Is It OCD or Just Me Being Me?

Do I Have OCD: Unlock the Truth 2025
Understanding When Thoughts and Behaviors Become a Concern
If you’re wondering do I have OCD, you’re not alone. Many people struggle to understand whether their repetitive thoughts and behaviors are part of their personality or signs of Obsessive-Compulsive Disorder.
Quick Answer: Signs You Might Have OCD
- Intrusive thoughts that feel impossible to control or ignore
- Compulsive behaviors you feel driven to perform repeatedly
- Time consumption – symptoms take up 1+ hours daily or significantly interfere with life
- Distress – these thoughts and behaviors cause genuine anxiety and suffering
- Recognition – you know the thoughts/behaviors are excessive but can’t stop them
The line between “just being thorough” and having OCD isn’t always clear. About 1 in 40 adults in the US live with OCD, making it far more common than many people realize. Unlike perfectionism or general anxiety, OCD involves unwanted intrusive thoughts (obsessions) that trigger repetitive behaviors (compulsions) in an endless cycle.
Many people dismiss their symptoms, thinking they’re just “quirky” or “detail-oriented.” But if unwanted thoughts are consuming your time, causing distress, or interfering with work and relationships, it may be time to dig deeper.
I’m Nate Raine, CEO of Thrive Mental Health, where I’ve helped countless individuals across Florida steer the question “do I have OCD” and find effective treatment paths. Through my work in behavioral health, I’ve seen how proper diagnosis and evidence-based treatment can transform lives when OCD symptoms feel overwhelming.
Do i have ocd word roundup:
What Are the Core Symptoms of OCD?
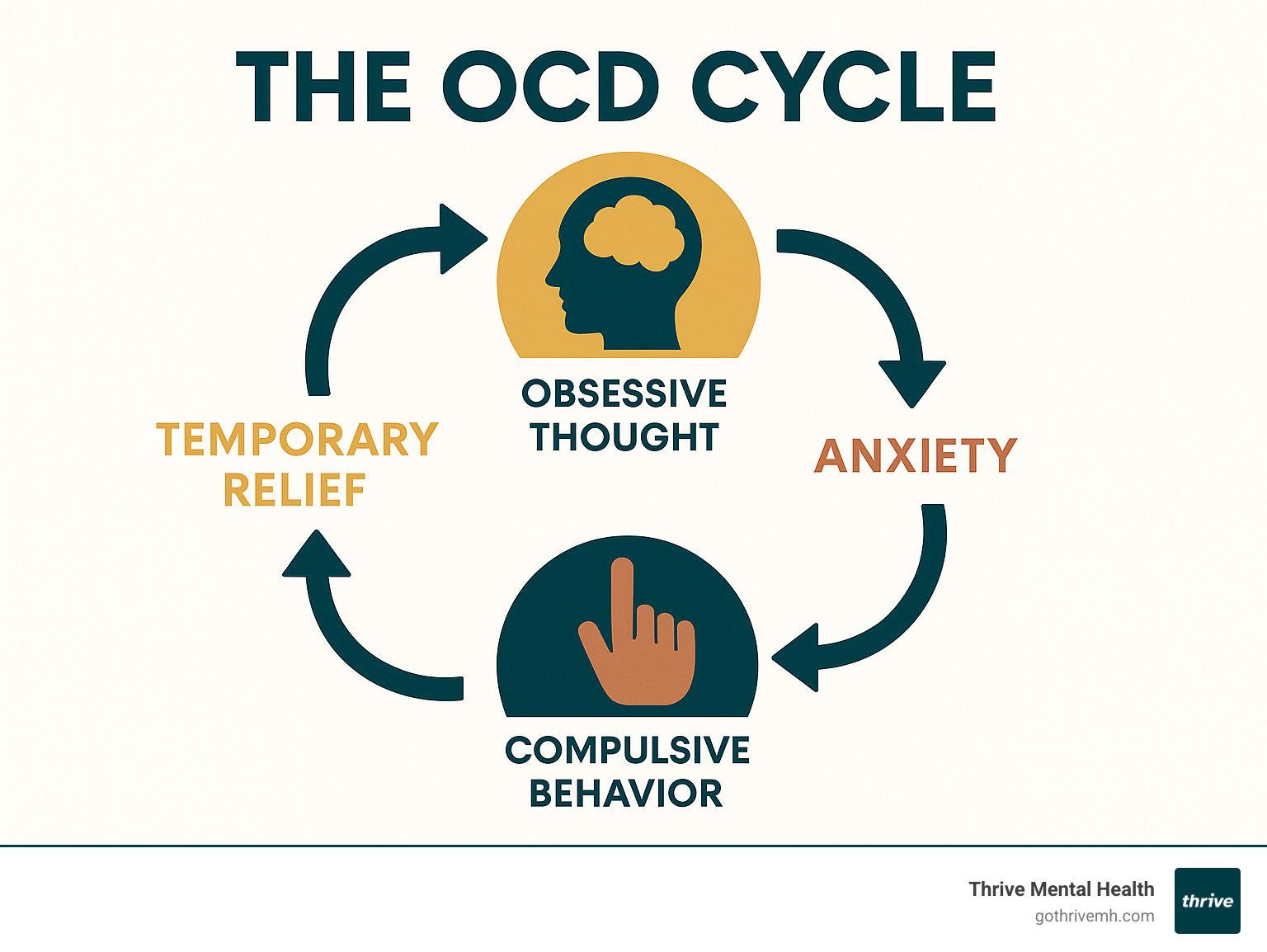
If you’re asking yourself “do I have OCD?” understanding the core symptoms is crucial. OCD isn’t just about being neat or organized – it’s a mental health condition driven by two main components that feed off each other: obsessions and compulsions.
It’s like a mental hamster wheel: distressing thoughts trigger behaviors for temporary relief, but the cycle repeats. This isn’t something you can control through willpower alone.

What Are Obsessions?
Obsessions are unwanted, intrusive, and persistent thoughts, images, or urges that are anxiety-provoking and feel impossible to ignore. Most people with OCD know these thoughts are irrational, which can make them even more frustrating, but obsessions don’t respond to logic.
Fear of contamination involves overwhelming worries about germs, dirt, or getting sick from touching everyday objects. This can include fears of specific substances or of contaminating others.
Fear of harm involves disturbing thoughts about accidentally or intentionally harming yourself or loved ones. These thoughts are highly distressing because they oppose your values, but having them does not make you dangerous.
Need for symmetry or order is an overwhelming urge for things to be “just right.” This can manifest as needing perfect alignment or symmetry to prevent intense discomfort or a feeling that something terrible will happen.
Taboo thoughts include unwanted sexual, religious, or violent images that are deeply upsetting because they contradict your moral beliefs.
Persistent doubt keeps you questioning whether you’ve completed important tasks, like turning off the stove. The uncertainty feels unbearable, despite logic.
For a comprehensive look at how these symptoms manifest, check out our detailed guide on OCD Symptoms.
What Are Compulsions?
Compulsions are the behaviors or mental acts you feel driven to perform in response to obsessions. They are your brain’s attempt to neutralize the anxiety, but the relief is only temporary. You might know they don’t make logical sense, but the anxiety feels so intense that you feel you must do them.
Excessive cleaning or washing goes far beyond normal hygiene, such as washing hands until they’re raw or cleaning surfaces repeatedly. The fear feels real, even if the behavior seems excessive.
Checking behaviors involve repeatedly verifying that doors are locked, appliances are off, or that you haven’t made a mistake, far beyond what is necessary.
Counting, ordering, and arranging are compulsions that involve performing tasks a specific number of times or arranging objects in precise patterns. These rituals feel necessary to prevent a feared event or to relieve discomfort.
Reassurance seeking means constantly asking others to confirm that everything is okay (e.g., “Are you sure I didn’t say anything offensive?”).
Mental rituals are invisible compulsions performed in your head, such as repeating phrases, counting, or mentally reviewing events to neutralize anxiety.
The key difference from regular habits is the distress and time consumed. If you spend hours daily on these behaviors or skipping them causes intense anxiety, it may be time to explore whether you have OCD.
To better understand the broader context of these symptoms, visit our resource on the Meaning of OCD.
How Is OCD Different From Perfectionism or Anxiety?
When you’re asking yourself “do I have OCD,” it’s natural to wonder if what you’re experiencing is just everyday anxiety or perfectionism. The key difference lies in what’s driving these behaviors and how much distress they cause.
A perfectionist wants a project to be excellent; someone with general anxiety worries about the future. In OCD, the thoughts feel intrusive and unwanted, and the behaviors aren’t about achieving a positive goal—they’re about desperately trying to quiet an internal alarm.
For example, someone might tidy their desk for better focus. A person with OCD, however, might feel a terrifying urge to arrange their desk in a specific way, believing that failing to do so will cause harm to a loved one. The compulsion is driven by intense, irrational fear, not productivity.
| Characteristic | Obsessive-Compulsive Disorder (OCD) | Perfectionism (Personality Trait) | General Anxiety (Disorder) |
|---|---|---|---|
| Thought Type | Intrusive, unwanted, often disturbing (e.g., harm, contamination). | High standards, desire for flawlessness (e.g., perfect work). | Broad worries about future events, health, finances (e.g., what if?). |
| Motivation for Behavior | Reduce intense anxiety/distress from obsessions, prevent feared outcomes. | Achieve high standards, avoid mistakes, produce excellent results. | Avoid potential threats, cope with uncertainty. |
| Behavioral Response | Compulsive, ritualistic, often irrational behaviors or mental acts. | Meticulous attention to detail, repeated checking for errors, over-preparation. | Avoidance, seeking reassurance, planning, rumination. |
| Level of Distress | Significant distress, anguish, and impairment. Behaviors are ego-dystonic (against one’s will). | Can be stressful, but often ego-syntonic (aligned with self-image). | Moderate to high, but typically less ritualistic than OCD. |
| Awareness of Irrationality | Often aware that thoughts/behaviors are irrational or excessive. | Usually sees behaviors as rational and beneficial. | May recognize worries are excessive, but struggles to control them. |
| Impact on Life | Consumes significant time (1+ hour/day), severely impairs daily functioning, relationships, work/school. | Can be productive, but may lead to burnout or procrastination. | Can impair functioning, but often less ritualistic and time-consuming. |
Anxiety often co-occurs with OCD, but the ritualistic responses to specific intrusive thoughts are what make OCD unique. If you’re struggling with broader anxiety symptoms, our Anxiety Symptoms page can help clarify the differences.
When Do These Behaviors Become a Disorder?
The line between quirky habits and a clinical disorder is about how much they take over your life. According to the DSM-5, your experiences cross into OCD territory when they meet these criteria:
Time consumption becomes significant. Obsessions and compulsions take up more than an hour per day, interfering with daily activities.
The distress is real and intense. The thoughts and behaviors cause genuine suffering, not just mild annoyance. They often lead to exhaustion and frustration.
Your daily life takes a hit. Work, social life, and relationships suffer. You may begin to avoid people, places, or situations that trigger your symptoms, making your world feel smaller.
This functional impairment is crucial. If you like things neat but can go about your day normally, it’s likely a personality trait. But if these patterns are interfering with your ability to enjoy life, it’s time to take them seriously.
For a deeper understanding of how OCD impacts daily functioning, visit our Understanding OCD page.
What Are the Common Types of OCD?
OCD varies widely in its specific themes, but the underlying cycle of obsession and compulsion is the same.
Contamination OCD involves fears of germs, dirt, or illness, leading to compulsions like excessive hand washing or constant cleaning.
Checking OCD involves persistent doubts about safety (e.g., locking doors, turning off appliances), leading to repetitive checking.
Symmetry and Ordering OCD is a need for things to feel “just right,” leading to arranging objects or performing tasks in specific ways to quiet an internal sense of wrongness.
Ruminations and Intrusive Thoughts (sometimes called “Pure O”) involve mental obsessions (e.g., about violence, sex, or religion) with less visible compulsions, like mentally “undoing” thoughts.
Harm OCD centers on intrusive thoughts about harming yourself or others, which are highly distressing because they oppose your values. Compulsions often involve avoidance.
Scrupulosity is an excessive worry about morality or religious correctness, leading to compulsions like repetitive prayer or confession.
Hoarding behaviors involve difficulty discarding possessions due to intense distress. While now its own disorder, it shares features with OCD.
Many people experience symptoms from multiple categories. The specific content matters less than the underlying pattern of distress and impairment.
Why Might I Have OCD? Understanding Causes and Diagnosis
The question “Why me?” is natural when you’re wondering do I have OCD. The truth is, OCD doesn’t have a single cause; it’s more like a perfect storm of factors. Think of it as a combination of genetic predispositions, brain chemistry, and stressful life events.

Understanding these factors can help you feel less alone and more hopeful about treatment.
What Are the Potential Causes and Risk Factors?
While we can’t pinpoint an exact cause, research has identified several key risk factors.
Genetics and family history play a significant role. OCD often runs in families. If a parent or sibling has OCD, your risk is about 25%. This suggests a genetic vulnerability, though it doesn’t guarantee you’ll develop the disorder.
Brain biology and chemistry differences are another piece of the puzzle. People with OCD often show differences in brain communication, like an overactive “error detection system.” Imbalances in the brain chemical serotonin, which helps regulate mood and anxiety, also appear to play a role.
Childhood trauma and stressful life events can act as triggers. Major life changes or trauma don’t cause OCD, but they can trigger its onset in predisposed individuals.
Temperament also matters. Certain temperaments, like being an anxious child or highly sensitive to uncertainty, can increase vulnerability to developing OCD.
There’s also PANDAS syndrome, which affects some children. In these rare cases, OCD symptoms suddenly appear or worsen following a strep infection, showing how infections can sometimes be a trigger.
Having these risk factors doesn’t mean you’re destined to have OCD. It’s simply a complex interplay of factors.
How Do Professionals Diagnose if I Have OCD?
If you’re seriously wondering do I have OCD, getting a professional evaluation is the most important step. While it can feel scary, mental health professionals are there to help, not judge.
There’s no single test for OCD. Diagnosis relies on a thorough evaluation process:
- Clinical Interview: A professional will ask detailed questions about your thoughts, behaviors, family history, and how symptoms affect your life.
- Psychological Assessments: Tools like The Obsessive-Compulsive Inventory can help clarify symptoms but are not a diagnosis on their own. They are a starting point for discussion.
- Ruling Out Other Conditions: A clinician will rule out other conditions with similar symptoms, like anxiety disorders or depression, to ensure an accurate diagnosis.
- DSM-5 Criteria: The diagnosis is confirmed if your experiences meet the DSM-5 criteria: obsessions and/or compulsions that are time-consuming (1+ hour/day), cause significant distress, and impair daily functioning.
It’s crucial to be honest during the evaluation, even about embarrassing thoughts. Professionals understand that distressing, value-conflicting thoughts are a core part of OCD and will not judge you.
Getting a proper diagnosis can be a relief. Finally having a name for what you’re experiencing, and knowing that effective treatments exist, can be the first step toward getting your life back. If you’re in Florida and ready to take that step, our team can provide a comprehensive evaluation to see if our OCD treatment programs are the right fit for you.
So, Do I Have OCD? What Are My Next Steps?
If these symptoms resonate with you, recognizing that you might have OCD is a brave and important first step. It can feel overwhelming, but it’s the start of breaking free from the cycle of obsessions and compulsions.

The question do I have OCD deserves a professional answer, but understanding your treatment options can help you feel more confident about taking that next step.
What Are the Most Effective Treatments if I Think I Have OCD?
The good news is that OCD is highly treatable. The right approach, often combining therapy and medication, leads to significant improvement for most people.
Psychotherapy is a primary treatment. Cognitive Behavioral Therapy (CBT) helps you understand the connection between your thoughts, feelings, and behaviors. Our Cognitive Behavioral Therapy page explains this approach.
The gold standard for OCD is Exposure and Response Prevention (ERP). This specialized therapy involves gradually facing your fears while resisting the urge to perform compulsions. For instance, someone with contamination fears might touch a doorknob and resist washing their hands. This process is challenging but proves you can handle the anxiety without the ritual.
Medication can also be highly effective. SSRIs (Selective Serotonin Reuptake Inhibitors) like fluvoxamine, sertraline, and fluoxetine are a common first choice. For OCD, they are often used at higher doses and may take 8-12 weeks to become fully effective.
Many people find that combining ERP therapy with medication gives them the best results. For treatment-resistant cases, advanced, FDA-approved options like rTMS and DBS are also available.
Self-care habits like regular exercise, good sleep, and stress management can also support your recovery. For more insights, check out our Mental Health Therapy page.
What Is the Outlook for Someone With OCD?
OCD is typically a chronic condition, but this means it’s manageable, not hopeless. With proper treatment, most people experience significant symptom reduction.
Your quality of life can improve dramatically, allowing you to refocus on work, relationships, and personal goals. Symptoms may flare up during stressful times, but with treatment, you’ll have the tools to manage these challenges effectively.
Early intervention makes a huge difference. The sooner you start treatment, the better your outcomes tend to be. Managing OCD is a lifelong journey of wellness, and many people develop incredible resilience and self-awareness through their recovery.
How to Find Specialized OCD Help in Florida
If you’re in Florida, finding specialized help for OCD is a crucial step. While your primary care doctor can be a good starting point for a referral, it’s essential to connect with a mental health professional specifically trained in evidence-based OCD treatments like ERP.
At Thrive Mental Health, we make it easy to access this specialized care. Our team includes therapists with deep expertise in treating OCD. We offer several programs tailored to your needs:
- Virtual Therapy: Our Virtual Intensive Outpatient Program (IOP) provides access to top OCD specialists from anywhere in Florida. Whether you’re in Tampa Bay, Central Florida, or another part of the state, you can receive expert care without the commute.
- Structured Support: For those needing consistent, structured care, our Outpatient Programs offer a supportive environment for recovery.
In addition to professional treatment, support groups can be validating. The International OCD Foundation is an excellent resource for finding peer support.
Seeking help isn’t admitting defeat—it’s choosing to fight for your well-being. You deserve to live free from the exhausting cycle of OCD, and expert help is available right here in Florida.
Conclusion
If you’ve made it this far, you’ve taken an important step in understanding whether do I have OCD. The journey to self-awareness isn’t always easy, but it’s incredibly brave.
We’ve walked through the difference between everyday quirks and genuine OCD symptoms – those intrusive obsessions and time-consuming compulsions that can hijack your daily life. We’ve explored how OCD differs from perfectionism or general anxiety, and most importantly, we’ve discussed when these patterns cross the line from personality traits into a treatable mental health condition.
Here’s what matters most: if your thoughts and behaviors are eating up hours of your day, causing you real distress, or preventing you from living the life you want, you deserve support. This isn’t about being “too sensitive” or needing to “just get over it.” OCD is a real condition that responds incredibly well to proper treatment.
The hope in all of this? Treatment works. With evidence-based approaches like Exposure and Response Prevention therapy and the right professional support, people with OCD can reclaim their time, reduce their distress, and get back to what truly matters to them.
At Thrive Mental Health, we understand that seeking help can feel overwhelming – especially when OCD might be making even simple decisions feel impossible. That’s why we’ve designed our care to be as accessible as possible. Whether through our Virtual Intensive Outpatient Program (IOP) that you can access from anywhere in Florida, or our specialized Exposure and Response Prevention Therapy, we’re here to meet you where you are.
Taking that first step toward getting help isn’t just about managing symptoms – it’s about choosing to be in control of your own life again. You don’t have to figure this out alone, and you don’t have to suffer in silence.
Ready to learn more? We’re here when you’re ready to take that next step.