From Obsessions to Freedom: Treating OCD Effectively

Your First Step to Freedom from OCD
If you or someone you know is in crisis or having thoughts of suicide, please call or text 988 to reach the Suicide and Crisis Lifeline. You are not alone.
How to Treat OCD in 2025: Proven Steps That Cut Symptoms by 50–70%
Summary: If you’re searching for how to treat OCD, the most effective, evidence-based options are Exposure and Response Prevention (ERP) therapy and medication (usually SSRIs). Many people see 50–70% symptom reduction with the right treatment plan combining therapy, medication, and support.
How to treat OCD involves a combination of evidence-based therapies and medications that can help you break free from the cycle of obsessions and compulsions. The most effective approaches include:
Primary OCD Treatments:
- Exposure and Response Prevention (ERP) – The gold standard therapy with 50-60% success rates.
- Selective Serotonin Reuptake Inhibitors (SSRIs) – First-line medications that reduce symptoms by 40-60%.
- Cognitive Behavioral Therapy (CBT) – Helps change thought patterns and behaviors.
- Combined treatment – Therapy plus medication benefits about 70% of cases.
Advanced Options for Severe Cases:
- Transcranial Magnetic Stimulation (TMS)
- Deep Brain Stimulation (DBS)
- Intensive outpatient programs
Obsessive-Compulsive Disorder affects millions of Americans, creating a relentless cycle of unwanted thoughts and repetitive behaviors. These intrusive thoughts can consume hours of your day and significantly impact your quality of life.
The good news? OCD is highly treatable. Research consistently shows that with the right approach, most people experience significant symptom reduction. Treatment helps many people, even those with severe OCD, regain control over their lives.
I’m Anna Green, LMHC, LPC, Chief Clinical Officer at Thrive Mental Health. With over a decade specializing in evidence-based care, I’ve seen how the right treatment approach can transform lives. Our virtual programs make quality care accessible, and I’ve witnessed firsthand how they restore hope for those struggling with OCD in Florida and other states we serve.
Related content about how to treat ocd:
Understanding and Diagnosing OCD: What You Need to Know
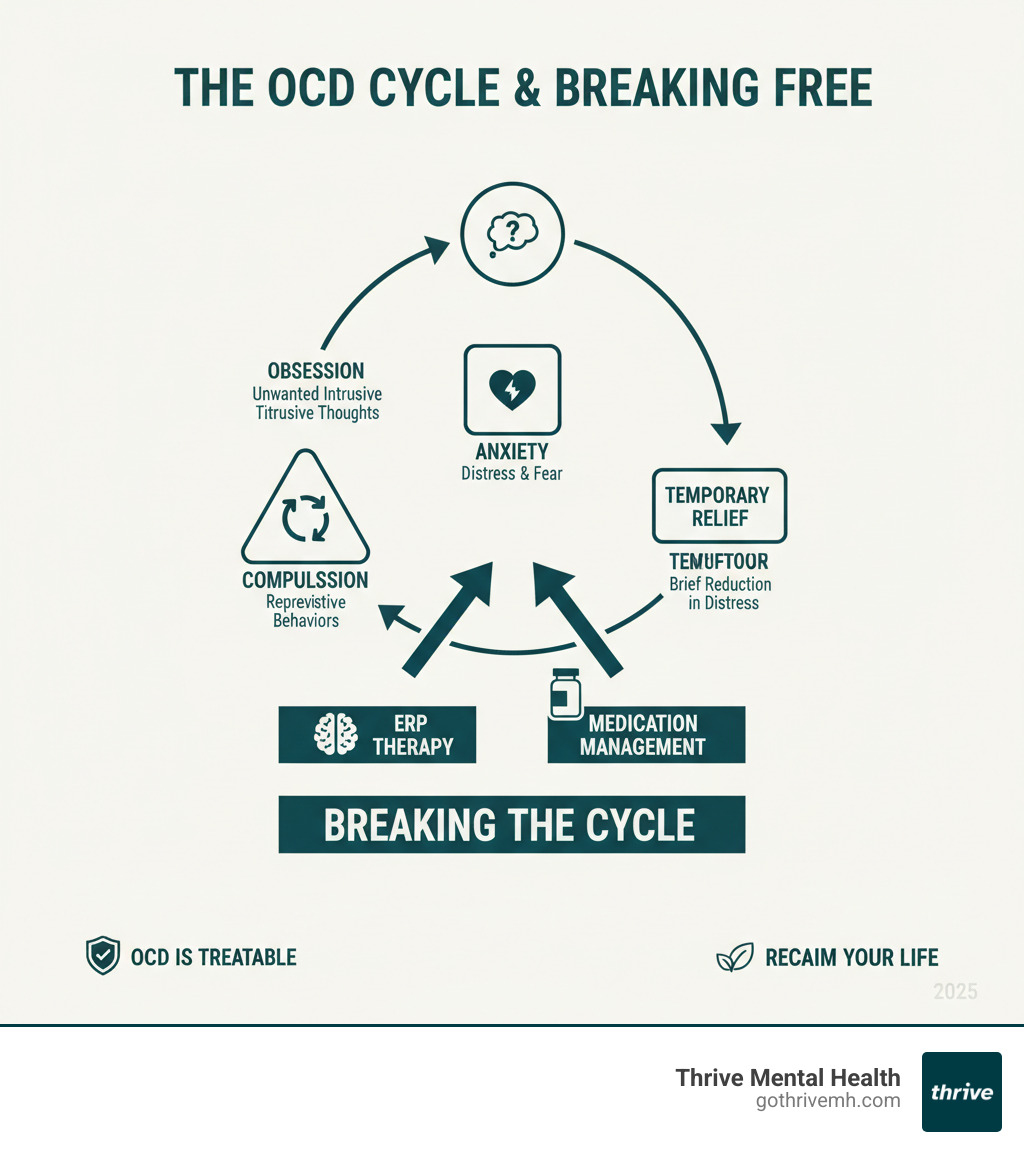
How to treat OCD starts with understanding the condition. Obsessive-Compulsive Disorder is a mental health condition where unwanted thoughts (obsessions) create intense anxiety, leading to repetitive behaviors (compulsions) for temporary relief. This cycle can hijack your brain’s problem-solving system, making it feel impossible to break free. Understanding the mechanics behind OCD is the first step toward effective treatment.

Is It OCD? Recognizing the Signs and Symptoms
The difference between OCD and simple habits is control and distress. With OCD, you feel you have no choice.
Obsessions are intrusive, distressing thoughts on repeat, often contrary to your values. Common themes include contamination, unwanted thoughts of harm, or a need for things to be “just right.”
Compulsions are the behaviors you perform to reduce the anxiety from obsessions. Examples include excessive washing, repeated checking of locks or appliances, arranging items until they feel right, or counting.
OCD symptoms are distinguished from habits because they take up more than an hour a day, cause significant distress, and interfere with your life. If you’re spending substantial time managing these thoughts and behaviors, it’s time to seek support. For a deeper dive, see our guide to OCD Symptoms.
The Path to an Official Diagnosis
An official diagnosis can be a relief, providing a name for your experience and a path to proven treatments. The process typically involves:
- A psychological evaluation: A mental health professional will ask about your specific obsessions and compulsions to understand their impact on your life. Honesty is key to getting the right help.
- A physical exam: This helps rule out other medical issues, like thyroid problems, that can mimic OCD symptoms.
- The DSM-5 criteria: This is the official framework for diagnosis. It requires that obsessions or compulsions are time-consuming (over an hour daily), cause distress or impairment, and aren’t due to other conditions.
Early diagnosis is important, as untreated OCD can become more complex over time.
| Feature | Obsessive-Compulsive Disorder (OCD) | Obsessive-Compulsive Personality Disorder (OCPD) |
|---|---|---|
| Nature of Symptoms | Intrusive, unwanted thoughts and repetitive behaviors performed to reduce anxiety | Pervasive pattern of preoccupation with orderliness, perfectionism, and control |
| Personal Experience | Symptoms feel distressing and unwanted (ego-dystonic) | Traits often feel acceptable or desirable (ego-syntonic) |
| Awareness | Usually aware symptoms are problematic and seeks help | Often unaware behaviors are problematic for others |
| Focus | Specific intrusive thoughts and rituals | General personality traits like extreme conscientiousness |
| Motivation | Driven by anxiety and fear of negative outcomes | Driven by desire for control and perfection |
What Causes OCD? The Role of Genetics, Biology, and Environment
OCD develops from a combination of factors, which helps explain why various treatments are effective.
- Genetics: A family history of OCD increases your risk, suggesting a genetic predisposition.
- Brain Structure and Function: People with OCD often have an overactive “alarm system” in their brain that detects threats everywhere, with an underactive “off switch” for repetitive behaviors. This is a key finding from scientific research on OCD brain activity.
- Serotonin: This neurotransmitter helps regulate mood and anxiety. The effectiveness of medications that target serotonin suggests it plays a key role in OCD.
- Temperament and Trauma: Anxious temperaments and childhood trauma can increase risk by making the brain’s threat-detection system more sensitive.
- PANDAS: In some children, sudden OCD symptoms can appear after a strep infection, suggesting an autoimmune trigger.
Understanding these factors helps create a personalized and effective treatment plan.
How to Treat OCD: First-Line, Evidence-Based Approaches
Learning how to treat OCD effectively often involves a combination of psychotherapy and medication. This integrated strategy is highly successful, with combination therapy helping about 70% of people find significant relief. At Thrive Mental Health, our evidence-based care helps you break free from OCD’s grip.
With the right treatment team, you can learn practical skills to manage your symptoms and build a life that isn’t controlled by OCD.
Psychotherapy: The Gold Standard for OCD Treatment
Cognitive Behavioral Therapy (CBT) is the gold standard for treating OCD. The most powerful form of CBT for OCD is Exposure and Response Prevention (ERP), which is proven to be the most effective, first-line therapy.
ERP works by gradually exposing you to your fears while you resist the urge to perform compulsions. Your therapist will help you create a fear hierarchy, starting with mildly anxiety-provoking situations and working your way up. By resisting compulsions, you learn that your anxiety decreases on its own and your feared outcomes don’t happen. This process breaks the OCD cycle.
The results are compelling: 50% to 60% of people improve significantly with ERP. However, finding specialized, supportive care is crucial for success. For more on the basics, read A Beginners Guide to Cognitive Behavioral Therapy (CBT), and for a deeper look at this specific approach, explore our guide on Exposure and Response Prevention Therapy.
How to Treat OCD with Medication
Medication, especially when combined with therapy, plays a crucial role in how to treat OCD. Antidepressants can help control obsessions and compulsions.
Selective Serotonin Reuptake Inhibitors (SSRIs) are the first-line choice. They work by increasing serotonin levels in the brain and are often prescribed at much higher doses for OCD than for depression.
The FDA has approved several medications for OCD:
- Fluoxetine (Prozac): For adults and children 7+.
- Fluvoxamine (Luvox): For adults and children 8+.
- Sertraline (Zoloft): For adults and children 6+.
- Paroxetine (Paxil): For adults only.
When SSRIs aren’t effective, Clomipramine (Anafranil), a tricyclic antidepressant, is another powerful option for adults and children 10+.
Patience is key, as it can take 8 to 12 weeks to see improvement. Never stop medication abruptly; always consult your doctor to create a safe tapering plan. For help with your medication journey, explore our Medication Management Online services.
Finding the Right Therapist and Program
The success of your treatment depends on finding the right support. Look for an ERP specialist and ask about their experience treating OCD.
For severe symptoms, traditional weekly therapy may not be enough. Intensive Outpatient Programs (IOPs) and Partial Hospitalization Programs (PHPs) offer structured, comprehensive treatment for several hours a day, multiple days a week.
At Thrive Mental Health, we specialize in providing this expert-led care to adults across Florida. Our flexible virtual and in-person programs are customized to your needs, with evening options available to fit your schedule. While we also serve clients in several other states, our focus on Florida ensures you can receive high-quality, accessible treatment from home. Learn more about our Intensive Outpatient Program Mental Health.
Advanced and Complementary OCD Treatments
When first-line treatments like ERP and medication aren’t enough, it’s important to know you have other options. Approximately 40% of individuals with OCD don’t respond fully to initial approaches. This means it’s time to explore advanced and complementary strategies for how to treat OCD. A holistic approach that addresses your overall well-being can make a significant difference.
When Standard Treatments Aren’t Enough: How to Treat Severe OCD
For severe, treatment-resistant OCD, several advanced medical interventions show promise.
- Deep Brain Stimulation (DBS): An FDA-approved surgical procedure for adults who haven’t responded to other treatments. Surgeons implant electrodes in specific brain regions to regulate abnormal activity. Studies show about two-thirds of patients experience substantial relief.
- Transcranial Magnetic Stimulation (TMS): A less invasive, FDA-approved procedure that uses magnetic fields to stimulate nerve cells in the brain. TMS can reduce symptoms enough to help people engage more effectively with ERP therapy. You can find more information on these devices on the FDA website.
- Clinical Trials: These research studies test new treatments and can provide access to innovative therapies. Discussing clinical trials with your provider may open up new possibilities.
Lifestyle and Home Remedies to Support Recovery
Daily lifestyle choices can significantly support your professional treatment.
- Stress Management: Stress fuels OCD. Techniques like deep breathing and relaxation can help you maintain control. Our guide on CBT for Stress Management offers valuable strategies.
- Mindfulness and Meditation: Mindfulness teaches you to observe thoughts without judgment, reducing their power and making them less likely to trigger compulsions.
- Regular Exercise: Aerobic activity can reduce OCD symptom severity and improve mood. Find an activity you enjoy and can stick with.
- Nutritional Support: A balanced diet rich in whole foods and attention to gut health can support overall well-being. Deficiencies in nutrients like Vitamin D, B vitamins, and omega-3s are common, so discuss supplements with your provider.
- Quality Sleep: Sleep deprivation worsens anxiety and OCD symptoms. Prioritize consistent sleep hygiene for better emotional regulation.
The Power of Support Systems
Connecting with others who understand your struggle is incredibly healing.
- Support Groups: Sharing experiences with others reduces shame and provides practical coping strategies. The International OCD Foundation (IOCDF) provides resources to find OCD support groups.
- Family Education and Therapy: Involving family can transform your home into a supportive environment. Family therapy helps everyone learn how to respond helpfully instead of enabling compulsions.
- Peer Support: Online forums and communities offer ongoing encouragement. Engage mindfully to avoid reassurance-seeking.
If you’re in crisis, call/text 988 right now. You are not alone.
Frequently Asked Questions about OCD Treatment
When you’re exploring how to treat OCD, it’s natural to have questions. Here are answers to some of the most common ones.
Can OCD be cured completely?
OCD is considered a chronic condition, so there isn’t a “cure” in the traditional sense. However, with effective treatment like ERP and medication, symptoms can be managed so well that they no longer significantly impact your life. Many people reach a point where OCD becomes manageable background noise, allowing them to live full, meaningful lives.
What is the most effective therapy for OCD?
Exposure and Response Prevention (ERP) is the “gold standard” and most effective psychotherapy for OCD. As a specialized type of Cognitive Behavioral Therapy (CBT), it directly targets the cycle of obsessions and compulsions. ERP works by helping you face your fears while resisting the rituals, which breaks the cycle that strengthens OCD.
How long does OCD treatment take?
The timeline varies. For mild OCD, 8 to 20 sessions of ERP may be enough. For more severe cases, treatment often lasts a year or more to build lasting skills and allow the brain to form healthier patterns. Managing OCD is often an ongoing process, and the skills you learn in therapy become lifelong tools.
Can you treat OCD without medication?
Yes. Many people successfully treat OCD using only psychotherapy. ERP can be as effective as medication, especially for mild to moderate symptoms. For severe OCD, a combination of ERP and medication is often most effective, benefiting about 70% of individuals. The decision should be made with your healthcare team.
What should I do first if I think I have OCD?
Start with a professional evaluation. A licensed therapist or psychiatrist can confirm a diagnosis and outline your next steps. For residents of Florida, the expert team at Thrive Mental Health can provide this evaluation and create a personalized treatment plan, which typically includes ERP, medication, or both. If symptoms are severe, ask about higher levels of care like an IOP or PHP to accelerate progress.
Suggested FAQ schema (JSON-LD):
{
"@context": "https://schema.org",
"@type": "FAQPage",
"mainEntity": [
{
"@type": "Question",
"name": "Can OCD be cured completely?",
"acceptedAnswer": {
"@type": "Answer",
"text": "OCD is considered chronic, but with ERP and/or medication many people reduce symptoms so they no longer significantly impact daily life."
}
},
{
"@type": "Question",
"name": "What is the most effective therapy for OCD?",
"acceptedAnswer": {
"@type": "Answer",
"text": "Exposure and Response Prevention (ERP), a specialized form of CBT, is widely recognized as the gold-standard therapy for OCD."
}
},
{
"@type": "Question",
"name": "How long does OCD treatment take?",
"acceptedAnswer": {
"@type": "Answer",
"text": "Mild cases may respond in 8–20 ERP sessions; more severe OCD can take longer and often benefits from ongoing skills practice."
}
},
{
"@type": "Question",
"name": "Can you treat OCD without medication?",
"acceptedAnswer": {
"@type": "Answer",
"text": "Yes. Many people improve with ERP alone. For severe OCD, combining ERP with medication is often most effective."
}
},
{
"@type": "Question",
"name": "What should I do first if I think I have OCD?",
"acceptedAnswer": {
"@type": "Answer",
"text": "Start with a professional evaluation to confirm a diagnosis and plan next steps. For Florida residents, Thrive Mental Health can provide this service and create a plan involving ERP, medication, or both. Ask about IOP/PHP for severe symptoms."
}
}
]
}
Take Back Control: Your Path to Recovery Starts Now
You’ve already taken the most important step: seeking help for how to treat OCD. The journey from feeling trapped to reclaiming your life is possible.
Recovery is absolutely possible. Research shows that with the right evidence-based treatments, about 70% of people with OCD experience significant improvement. Whether through ERP therapy, medication, or intensive programs, relief is within reach. The key is accessing effective, customized treatment from professionals who specialize in proven approaches like ERP.
At Thrive Mental Health, our programs are built to make recovery accessible, with a special focus on serving Florida. Our virtual and hybrid Intensive Outpatient (IOP) and Partial Hospitalization (PHP) programs are available to adults across the state, including in Tampa Bay, St. Petersburg, Miami, and Orlando. With evening options, flexible scheduling, and partnerships with major insurance plans like Florida Blue, Cigna, and Optum, we remove barriers to getting help. While we also serve other states, our deep roots in Florida ensure you receive expert, convenient care.
You don’t have to figure this out alone. The evidence-based care you need is available now. Your story doesn’t end with OCD—it begins with the choice to seek help.
Ready for support? Thrive offers virtual and hybrid IOP/PHP with evening options. Verify your insurance in 2 minutes (no obligation) → https://gothrivemh.com/verify-insurance/ or call 561-203-6085. If you’re in crisis, call/text 988.


