Navigating Trauma: Specialized Therapies for Every Age and Family

Why Trauma Therapy for Teens Is More Critical Than Ever
Trauma therapy for teens addresses the deep emotional wounds that can shape your child’s future. If your teenager has withdrawn from family, lost interest in activities they once loved, or is struggling with anger and anxiety, you’re not alone—and there’s help.
What you need to know right now:
- 1 in 4 young people experience a significantly traumatic event during childhood or adolescence
- Trauma-focused CBT (TF-CBT) and EMDR therapy are the only two treatments recommended by the World Health Organization for teens with trauma
- Symptoms lasting more than a month require professional intervention—don’t wait
- Evidence-based treatment typically takes 16-20 sessions and includes parent involvement
- Dual diagnosis programs are essential when trauma co-occurs with substance abuse
Trauma doesn’t just hurt—it rewires the developing teenage brain. The good news? With the right approach, healing is possible. This guide will walk you through recognizing the signs, understanding evidence-based treatment options, and knowing when to seek help for your teen.
I’m Nate Raine, CEO of Thrive Mental Health, and over the past decade I’ve worked at the intersection of behavioral health innovation and clinical care, focusing on expanding access to evidence-based trauma therapy for teens right here in Florida. My goal is to help you understand what works and how to find the right support for your family.
Key trauma therapy for teens vocabulary:
- Somatic Therapy vs. EMDR: Which is Right For You?
- Is EMDR Right for Everyone? The Science Behind the Debate
- How Somatic Therapy Works
Is Your Teen Suffering from Unseen Wounds? Recognizing the Signs of Trauma
When a teen experiences a traumatic event, their world can be turned upside down. The emotional and psychological response can be profound, leading to lasting mental health symptoms. It’s crucial for us to understand that trauma doesn’t just affect adults; it impacts developing brains differently, often manifesting in ways that might be misinterpreted as typical teenage angst or defiance. The adolescent brain is still maturing, particularly the prefrontal cortex responsible for decision-making and emotional regulation, making teens especially vulnerable to the lasting effects of trauma.
Trauma can trigger the body’s primitive fight-flight-freeze response, leading to a state of chronic stress that can literally alter brain structure. This constant state of alert can make it incredibly difficult for teens to feel safe, trust others, or manage daily stressors. Recognizing these signs is the first step toward finding effective trauma therapy for teens.
The National Institute of Mental Health (NIMH) advises that while many reactions to traumatic events are normal and will lessen with time, if symptoms last for more than a month, families should reach out to a healthcare provider. This is a critical indicator that professional intervention is needed. For a comprehensive overview of how children and adolescents respond to traumatic events, we recommend reviewing A guide for parents on adolescent trauma responses.

Emotional and Behavioral Symptoms to Watch For
Trauma in adolescents often presents as a complex mix of emotional and behavioral changes. These aren’t just “bad behaviors”; they are often unconscious coping mechanisms developed in response to overwhelming experiences. We often see:
- Irritability and mood swings: Teens may become easily frustrated, quick to anger, or experience rapid shifts in mood.
- Social withdrawal: A desire to isolate from friends and family, losing interest in activities they once enjoyed.
- Anger outbursts: Uncharacteristic explosions of anger or aggression, often triggered by seemingly minor events.
- Avoidance of triggers: Going to great lengths to avoid places, people, conversations, or situations that remind them of the traumatic event.
- Loss of interest in hobbies: Apathy towards school, sports, creative pursuits, or anything that previously brought joy.
- Risky behaviors: Engaging in impulsive or dangerous activities, including reckless driving, unprotected sex, or self-harm.
- Substance use: Turning to drugs or alcohol to self-medicate or escape painful memories and emotions. This is a significant concern, as trauma and substance abuse often go hand-in-hand in teenagers.
- Changes in eating/sleeping patterns: Significant alterations in appetite (eating too much or too little) or sleep disturbances (insomnia, nightmares, sleeping excessively).
- Difficulty concentrating: Struggling with schoolwork, remembering information, or staying focused on tasks.
- Increased anxiety and fear: Persistent worries, panic attacks, or a generalized sense of dread.
These symptoms can seriously impact a teen’s academic performance, social relationships, and overall well-being.
How Trauma Manifests Physically in Adolescents
Trauma isn’t just a mental or emotional experience; it deeply impacts the body. Teens may experience a range of physical symptoms directly linked to their traumatic experiences. These are not imaginary but real physiological reactions to a dysregulated nervous system. We often observe:
- Headaches and stomachaches: Frequent, unexplained pains that are not relieved by typical remedies.
- Chronic fatigue: Persistent tiredness or lack of energy, even after adequate sleep.
- Racing heart: Episodes of rapid heartbeat or palpitations, often accompanied by feelings of anxiety.
- Being easily startled: An exaggerated startle response to sudden noises or movements.
- Emotional numbness: A sense of detachment from their own body or emotions, sometimes described as feeling “empty” or “disconnected.”
- Muscle tension: Chronic tightness in the shoulders, neck, or jaw.
These physical manifestations underscore the profound, holistic impact of trauma and highlight the need for integrated, comprehensive trauma therapy for teens.
What is Trauma-Informed Therapy for Teens and Why Is It Critical for Healing?
Trauma-informed therapy for teens is not just a set of techniques; it’s a fundamental shift in how we approach care. At its core, trauma-informed practice is a way of being in relationship to others that supports safety, choice, and healing, benefiting everyone regardless of one’s life history. It acknowledges the widespread impact of trauma and understands potential paths for recovery, recognizing the signs and symptoms of trauma in clients, families, staff, and others involved with the system. Most importantly, it actively resists re-traumatization.
This approach is critical because it creates an environment where healing can truly begin. It moves beyond simply treating symptoms to addressing the root causes of distress, fostering resilience, and empowering teens to regain control over their lives. For a deeper dive into how we tailor treatment to individual needs, explore More info about our treatment modalities.
Here’s a comparison of traditional vs. trauma-informed therapy approaches:
| Feature | Traditional Therapy | Trauma-Informed Therapy |
|---|---|---|
| Primary Question | “What’s wrong with you?” | “What happened to you?” |
| Focus | Symptom reduction, behavior modification | Understanding trauma’s impact, building safety, processing experiences, developing coping skills |
| Client Role | Passive recipient of treatment | Active collaborator in healing, empowered to make choices |
| Therapist Role | Expert, problem-solver | Guide, facilitator, creating a safe and transparent environment |
| View of Behavior | Often seen as pathology or resistance | Understood as a coping mechanism or adaptation to trauma |
| Risk of Re-traumatization | Higher, due to potential for power imbalances or lack of sensitivity to triggers | Minimized through explicit attention to safety, trust, and client empowerment |
| Core Principles | Diagnosis-driven, therapist-led | Safety, trustworthiness, peer support, collaboration, empowerment, cultural/historical/gender issues |
The Core Difference: “What Happened to You?” vs. “What’s Wrong with You?”
This shift in perspective is perhaps the most profound aspect of trauma-informed care. Instead of asking “What’s wrong with you?”—a question that can imply blame and further shame—we ask “What has happened to you?” This simple change reorients the entire therapeutic process. It recognizes that challenging behaviors are often adaptive responses to overwhelming or threatening experiences.
By understanding behavior as a coping mechanism, we can approach teens with empathy and validation, rather than judgment. This builds a strong therapeutic alliance, a critical component for effective trauma therapy for teens. It allows us to help teens make sense of their experiences, develop healthier coping strategies, and ultimately heal. As the experts at Heart Mind Online explain, Supporting teens with a trauma-informed approach isn’t about being perfect; it’s about consistently prioritizing safety, choice, and healing in every interaction.
The Gold Standard: Evidence-Based Trauma Therapies That Actually Work
When it comes to trauma therapy for teens, relying on evidence-based approaches is paramount. We want to ensure that the interventions we use have been rigorously tested and proven effective. The good news is that there are highly effective modalities specifically designed for young people.
In 2013, the World Health Organization (WHO) examined existing literature and recommended only two treatment options for children and adolescents with PTSD: Trauma-Focused Cognitive Behavioral Therapy (TF-CBT) and Eye Movement Desensitization and Reprocessing (EMDR) therapy. A 2018 meta-analysis reviewing research on both TF-CBT and EMDR for children and adolescents who experienced trauma confirmed that both are effective in reducing symptoms, with TF-CBT potentially being slightly more effective.
The goal of these therapies isn’t to erase painful memories—that’s often impossible. Instead, it’s about processing those memories, reducing their emotional charge, and integrating the traumatic experience into a teen’s life story in a way that no longer dominates their present or dictates their future. We tailor treatment to each teen’s unique needs and experiences, often within our structured programs. Learn more about More info about our intensive outpatient programs.
Trauma-Focused Cognitive Behavioral Therapy (TF-CBT) for Teens
Trauma-Focused Cognitive Behavioral Therapy (TF-CBT) is widely considered the most empirically supported treatment for PTSD in adolescents. Developed in 1996 by psychiatrist Dr. Judith A. Cohen and psychologists Dr. Anthony P. Mannarino and Dr. Esther Deblinger, TF-CBT is a specialized form of CBT designed exclusively for children and adolescents aged 3 to 18 who have experienced trauma. It combines CBT techniques with elements of play and family therapy, adapting to the developmental needs of young people.
TF-CBT typically occurs over an average of 16 sessions with a psychologist, though the duration can vary. It’s a components- and phase-based treatment that involves both individual sessions with the teen and parallel sessions with parents or caregivers, often including conjoint sessions. The model is built around eight core components, often remembered by the acronym “PRACTICE”:
- Psychoeducation and parenting skills: Helping teens and parents understand trauma and its effects, and teaching parents how to support their child.
- Relaxation techniques: Teaching coping skills like deep breathing and progressive muscle relaxation to manage anxiety and stress.
- Affective expression and regulation: Helping teens identify, express, and manage their emotions in healthy ways.
- Cognitive coping and processing: Identifying and challenging unhelpful thoughts related to the trauma, and developing more balanced perspectives.
- Trauma narration and processing: Gradually and safely telling the story of the traumatic event, which helps integrate the memory and reduce its emotional power.
- In-vivo exposure: Gradually confronting safe situations, places, or reminders that have been avoided due to trauma.
- Conjoint parent/child sessions: Facilitating communication and support between the teen and their caregiver regarding the trauma.
- Enhancing personal safety and future growth: Developing safety plans, social skills, and strategies for continued growth and resilience.
TF-CBT is effective for diverse types of traumas and has been rigorously tested in numerous studies worldwide. For more details on the research supporting this approach, see Scientific research on TF-CBT for youth.
Eye Movement Desensitization and Reprocessing (EMDR)
Eye Movement Desensitization and Reprocessing (EMDR) therapy is another highly effective and WHO-recommended treatment for trauma in teens. Created by psychologist Dr. Francine Shapiro in 1989, EMDR helps teens process traumatic memories by using bilateral stimulation, such as guided eye movements, taps, or tones. This stimulation is believed to help the brain reorganize how memories are stored, reducing their emotional intensity without overwhelming the teen.
EMDR typically follows an eight-phase approach:
- History-taking and treatment planning: Understanding the teen’s trauma history and developing a treatment plan.
- Preparation: Teaching stress management tools and building a safe, trusting therapeutic relationship.
- Assessment: Identifying specific traumatic memories, associated negative beliefs, and desired positive beliefs.
- Desensitization: Using bilateral stimulation while the teen focuses on the traumatic memory, reducing its emotional charge.
- Installation: Strengthening positive beliefs to replace negative ones.
- Body scan: Checking for any remaining physical sensations related to the trauma.
- Closure: Ensuring the teen feels grounded and stable before the session ends.
- Reevaluation: Reviewing progress and planning for future sessions.
EMDR is particularly powerful for teens who struggle with vivid flashbacks, intense emotional distress, or who haven’t found relief with traditional talk therapy. It helps transform harmful thought patterns into positive beliefs, empowering teens to move forward.
Treating Complex Trauma and Co-Occurring Substance Abuse
Some teens experience what we call “complex trauma,” which often results from multiple, chronic, and prolonged traumatic events, such as ongoing abuse or neglect. This can lead to pervasive regulation problems across multiple domains, including affect, attachment, behavior, biology, cognition, and perception. Teens with complex trauma may also have experienced “poly-victimization”—exposure to many different types of victimization.
For these teens, the impact is often deeper and more entrenched, requiring a specialized and often longer-term approach to trauma therapy for teens. The National Child Traumatic Stress Network (NCTSN) recommends a multimodal trauma-informed approach called Integrative Treatment of Complex Trauma for Adolescents (ITCT-A), which combines several therapeutic modalities including cognitive therapy, exposure therapy, and mindfulness.
A significant concern for teens with trauma, especially complex trauma, is the co-occurrence of substance abuse. Research shows that trauma and substance abuse often go hand-in-hand as teens try to cope with inner turmoil, self-medicate, or escape reality. This can lead to chemical dependency, and we often see many signs of substance abuse overlapping with PTSD symptoms.
When a mental health issue like PTSD co-occurs with chemical dependency, it’s known as a dual diagnosis. In such cases, dual diagnosis treatment is essential. This integrated approach addresses both conditions simultaneously, recognizing that they are intertwined and must be treated holistically for lasting recovery. Our specialized programs in Florida are designed to address these complex needs, providing comprehensive, local support for teens and families across the state facing both trauma and substance use challenges.
Your Role in Their Recovery: How to Support Your Teen at Home
Your involvement as a parent or caregiver is invaluable in your teen’s healing journey. Creating a safe, predictable, and supportive environment at home can significantly bolster the effects of trauma therapy for teens. We understand that this can be incredibly challenging, especially if you yourself are feeling overwhelmed. You don’t have to be perfect; your consistent presence and effort make a profound difference.

Here are key ways you can support your teen:
- Create a safe and supportive environment: Ensure your teen feels physically and emotionally secure. This means minimizing conflict, providing consistent routines, and offering a comforting presence.
- Maintain routines: Predictability helps counteract the chaos that trauma can create. Stick to regular schedules for meals, sleep, and activities whenever possible.
- Active listening: When your teen chooses to talk, listen without judgment. Validate their feelings, even if you don’t fully understand them. Avoid minimizing their experiences or telling them how they “should” feel.
- Validate feelings without judgment: Let them know that whatever they are feeling—anger, sadness, fear, numbness—is okay. “It makes sense that you feel that way after what you’ve been through.”
- Limit exposure to repetitive news: Especially after a community or large-scale traumatic event, reduce their exposure to constant media coverage, which can re-traumatize.
- Encourage expression: While you shouldn’t force them to talk, create opportunities for them to express themselves through writing, drawing, music, or other creative outlets.
- Help them feel in control: Allow them to make small decisions where appropriate, giving them a sense of agency that trauma often strips away.
- Monitor for changes: Continue to observe their behavior, mood, and sleep patterns. If symptoms worsen or new concerns arise, communicate with their therapist.
Sometimes, teens require a more structured environment to process trauma and develop healthy coping mechanisms. Our More info about our partial hospitalization programs can offer this level of care, providing intensive support while allowing teens to remain at home.
Practical Coping Skills and Grounding Techniques for Teens
Teaching and practicing coping skills and grounding techniques are vital components of trauma therapy for teens. These tools empower teens to manage overwhelming emotions, reduce distress, and stay connected to the present moment.
Here are some practical strategies:
- Grounding Techniques: These help teens return to the “here and now” when they feel overwhelmed, disconnected, or caught in a flashback.
- The 5-4-3-2-1 Method: Identify 5 things you can see, 4 things you can touch, 3 things you can hear, 2 things you can smell, and 1 thing you can taste. This engages all senses to anchor them to reality.
- The Butterfly Hug: Cross your arms over your chest, placing each hand on the opposite shoulder or upper arm. Gently tap one hand, then the other, in a rhythmic, alternating pattern. This bilateral stimulation can be very calming.
- Mindful Breathing: Simple deep breathing exercises can regulate the nervous system. Teach them to breathe in slowly through their nose for a count of four, hold for a count of four, and exhale slowly through their mouth for a count of six.
- Progressive Muscle Relaxation (PMR): Tense and then relax different muscle groups throughout the body, starting from the toes and working up to the head. This helps teens recognize and release physical tension.
- Encouraging Healthy Outlets:
- Art and creative expression: Drawing, painting, writing poetry, or playing music can be powerful ways to process emotions without words.
- Exercise and movement: Physical activity is a natural stress reliever. Encourage walking, running, dancing, or sports.
- Journaling: Writing about their experiences and feelings in a private space can significantly improve psychological health.
- Connecting with nature: Spending time outdoors can be incredibly grounding and soothing.
We encourage teens to build a “Feelings Survival Kit” – a collection of these and other personalized strategies they can use when difficult emotions arise. The key is consistent practice, so these tools become second nature when needed most.
Frequently Asked Questions about Trauma Therapy for Teens
How long does trauma therapy for teens usually take?
The duration of trauma therapy for teens can vary based on the individual’s needs, the type and severity of trauma, and the specific therapeutic modality used. However, evidence-based models like Trauma-Focused Cognitive Behavioral Therapy (TF-CBT) often average around 16 to 20 sessions. For teens dealing with complex trauma, which involves multiple or prolonged traumatic experiences, treatment may require a longer-term commitment, potentially extending to 25-30 sessions or more. The focus is always on achieving meaningful progress and building lasting skills, rather than adhering to a fixed timeline.
Can trauma cause real physical symptoms in teenagers?
Absolutely. Trauma has a profound impact on the body’s physiological systems. When a teen experiences trauma, their nervous system can become dysregulated, leading to a chronic “fight-flight-freeze” response. This constant state of alert can manifest in a variety of physical symptoms, including frequent headaches, stomachaches, chronic fatigue, a racing heart, muscle tension, and being easily startled. These symptoms are not “just in their head” but are real, measurable physiological reactions to the trauma. Addressing these physical manifestations is an important part of comprehensive trauma therapy for teens.
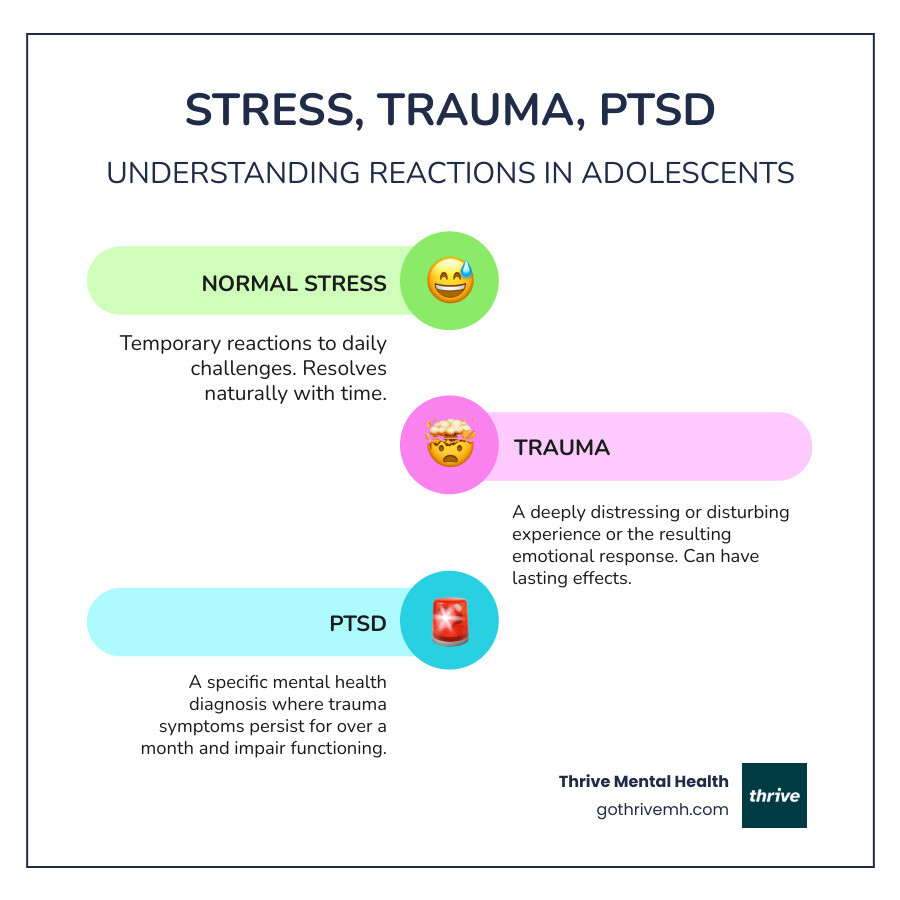
What is the difference between trauma and PTSD?
Trauma refers to the distressing event or series of events itself, and the immediate emotional and psychological response to it. This could be anything from a single incident like an accident or natural disaster to ongoing experiences like abuse or neglect. Post-Traumatic Stress Disorder (PTSD), on the other hand, is a specific mental health diagnosis that can develop after experiencing trauma. It’s characterized by a distinct cluster of symptoms that persist for more than a month, including intrusive thoughts (flashbacks, nightmares), avoidance of trauma-related reminders, negative changes in thoughts and mood, and hyperarousal (being easily startled, irritability, difficulty sleeping). Not everyone who experiences trauma will develop PTSD, but anyone experiencing significant distress after a traumatic event can benefit from trauma therapy for teens.
Take the First Step Toward Healing
Healing from trauma is a journey, not a destination, and the right support makes all the difference. For teens in Florida struggling with the weight of trauma, especially when it co-occurs with other mental health challenges, a higher level of care like an Intensive Outpatient Program (IOP) or Partial Hospitalization Program (PHP) can provide the structured, local support needed to build coping skills and process difficult experiences. Thrive Mental Health offers expert-led, evidence-based programs specifically for Florida teens and families. We understand the unique challenges facing adolescents in our communities, and our programs are designed to foster resilience and lasting recovery.
Ready for support? Thrive offers virtual and hybrid IOP/PHP programs with evening options. Verify your insurance in 2 minutes (no obligation) → Start benefits check or call 561-203-6085. If you’re in crisis, call/text 988.