrated. With the right support, strategies, and professional guidance, you can learn to calm your nervous system, process underlying trauma, and regain a sense of safety and control in your life.
At Thrive Mental Health, we are dedicated to helping you achieve this. Our virtual and hybrid IOP/PHP programs and Virtual Therapy offer the comprehensive, evidence-based care you need, delivered by compassionate experts. We understand the unique challenges of hyperarousal and are here to provide a path forward for individuals throughout Florida.
Summary: Hyperarousal is your body’s stress alarm stuck on high, but it is treatable. With a mix of professional treatment (like IOP/PHP), lifestyle changes, and nervous-system-calming skills, you can reduce symptoms, sleep better, and feel in control again.
Ready for support? Thrive offers virtual and hybrid IOP/PHP programs with evening options. Verify your insurance in 2 minutes (no obligation) → Start benefits check or call 561-203-6085. If you’re in crisis, call/text 988.