Intervene Like You Mean It: Understanding Crisis Intervention Mental Health Services

Crisis Intervention Mental Health Services: 24/7 Lifesaving Support
When Mental Health Becomes an Emergency
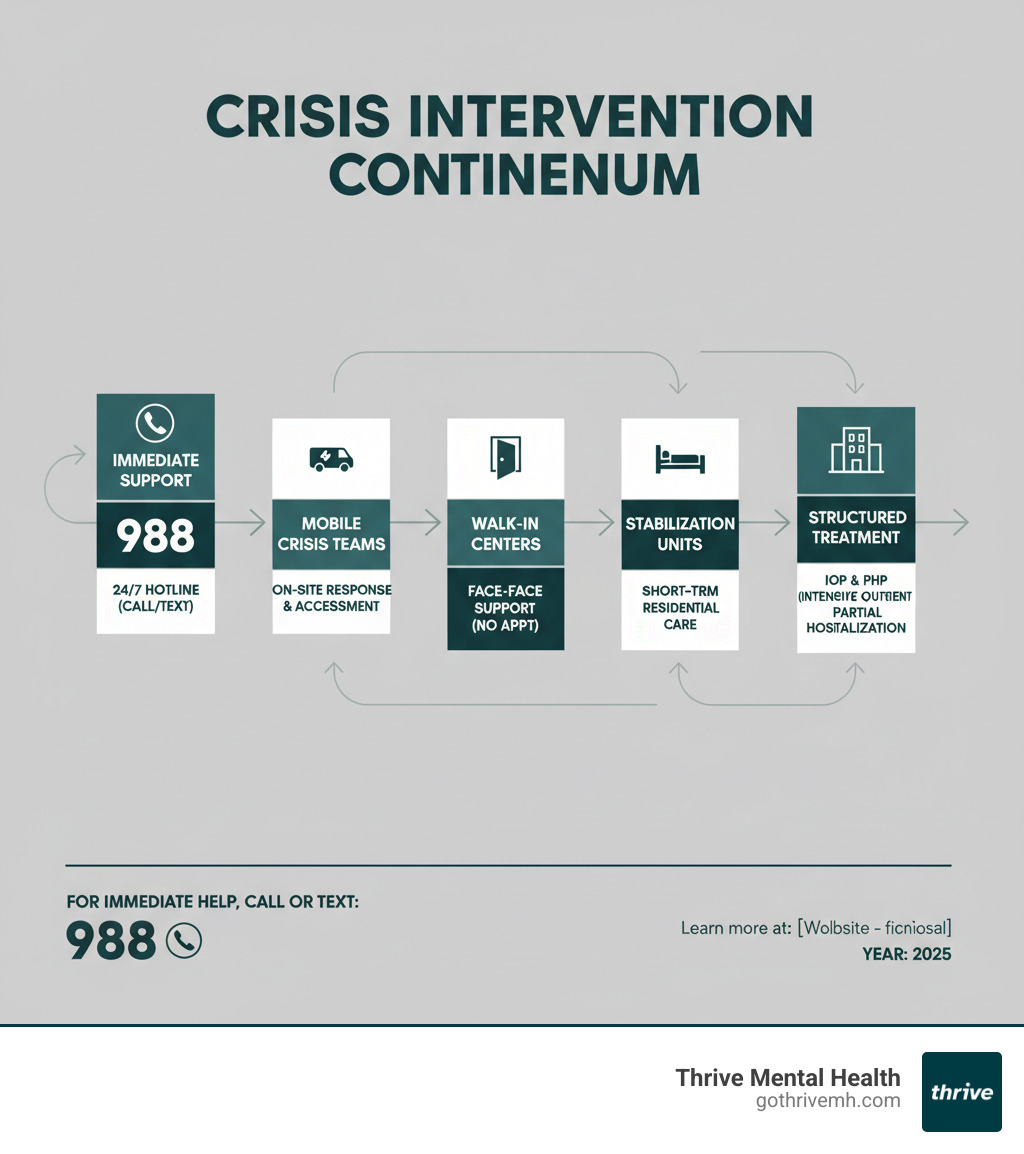
Crisis intervention mental health services provide immediate, life-saving support when emotional distress becomes an emergency. These services bridge the gap between routine mental health care and the ER, offering rapid stabilization and a path to ongoing treatment. They include:
- 24/7 Crisis Hotlines: Immediate phone and text support, like the 988 Suicide & Crisis Lifeline.
- Mobile Crisis Teams: On-site response in your community.
- Walk-In Crisis Centers: Face-to-face support without an appointment.
- Crisis Stabilization Units: Short-term residential care to avoid hospitalization.
- Intensive Outpatient/Partial Hospitalization Programs (IOP/PHP): Structured treatment to prevent future crises.
A crisis occurs when a person’s coping skills are overwhelmed by what feels like an unbearable situation. This isn’t just a bad day; it’s an urgent state that can involve suicidal thoughts, psychosis, or severe episodes of depression or mania. According to the National Institute of Mental Health, over 14 million U.S. adults have a serious mental condition, and with suicide rates rising, access to these services is critical.
If you or someone you know is in immediate danger, call 911. For mental health crises, call or text 988.
I’m Anna Green, LMHC, LPC, founder and Chief Clinical Officer of Thrive Mental Health. I’ve dedicated my career to developing evidence-based crisis intervention mental health services, including our virtual IOP and PHP programs, to prevent hospitalization and connect people to the right level of care.
What is a Mental Health Crisis? Recognizing the Red Flags
If you’re in crisis, call/text 988 right now. You are not alone.
A mental health crisis occurs when emotional pain becomes so intense it overwhelms your ability to cope. It’s more than a bad day; it’s a situation where a person’s feelings and behaviors put them at risk of harming themselves or others, or they become unable to care for their basic needs. Triggers can include trauma, substance use, job loss, or a flare-up of a pre-existing mental health condition.
Recognizing a crisis early is key to getting help fast.
Emotional and Behavioral Signs
Watch for these red flags, which can appear suddenly or build over time:
- Intense Sadness or Hopelessness: A pervasive despair that interferes with daily life, often expressed with phrases like “nothing will ever get better.”
- Overwhelming Anxiety or Panic Attacks: Episodes of intense fear with physical symptoms like a racing heart, shortness of breath, or a feeling of impending doom.
- Extreme Irritability or Anger: Uncharacteristic explosive outbursts or a constant, simmering rage.
- Social Withdrawal: Isolating from friends and family, canceling plans, and avoiding social contact.
- Risky or Impulsive Behaviors: Actions with little regard for consequences, such as self-harm, reckless driving, or substance abuse.
- Significant Changes in Sleep or Appetite: Drastic shifts like sleeping all day, insomnia, or major weight changes.
- Expressions of Self-Harm or Suicide: Talking about wanting to die, feeling like a burden, giving away possessions, or researching methods. This is the most critical warning sign.
- Psychotic Symptoms: Paranoia, suspiciousness, or experiencing hallucinations or delusions (seeing, hearing, or believing things that aren’t real).
Common Types of Crises
Crisis intervention mental health services are equipped to handle various emergencies:
- Suicidal Ideation and Behavior: Ranges from passive thoughts of death to active planning. All mentions of suicide require an immediate, serious response.
- Psychotic Episodes: A break from reality involving hallucinations, delusions, and disorganized thinking.
- Severe Depression: A profound low mood that makes basic self-care (showering, eating) feel impossible.
- Manic Episodes: Abnormally high energy and mood leading to impulsive decisions, reckless behavior, and little need for sleep.
- Panic Attacks: Sudden, intense fear that triggers severe physical reactions without a real threat.
- Substance-Induced Crises: Acute mental health symptoms like psychosis or severe anxiety triggered by drug or alcohol use or withdrawal.

Swift intervention dramatically improves outcomes. Understanding these signs helps you know when to call 988, visit a crisis center, or connect with intensive outpatient programs for ongoing support.
The First Response: How to Help Someone in Crisis
When someone is in a mental health crisis, your response can be life-saving. You don’t need to be a professional to help. Your goal is to create safety, show compassion, and connect them to professional crisis intervention mental health services.
Immediate Steps to Take
If you or a loved one are in immediate danger, call 911. For urgent mental health support, call or text the 988 Suicide & Crisis Lifeline.
- Ensure Safety: The first priority is safety for everyone. If you can do so safely, remove any weapons, medications, or other means of harm from the area.
- Stay Calm: Your calm presence can be grounding. Speak gently and avoid rushing.
- Listen Without Judgment: Put your phone away and give them your full attention. Let them talk without offering advice or trying to “fix” it. Simply being heard is powerful.
- Ask Directly About Suicide: If you are concerned about suicide, ask directly: “Are you thinking about ending your life?” This does not plant the idea; it shows you care and opens the door for them to talk about it.
- Validate Their Feelings: Use phrases like, “This sounds incredibly painful,” instead of “It’s not that bad.” Acknowledge that their pain is real to them.
- Don’t Leave Them Alone: Stay with them until professional help arrives or the immediate danger has passed. Offer to help them call a crisis line or drive them to get help.
Crisis Intervention vs. Suicide Prevention
While related, these two concepts have different focuses:
| Feature | Crisis Intervention | Suicide Prevention |
|---|---|---|
| Primary Goal | Stabilize the immediate crisis and connect to ongoing care. | Ensure immediate safety from self-harm and prevent future attempts. |
| Scope | Addresses any acute mental health distress (e.g., psychosis, severe anxiety, manic episodes, trauma). | Specifically targets individuals at risk of suicide. |
| Timeframe | Short-term, immediate response to an acute situation. | Can involve immediate response, but also long-term strategies and education. |
| Techniques Used | De-escalation, safety planning, assessment, brief counseling, referral to various mental health services. | Risk assessment, safety planning, means restriction, supportive counseling, connecting to suicide-specific resources (e.g., 988). |
| Overlap | A suicide crisis is a type of mental health crisis, so crisis intervention will often include suicide prevention strategies. | Suicide prevention efforts often involve crisis intervention techniques to manage immediate risk. |
In practice, many mental health crises involve suicide risk, so professionals use techniques from both. The key is connecting the person to the right level of care.
The Spectrum of Care: Types of Crisis Intervention Mental Health Services
Crisis intervention mental health services operate on a spectrum, offering different levels of support to meet you where you are. This continuum provides a safety net, from immediate phone support to structured daily programs that help rebuild your life.

Immediate Support: Hotlines, Walk-In Clinics, and Mobile Teams
These services are the first line of defense when a crisis hits:
- 24/7 Crisis Helplines: The 988 Suicide & Crisis Lifeline offers free, confidential support anytime by calling or texting 988. For text-based support, you can also text “HELLO” to 741741 to reach the Crisis Text Line.
- Walk-In Crisis Centers: These centers provide immediate, face-to-face evaluation, brief therapy, and referrals without an appointment, serving as an alternative to an ER visit.
- Mobile Crisis Teams: Mental health professionals respond to your location in the community, providing on-site assessment, de-escalation, and connection to care. This approach reduces police involvement and is increasingly available across Florida.
Short-Term Stabilization: Bridging the Gap to Recovery
When a crisis requires more than immediate support, these services offer a bridge to recovery:
- Crisis Stabilization Units (CSUs): Short-term residential facilities that provide intensive support, therapy, and medication management in a safe, less restrictive environment than a hospital.
- Respite Care: Offers a therapeutic “timeout” in a supportive, home-like setting to help you stabilize away from daily stressors.
- Inpatient Hospitalization: The highest level of care, reserved for when a person is an immediate danger to themselves or others and requires 24/7 supervision and intensive treatment.
Structured Treatment: IOP and PHP for Crisis Intervention Mental Health Services
Once the immediate crisis is stable, structured programs are key to building lasting recovery and preventing future crises.
Intensive Outpatient Programs (IOP) and Partial Hospitalization Programs (PHP) provide comprehensive care for several hours a day, multiple days a week, while you continue to live at home. These programs are vital for crisis intervention mental health services as they can:
- Serve as a step-down from hospitalization, easing the transition back to daily life.
- Act as an alternative to hospitalization for those who need intensive care but can remain safely at home.
- Focus on crisis prevention by teaching coping skills and addressing underlying conditions through evidence-based therapies.
At Thrive Mental Health, our virtual and in-person IOP and PHP programs offer this structured support with flexible scheduling, including evening options, to fit your life. Curious how virtual programs work? Explore more resources on our blog.
Accessing Care: How to Find and Pay for Services
Finding the right crisis intervention mental health services can feel overwhelming, but help is more accessible than you might think.

Finding Help in Your Area
Here’s where to start looking for support:
- National Lifelines: Call or text 988 to reach the Suicide & Crisis Lifeline for any mental health crisis. You can also text “HELLO” to 741741 to connect with the Crisis Text Line.
- Local Resources: Dial 211 to connect with local mental health services, crisis centers, and support programs in your community.
- Community Organizations: Your local public health department, university counseling center (for students), and chapters of NAMI (National Alliance on Mental Illness) are excellent resources for finding local care.
- State-Specific Services: Residents in Florida can access a robust network of community mental health centers and mobile crisis response teams.
Thrive Mental Health offers virtual IOP and PHP services across Florida, with local access points in major areas including Tampa Bay, St. Petersburg, Miami, and Orlando.
Navigating Insurance for Crisis Intervention Mental Health Services
Don’t let cost be a barrier. Crisis intervention mental health services are often covered better than you expect.
The Mental Health Parity Act requires most insurance plans to cover mental health care at the same level as medical care. This means your co-pays, deductibles, and treatment limits should be comparable.
Always check if a provider is in-network with your insurance to keep costs down. Before starting treatment, verify your benefits by asking your insurance provider: What are my mental health benefits? Is IOP or PHP covered? What is my deductible and co-pay?
Major insurers like Cigna, Optum, Florida Blue, and Aetna often cover IOP and PHP because they are effective alternatives to more expensive hospitalization. At Thrive, we work with these providers and can help you verify your insurance coverage online in minutes.
Frequently Asked Questions about Crisis Intervention
What is the first step in crisis intervention?
The first step is always to ensure physical safety for everyone involved. Once the environment is safe, a crisis counselor will work to build trust, listen actively to understand the person’s needs, and de-escalate the immediate distress to a calmer state before planning next steps.
Can you be forced into mental health treatment during a crisis?
Yes, but only under strict legal conditions. Involuntary commitment (or a psychiatric hold) can occur if a qualified professional determines a person is an immediate danger to themselves or others, or is “gravely disabled” and unable to care for their basic needs. Laws vary by state; in Florida, this process is governed by the Baker Act and involves professional assessment and legal oversight. Voluntary treatment is always the preferred goal.
How long do crisis intervention services last?
Crisis intervention is designed to be short-term. A crisis hotline call may last from minutes to an hour. A stay in a Crisis Stabilization Unit (CSU) is typically a few days. The goal is not long-term treatment but to stabilize the immediate crisis and connect the person to ongoing care, such as therapy or an Intensive Outpatient Program (IOP).
How can family and friends support someone experiencing a mental health crisis?
Your support is crucial. Stay calm, listen without judgment, and validate their feelings. Offer practical help, like calling a crisis line with them or driving them to a clinic. Ask directly about suicide if you are concerned, and do not leave them alone if you believe they are at risk. Encouraging them to get professional help is the most supportive action you can take.
What is the role of mobile crisis teams in mental health crisis intervention?
Mobile crisis teams bring mental health professionals directly to a person’s location in the community. They provide on-the-spot assessment, de-escalation, and brief counseling. A key benefit is reducing police involvement in mental health emergencies, offering a more compassionate and appropriate response. Their goal is to stabilize the situation and connect the person to community resources, often preventing unnecessary ER visits or hospitalizations.
{
"@context": "https://schema.org",
"@type": "FAQPage",
"mainEntity": [
{
"@type": "Question",
"name": "What is the first step in crisis intervention?",
"acceptedAnswer": {
"@type": "Answer",
"text": "Ensure physical safety first. Then a trained counselor builds rapport, listens to immediate needs, and de-escalates before planning next steps."
}
},
{
"@type": "Question",
"name": "Can you be forced into mental health treatment during a crisis?",
"acceptedAnswer": {
"@type": "Answer",
"text": "Yes, but only under strict legal conditions. In Florida, the Baker Act allows for involuntary commitment if a person is a danger to themselves or others, or is gravely disabled. The process has strict legal oversight."
}
},
{
"@type": "Question",
"name": "How long do crisis intervention services last?",
"acceptedAnswer": {
"@type": "Answer",
"text": "They are short-term: hotline calls last minutes to an hour; Crisis Stabilization Units are typically a few days, with referrals to ongoing care like IOP/PHP."
}
},
{
"@type": "Question",
"name": "How can family and friends support someone in crisis?",
"acceptedAnswer": {
"@type": "Answer",
"text": "Stay calm, listen without judgment, validate feelings, ask directly about suicide if concerned, and do not leave them alone until safe. Help connect them to professional care."
}
},
{
"@type": "Question",
"name": "What do mobile crisis teams do?",
"acceptedAnswer": {
"@type": "Answer",
"text": "They respond on-site with assessment, de-escalation, brief counseling, and referrals—often preventing unnecessary ER visits and reducing police involvement."
}
}
]
}
Conclusion: Your Path Forward from Crisis to Stability
A mental health crisis can feel isolating, but it is a temporary state, not a final destination. You now have a roadmap for recognizing the warning signs, responding with compassion, and connecting to the right level of care.
The system of crisis intervention mental health services is more accessible than ever, with a spectrum of options from the 988 lifeline and mobile crisis teams to structured programs like IOP and PHP that build long-term stability. Recovery is not just possible; it’s happening every day for people who take the brave step of asking for help.
Seeking support is an act of courage. At Thrive Mental Health, our virtual and in-person IOP and PHP programs in Florida are designed to provide the right intervention at the right time, helping you move from crisis to stability. These services open the door to ongoing support, community, and the tools you need to thrive.
Ready for support? Thrive offers virtual and hybrid IOP/PHP with evening options. Verify your insurance in 2 minutes (no obligation) → Start benefits check or call 561-203-6085. If you’re in crisis, call/text 988.