The 5 Best Mental Health Centers for CBT & EMDR Trauma Compared

Find 5 Best CBT & EMDR Mental Health Trauma Centers
Your Path to Healing Starts Here: Understanding Trauma and Effective Treatment
Find me mental health centers that specialize in both CBT and EMDR for trauma is a search that reflects both urgency and hope—you’re ready for help, and you want the right kind.
Quick Answer: Top Characteristics to Look For
When searching for centers that offer both CBT and EMDR for trauma, prioritize these features:
- Dual Specialization: Staff trained and certified in both Cognitive Behavioral Therapy (CBT) and Eye Movement Desensitization and Reprocessing (EMDR)
- Trauma-Informed Care: Environments that prioritize safety, trust, and empowerment
- Flexible Programs: Options like Intensive Outpatient (IOP) or Partial Hospitalization (PHP) with evening or virtual sessions
- Qualified Therapists: Look for EMDRIA-certified clinicians and licensed professionals (LCSW, LMFT, PsyD)
- Evidence-Based Approach: Centers that integrate both modalities for comprehensive healing
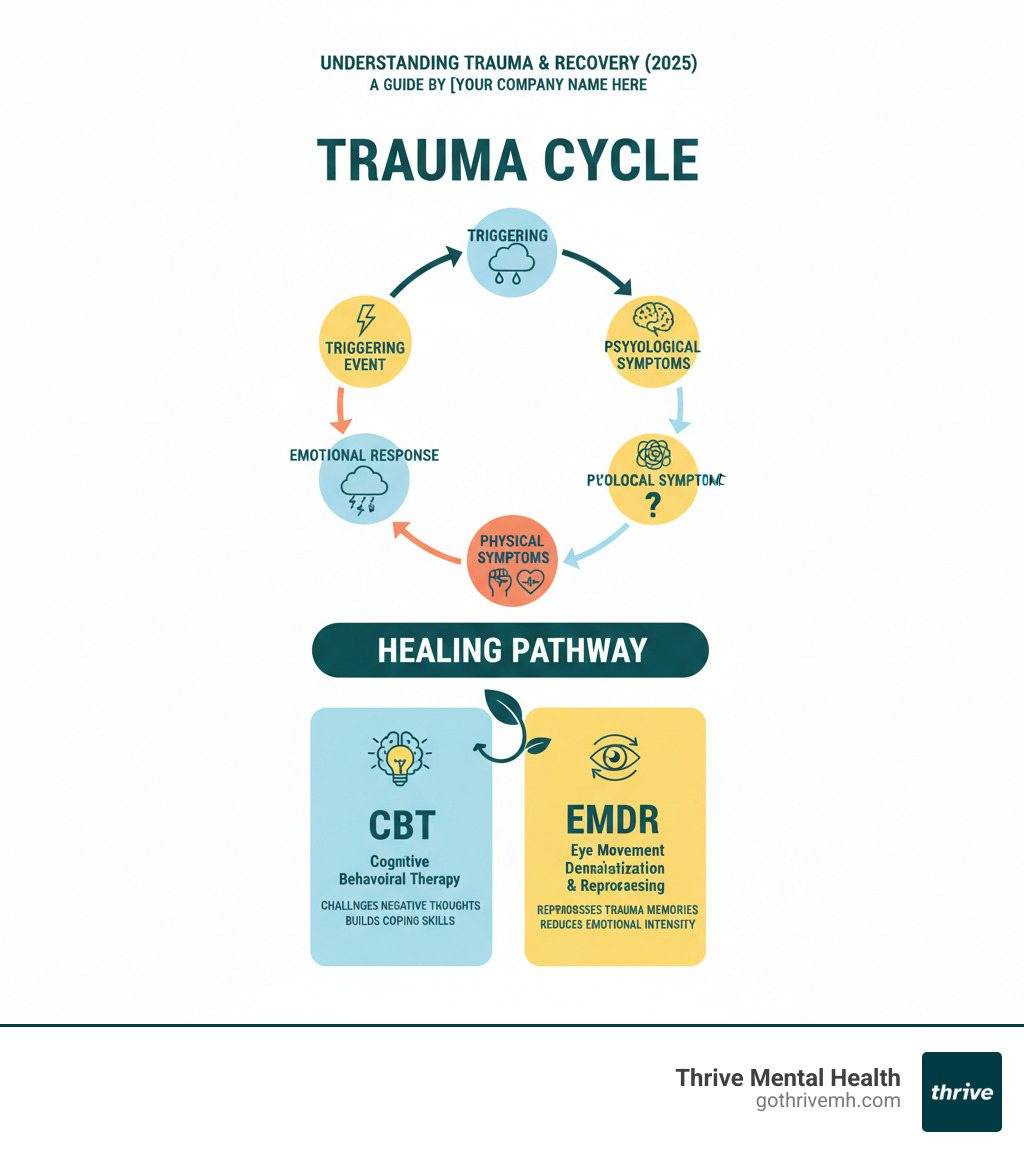
Trauma is an emotional response to a deeply distressing event—and it can leave lasting marks on your mental and physical health. It shows up as flashbacks, hypervigilance, anxiety, depression, and dissociation. Whether you’ve experienced a single traumatic incident or complex, long-term trauma, the impact on your nervous system is real and often overwhelming.
The good news? Trauma can heal. Research consistently shows that psychological therapies have a larger effect size than pharmacotherapy for PTSD, meaning therapy works—and it works well. Two of the most effective, evidence-based treatments for trauma are Cognitive Behavioral Therapy (CBT) and Eye Movement Desensitization and Reprocessing (EMDR). CBT helps you change negative thought patterns and build coping skills, while EMDR helps your brain reprocess traumatic memories so they no longer trigger intense emotional reactions.
Together, these therapies form a powerful combination. CBT stabilizes your day-to-day functioning while EMDR addresses the root of your trauma. Many leading mental health centers now offer both, creating a comprehensive path to recovery.
Finding a center that specializes in both CBT and EMDR can feel overwhelming, especially when you’re already struggling. This guide will walk you through what trauma is, how these therapies work, what to look for in a treatment center, and how to find the right fit for your needs.
I’m Anna Green, LMHC, LPC, Chief Clinical Officer and founder of Thrive Mental Health. I’ve spent years helping people find me mental health centers that specialize in both CBT and EMDR for trauma, and I’m trained in EMDR, psychodynamic therapy, and evidence-based modalities that support recovery from complex trauma. My mission is to make high-quality, accessible trauma care easier to start and stick with.
Trauma can manifest in various forms, from physical and sexual abuse to emotional neglect, natural disasters, or military combat. Each type leaves its unique imprint, often leading to long-term effects like disturbed sleep, relationship challenges, and self-esteem issues. Understanding these manifestations is the first step toward healing. For a deeper dive into this topic, refer to our Understanding Trauma: A Beginner’s Guide. The ultimate goal of trauma treatment is not to erase the past, but to help you process it, integrate it into your life story, and move forward with resilience and hope.
The Power Duo: Why CBT and EMDR Are Gold Standards for Trauma Recovery
When you’re searching for mental health centers that specialize in both CBT and EMDR for trauma, you’re looking for therapies that actually work—not just promising theories, but approaches backed by decades of research and real-world results.
Here’s what matters most: Cognitive Behavioral Therapy (CBT) and Eye Movement Desensitization and Reprocessing (EMDR) aren’t just popular buzzwords. They’re recognized by the World Health Organization, the American Psychological Association, and the Department of Veterans Affairs as first-line treatments for trauma and PTSD. These aren’t experimental approaches—they’re proven pathways to healing.
And here’s something that might surprise you: psychological therapies have a larger effect size than pharmacotherapy for PTSD. In plain English? Therapy works better than medication alone for treating trauma. That doesn’t mean medication has no place—it can be helpful for managing symptoms—but when it comes to actually healing from trauma, therapy leads the way.
CBT focuses on the connection between your thoughts, feelings, and behaviors. It helps you recognize when your mind is stuck in unhelpful patterns—like believing you’re always in danger or that you can’t trust anyone—and teaches you how to challenge those thoughts and respond differently. You’ll learn practical coping skills you can use every day, from managing panic attacks to handling triggers without falling apart.
EMDR takes a different approach. Instead of focusing primarily on changing your thoughts, it helps your brain reprocess traumatic memories so they no longer feel so overwhelming. Through bilateral stimulation—usually guided eye movements—your brain can finally digest experiences that got “stuck” during the trauma. The memory doesn’t disappear, but it loses its emotional punch. It becomes something that happened to you, not something that’s still happening to you.
When these two therapies work together, something powerful happens. CBT gives you the tools to manage your day-to-day symptoms and build a foundation of stability. EMDR goes deeper, addressing the core memories that keep fueling those symptoms. It’s like putting out both the visible flames and the underlying embers. For more on how this combination works, explore A Combination of CBT and EMDR Would Be Treatment For.
Key Differences: CBT vs. EMDR for Trauma
Understanding how CBT and EMDR differ helps you appreciate why having both available matters so much. They’re not competing approaches—they’re complementary tools that address different aspects of trauma.
| Feature | Cognitive Behavioral Therapy (CBT) | Eye Movement Desensitization and Reprocessing (EMDR) |
|---|---|---|
| Primary Focus | Identifying and changing negative thought patterns and behaviors | Reprocessing distressing traumatic memories and reducing their emotional impact |
| Technique | Talk therapy, cognitive restructuring, exposure, skill-building | Bilateral stimulation (eye movements, taps, sounds) while recalling traumatic memories |
| Session Structure | Structured, goal-oriented, often involves homework assignments | Eight-phase protocol, guided by therapist, less traditional “talk” about the trauma |
| Duration of Treatment | Can be short-term (12-20 sessions) or longer, depending on complexity | Often leads to quicker improvements for PTSD (8-12 sessions for single-incident trauma), but can be longer |
| Mechanism | Addresses cognitive distortions and maladaptive behaviors | Facilitates the brain’s natural information processing system, integrating traumatic memories |
CBT is a talk therapy that helps you understand the relationship between your thoughts and behaviors. If you’ve been avoiding driving since a car accident, CBT helps you identify the thought “I’m always unsafe” and test whether it’s actually true. You’ll practice relaxation techniques, learn to challenge catastrophic thinking, and gradually face situations you’ve been avoiding. It’s structured and practical—you’ll often have homework between sessions. To learn more about this approach, visit our Cognitive Behavioral Therapy (CBT) page.
EMDR works differently. You don’t have to talk through every detail of your trauma or complete homework assignments. Instead, you recall the traumatic memory while your therapist guides you through bilateral stimulation—typically following their finger with your eyes or feeling alternating taps on your hands. This process helps your brain reprocess the memory, integrating it into your regular memory networks where it no longer triggers intense reactions. Research shows that EMDR is highly effective for PTSD, often working faster than traditional talk therapy for single-incident trauma.
Some people prefer CBT because it feels more straightforward and logical. Others find EMDR more comfortable because they don’t have to verbally process every painful detail. Many people benefit from both. For a detailed comparison of different therapeutic approaches, see CBT vs. DBT vs. EMDR.
How CBT and EMDR Work Together for Comprehensive Healing
Think of trauma recovery like building a house. You need both a solid foundation and strong walls. CBT provides the foundation—the stability and coping skills you need to function day-to-day. EMDR builds the walls—addressing the core traumatic memories that keep destabilizing you.
Most integrated treatment approaches start with CBT during the stabilization phase. This is especially important if you’re dealing with complex trauma, ongoing life stressors, or severe symptoms that make you feel unsafe. You’ll learn grounding techniques for when you’re triggered, ways to manage overwhelming emotions, and skills for handling flashbacks or panic attacks. You might work on challenging negative beliefs like “I’m broken” or “It’s all my fault.” This foundation of skills makes it safer to do the deeper memory work that comes with EMDR.
Once you’ve built that foundation, EMDR can address the deeply embedded traumatic memories without overwhelming your system. Because you have coping skills from CBT, you can handle the emotional processing that EMDR involves. The bilateral stimulation helps your brain reprocess specific traumatic memories, reducing their emotional charge. As those memories lose their power, the cognitive distortions you worked on in CBT become easier to change—because they’re no longer being constantly reinforced by unprocessed trauma.
Here’s a real example: A veteran might use CBT to manage hypervigilance and sleep problems, learning relaxation techniques and challenging the belief that they’re always in danger. Once they’re stable, EMDR can help reprocess specific combat memories. As those memories are integrated, the hypervigilance naturally decreases because the brain is no longer stuck in survival mode. The CBT skills continue supporting them as they adjust to feeling safer in the world.
Research shows that CBT is effective in treating about 60% of trauma survivors with PTSD, with significant symptom reduction. When you add EMDR to the mix—especially for addressing specific traumatic memories—the outcomes improve even more. This phased, complementary approach ensures you’re not just managing symptoms but actually healing from the root causes of your trauma.
At Thrive Mental Health, we integrate both approaches into our Intensive Outpatient Program (IOP) and Partial Hospitalization Program (PHP), offering the comprehensive care that makes lasting recovery possible.
What to Look For in a Center Specializing in CBT & EMDR
When you’re ready to find me mental health centers that specialize in both CBT and EMDR for trauma, you’re not just looking for a list of treatment options. You’re searching for a place that truly understands what you’ve been through and has the expertise to walk beside you on your healing journey.

The foundation of effective trauma treatment is trauma-informed care—and this isn’t just a nice phrase on a website. It’s a fundamental commitment to recognizing how deeply trauma affects every aspect of your life and creating an environment where healing can actually happen. A truly trauma-informed center doesn’t just treat your symptoms; it understands the story behind them.
This starts with safety. You need to feel physically and emotionally secure from the moment you make your first phone call. The right center will prioritize creating spaces—whether virtual or in-person—where you can let your guard down without fear of judgment or harm. Trustworthiness follows naturally when staff members are transparent about treatment processes, honest about what to expect, and consistent in their support.
Empowerment is another crucial element. Your voice matters. Your choices matter. A quality center will partner with you to create individualized treatment plans that honor your unique experiences, strengths, and goals. You’re not a diagnosis to be managed; you’re a person with your own path to healing. This collaborative approach ensures that both CBT and EMDR are applied in ways that make sense for your specific situation.
The therapeutic relationship itself becomes a powerful tool for healing. When you find a center where therapists genuinely listen, validate your experiences, and respect your pace, the work goes deeper. This connection provides a safe container for the challenging work of processing trauma—whether that’s examining difficult thoughts in CBT or revisiting painful memories in EMDR.
Consider the program structure as well. Sometimes weekly therapy isn’t enough when trauma symptoms are overwhelming your daily life. An Intensive Outpatient Program (IOP) or Partial Hospitalization Program (PHP) offers more frequent, intensive support while still allowing you to maintain work or family commitments. These programs often integrate individual therapy, group sessions, and skill-building workshops, creating a comprehensive healing environment. At Thrive Mental Health, we offer flexible Intensive Outpatient Programs that combine both CBT and EMDR with the convenience of virtual or hybrid options, including evening sessions for busy professionals.
The right center will also accept peer support, recognizing that connecting with others who understand trauma can be profoundly healing. Group therapy isn’t about sharing every detail of your story—it’s about finding you’re not alone and learning from others’ resilience. Cultural sensitivity matters too. Your therapist should understand and respect your background, identity, and the unique context of your experiences.
Finding Qualified Therapists: Credentials That Matter
The credentials and experience of your therapist can make all the difference in your recovery. When you’re searching for centers that offer both CBT and EMDR, you want to see specific qualifications that demonstrate real expertise—not just general training.
For EMDR, the gold standard is an EMDRIA Certified Therapist. EMDRIA (EMDR International Association) requires extensive training beyond basic licensure—we’re talking about specialized coursework, supervised practice with actual clients, and ongoing consultation hours. This certification tells you the therapist has invested significant time mastering the eight-phase EMDR protocol and knows how to apply it safely and effectively. It’s not something you get from a weekend workshop.
For CBT, look for therapists with specialized training in trauma-focused CBT or significant documented experience applying CBT principles to trauma recovery. Many excellent CBT therapists are Licensed Clinical Social Workers (LCSW), Licensed Marriage and Family Therapists (LMFT), or hold a Doctorate in Psychology (PsyD). These professionals have foundational training in cognitive and behavioral techniques, but the key is finding someone who has adapted these skills specifically for trauma work.
Experience with your specific type of trauma matters too. Some therapists specialize in complex trauma from childhood, others in single-incident trauma like accidents or assault, and still others focus on military trauma or specific forms of abuse. Don’t hesitate to ask during your initial consultation: “How many clients with [your type of trauma] have you worked with?” and “What’s your approach to combining CBT and EMDR?”
Mental health professionals are held by ethical standards through the American Psychological Association (APA), which means they’re committed to providing care with integrity, maintaining confidentiality, and respecting your autonomy. These aren’t just rules—they’re the foundation of the trust you need to do this deep work.
How to find me mental health centers that specialize in both CBT and EMDR for trauma: The Importance of a Trauma-Informed Approach
A trauma-informed approach isn’t optional—it’s essential. This is the difference between a center that offers trauma treatments and one that truly gets trauma at every level of care, from the front desk staff to the therapists to the way your insurance verification is handled.
Here’s what this looks like in practice. The Substance Abuse and Mental Health Services Administration (SAMHSA) identifies six core principles of trauma-informed care, and the best centers weave these into everything they do.
Safety means more than locked doors and comfortable chairs. It’s about creating an emotional environment where you can be vulnerable without fear of being dismissed, judged, or overwhelmed. Trustworthiness and transparency show up in clear communication—you know what’s happening in your treatment, why, and what comes next. No surprises, no hidden agendas.
Peer support recognizes that healing happens in connection. You’re not just sitting across from a therapist; you might also be part of a group where others understand what it’s like to live with trauma’s aftermath. Collaboration and mutuality mean your therapist works with you, not on you. Your insights about what helps and what doesn’t are valued and incorporated into your care plan.
Empowerment, voice, and choice put you in the driver’s seat. You decide when you’re ready to process a memory in EMDR. You choose which CBT homework assignments fit your life. Your goals guide the treatment, not a one-size-fits-all protocol. Finally, attention to cultural, historical, and gender issues ensures your unique identity and background are honored, not overlooked.
When these principles are genuinely integrated, they create the conditions for both CBT and EMDR to work at their deepest levels. You can’t effectively challenge cognitive distortions in CBT if you don’t feel safe enough to be honest about your thoughts. You can’t reprocess traumatic memories in EMDR if you don’t trust your therapist to help you manage what comes up.
This trauma-informed foundation also helps prevent re-traumatization—when treatment inadvertently triggers past pain in ways that set you back rather than move you forward. The right center anticipates this risk and builds in safeguards, like teaching grounding techniques before starting EMDR or moving at a pace that respects your window of tolerance.
If you’re looking for this level of care, our guide on how to Discover Top EMDR Therapist: Find Relief Today offers additional insights into what makes a trauma therapist truly effective. The bottom line: when you find me mental health centers that specialize in both CBT and EMDR for trauma, you’re not just looking for techniques—you’re looking for a place that sees you as a whole person and treats you with the dignity and expertise your healing deserves.
How to Find Me Mental Health Centers That Specialize in Both CBT and EMDR for Trauma
You’ve decided you’re ready for help. You know you want both CBT and EMDR. Now comes the practical question: how do you actually find a center that offers both, and how do you know it’s the right fit?
The search doesn’t have to be overwhelming. With a few strategic approaches and the right questions, you can narrow down your options and find a place that truly understands trauma recovery. The key is being clear about what you need and not settling for less than specialized care.
Start by getting specific in your search. You’re not just looking for “therapy”—you’re looking for mental health centers that specialize in both CBT and EMDR for trauma. This specificity matters. When you contact centers, ask direct questions: Do you offer both modalities specifically for trauma? How do you integrate them? Are your therapists trained in both approaches, or will I see different providers for each?
Also consider your practical needs. Do you need evening sessions because of work? Would virtual therapy make it easier to show up consistently? Do you need a higher level of care like an Intensive Outpatient Program (IOP) or Partial Hospitalization Program (PHP) to really make progress? These programs offer more frequent, intensive therapy—often multiple sessions per week—which can accelerate healing, especially for complex trauma.
At Thrive Mental Health, we’ve designed our programs with these realities in mind. We offer both virtual and hybrid IOP and PHP programs with evening options, because we know that healing shouldn’t require you to quit your job or upend your life. Our therapists integrate both CBT and EMDR into individualized treatment plans, meeting you exactly where you are.
Using Online Directories and Professional Networks
The internet can be your best friend when searching for specialized trauma care—if you know where to look. Several trusted directories and professional networks can help you find qualified therapists and centers that offer both CBT and EMDR.
The EMDRIA “Find a Therapist” tool is an excellent starting point. The EMDR International Association maintains a searchable directory of EMDRIA Certified Therapists and Approved Consultants, ensuring you’re finding clinicians with verified training and expertise. This directory lets you filter by location and specialty, making it easier to find trauma-focused providers.
Psychology Today is another widely-used resource that allows you to search by location, insurance, and specific specialties like “trauma,” “EMDR,” and “CBT.” You can read detailed therapist profiles to get a sense of their approach, experience, and personality before reaching out. The site also includes treatment center listings, not just individual therapists.
The SAMHSA National Helpline (1-800-662-HELP or 4357) offers confidential, free support 24/7. Their trained specialists can connect you to local treatment resources and answer questions about what types of care might be right for you.
Don’t overlook targeted local searches either. Try search terms like “trauma therapy Indiana,” “EMDR California,” or “CBT and EMDR IOP” to find centers in your area or that serve your state. Many excellent programs, including virtual ones, may not appear in national directories but will show up in location-specific searches.
When you start reaching out, come prepared with questions. Ask about therapist credentials—are they EMDRIA-certified? Do they have specialized training in trauma-focused CBT? Inquire about their treatment philosophy and how they integrate both modalities. Ask about program structure: do they offer IOP or PHP? Are virtual sessions available? What does their approach to trauma-informed care look like in practice?
The consultation process itself tells you a lot. A good center will take time to understand your needs, answer your questions thoroughly, and help you feel comfortable before you commit. If you feel rushed or dismissed, that’s valuable information too.
Navigating Costs and Insurance Coverage
Let’s talk about money—because it matters, and pretending it doesn’t helps no one. Quality trauma treatment is an investment in your future, but understanding costs and insurance coverage can make it much more accessible than you might think.
Your first step should always be verifying your insurance benefits. Call your insurance provider directly and ask specific questions: What’s my coverage for outpatient mental health services? What about intensive outpatient programs or partial hospitalization? What’s my deductible, and have I met it this year? What’s my co-pay per session? Are there limits on the number of sessions covered?
Many quality trauma centers work with major insurance providers. At Thrive Mental Health, we work with Cigna, Optum, Aetna, United Healthcare, United Behavioral Health, UMR, Uprise Health, Triwest CCN, TRICARE, MOLINA, MHN, Health Net, and Florida Blue, among others. We understand that navigating insurance can be confusing, which is why we offer a quick insurance verification process—you can check your benefits in about two minutes with no obligation.
The distinction between “in-network” and “out-of-network” providers significantly impacts your costs. In-network centers have negotiated rates with your insurance, typically resulting in lower out-of-pocket expenses. Out-of-network providers may cost more upfront, though some will provide a “superbill” you can submit to your insurance for partial reimbursement.
Typical costs of therapy vary widely depending on the type and intensity of treatment. Individual therapy sessions generally range from $100 to $250+ per hour. IOP and PHP programs have higher overall costs due to their intensive nature—you’re receiving multiple therapy sessions per week, often including individual, group, and family therapy. However, these programs frequently have more comprehensive insurance coverage because they’re considered a higher level of care.
Don’t be afraid to have honest conversations about money with the centers you’re considering. Many are willing to discuss payment plans, sliding scale fees, or other options to make treatment accessible. The admissions team should be transparent about costs from the beginning—if they’re evasive or unclear, that’s a red flag.
Remember: the cost of not treating trauma—in terms of your health, relationships, career, and quality of life—is often far higher than the cost of effective treatment. You deserve care that works, and finding a way to afford it is part of the journey. For more information on how we approach comprehensive trauma care, visit our dedicated Trauma treatment page.
Your Healing Journey: What to Expect from Intake to Recovery
Starting on a healing journey from trauma takes real courage. If you’re wondering what happens after you reach out for help, knowing what to expect can ease some of that natural apprehension and help you feel more prepared for the transformative work ahead.

When you find me mental health centers that specialize in both CBT and EMDR for trauma, you’re looking for a place that can guide you through a structured yet deeply personal process. At Thrive Mental Health, we’ve designed our programs to support you from your very first call all the way through to long-term well-being. Your journey won’t be perfectly linear—healing rarely is—but it will be one filled with growth, increasing resilience, and compassionate guidance every step of the way.
The Treatment Process: From Your First Call to Your Last Session
Your healing journey typically begins the moment you reach out. That first call or message is often the hardest step, and we honor that. Our intake process is designed to be thorough yet welcoming, giving us a clear picture of your unique needs without feeling overwhelming.
During your initial comprehensive evaluation, we’ll sit down with you to understand your trauma history, current symptoms, daily challenges, and what you’re hoping to achieve through treatment. This isn’t just a checklist—it’s a conversation. We want to know what brings you here and what healing looks like to you. This assessment helps us determine the most appropriate level of care, whether that’s an Intensive Outpatient Program (IOP), Partial Hospitalization Program (PHP), or individual therapy sessions.
Based on what we learn together, we’ll collaborate with you to create a personalized treatment plan. This isn’t something we hand to you—it’s something we build with you, outlining your specific goals and how we’ll use both CBT and EMDR to help you reach them.
The early phase often focuses on stabilization and building coping skills, typically drawing heavily on CBT techniques. Before diving into deep trauma processing, it’s crucial to establish a foundation of safety and develop tools for managing overwhelming emotions. You’ll learn practical techniques for challenging negative thought patterns, grounding yourself when you feel triggered, and developing healthier behaviors. Think of it as building your emotional toolbox—mindfulness exercises, stress reduction strategies, and ways to regulate your nervous system when it goes into overdrive.
Once you’ve developed these essential coping skills and feel more stable, we move into the trauma processing phase, where EMDR often takes center stage. This is where the deeper healing happens. Using EMDR’s phased approach, we’ll work through specific distressing memories in a controlled, supportive environment. The bilateral stimulation helps your brain reprocess these memories, gradually reducing their emotional charge. You’re not forgetting what happened—you’re changing how your brain stores and responds to those memories.
Throughout your treatment, we’re constantly measuring progress and adapting your plan as needed. Healing isn’t one-size-fits-all, and your treatment shouldn’t be either. As you process your trauma and integrate new insights, we help you weave these changes into your daily life. The skills you learn in CBT and the processing you do through EMDR work together, creating lasting change.
As you near the end of your program, we focus heavily on discharge planning and setting you up for long-term success. We’ll identify potential triggers, develop strategies for managing setbacks, and ensure you have a solid plan for maintaining your progress. You’ll leave with practical tools and a clear path forward, not just a sense of having “finished therapy.”
Throughout this entire process, the therapeutic relationship is at the heart of everything we do. We strive to create a safe, non-judgmental space where you feel genuinely supported and empowered to engage in this deep, often challenging work. Your therapist is your partner in this journey, not just an expert telling you what to do.
Long-Term Benefits and Relapse Prevention
The benefits of undergoing treatment that combines CBT and EMDR for trauma reach far beyond just feeling better in the moment. The changes you experience are often profound and lasting.
Most people see a significant reduction in PTSD symptoms—fewer flashbacks, nightmares that gradually fade, less hypervigilance that kept you constantly on edge, and a decreased need to avoid places or situations that once felt unbearable. But the benefits go deeper than symptom relief.
You’ll likely notice improved emotional regulation—that overwhelming flood of feelings becomes more manageable. Instead of emotions controlling you, you develop the ability to experience them, understand them, and move through them. This leads to more stable moods and a greater sense of control over your inner world.
Many people find their relationships improve dramatically. As you heal, communication becomes easier, trust feels more possible, and you develop a greater capacity for genuine connection. The walls you built to protect yourself can start to come down in healthy ways.
Perhaps most importantly, you develop increased resilience—a deeper well of inner strength to draw from when life gets hard. You’re not just surviving anymore; you’re building the capacity to thrive. This often comes with a shift in how you see yourself, as negative self-beliefs are challenged and replaced with a stronger, more compassionate sense of self-worth.
Relapse prevention is a crucial part of long-term healing, and we take it seriously. This means continuing to practice the mindfulness techniques you learned, maintaining a strong support system, and making healthy lifestyle choices that support your mental health. Many people find ongoing benefit from support groups, where connecting with others who understand what you’ve been through provides continued healing and perspective.
Some individuals find that occasional “booster” therapy sessions help them maintain their progress, especially during particularly stressful times. There’s no shame in reaching back out—in fact, it’s a sign of strength and self-awareness.
Different populations benefit from this combined approach in unique ways. Young professionals struggling with the pressures of early career success often find that unresolved trauma is holding them back in ways they didn’t fully realize. Adults living with complex PTSD from childhood experiences—whether emotional neglect, abuse, or unstable home environments—often find that the structured skill-building of CBT combined with the deep memory processing of EMDR addresses their needs in ways other treatments haven’t. The comprehensive nature of these therapies allows us to tailor interventions to your specific situation, whatever that may be.
For more stories of recovery and what healing can look like, read our article on Healing from PTSD: Overcoming Traumatic Experiences. Your story of healing is waiting to be written, and we’re here to help you write it.
Frequently Asked Questions about CBT and EMDR for Trauma
Is EMDR or CBT better for PTSD?
Both are highly effective, first-line treatments for PTSD. Leading health organizations like the World Health Organization and the American Psychiatric Association recognize both EMDR therapy and CBT as valuable tools. The “better” choice depends on the individual’s specific trauma, symptoms, and personal preference. CBT focuses on changing negative thought patterns and behaviors, while EMDR focuses on reprocessing traumatic memories to reduce their emotional impact. Many centers combine both for comprehensive care, offering the best of both worlds.
How long does it take to heal from trauma with CBT and EMDR?
The healing timeline is highly individual and depends on factors like the nature and severity of the trauma, individual resilience, and the consistency of treatment. Some people see significant improvement in 8-12 sessions, especially with single-incident trauma. Complex or developmental trauma may require longer-term therapy, potentially spanning months or even years. Consistent participation in programs like an Intensive Outpatient Program (IOP) or Partial Hospitalization Program (PHP) can accelerate progress by providing more intensive support. Most people make significant progress within three to six months of consistent therapy.
Can EMDR and CBT be done virtually?
Yes, both CBT and EMDR have been adapted effectively for virtual therapy. Therapists use secure video platforms and specialized tools to guide clients through bilateral stimulation for EMDR (e.g., visual cues on screen, audio tones, or self-tapping exercises) and deliver CBT exercises. Virtual IOP and PHP programs make this specialized care accessible from anywhere, offering flexibility and convenience without compromising on the quality or effectiveness of treatment.
Take the Next Step Toward Healing
You’ve made it this far, and that alone says something powerful about your courage and readiness. Finding a mental health center that specializes in both CBT and EMDR for trauma is more than just a Google search—it’s a declaration that you’re ready to reclaim your life from the grip of past pain.
Throughout this guide, we’ve walked through what trauma is, how CBT and EMDR work individually and together, and what to look for in a treatment center. You now know that evidence-based therapies like CBT and EMDR aren’t just buzzwords—they’re proven pathways to healing, backed by research and real-world results. You understand that the right center will offer trauma-informed care, qualified therapists with credentials that matter, and a treatment approach that honors your unique story and needs.
Healing is not only possible—it’s within your reach. The journey might feel daunting, but you don’t have to walk it alone. Thrive Mental Health offers expert-led, evidence-based care custom to your unique needs, whether you’re dealing with single-incident trauma or complex, long-standing PTSD. We provide both virtual and in-person Intensive Outpatient Programs (IOP) and Partial Hospitalization Programs (PHP) with flexible scheduling, including evening options, so treatment fits into your life rather than disrupting it.
We serve adults and young professionals across multiple states, with locations in Florida (Tampa Bay, St. Petersburg, Miami, Orlando), South Carolina (Charleston, Columbia), Indiana (Indianapolis, Fort Wayne), Arizona (Phoenix, Tucson), and California (Sacramento, Los Angeles, San Diego). Our programs integrate both CBT for building coping skills and EMDR for deep memory processing, giving you comprehensive support every step of the way. We also work with major insurance providers, including Cigna, Optum, Aetna, United Healthcare, United Behavioral Health, UMR, Uprise Health, Triwest CCN, TRICARE, MOLINA, MHN, Health Net, and Florida Blue, making quality trauma care more accessible.
The path to healing starts with a single step—reaching out. That step might feel scary, but it’s also the most important one you’ll take. You deserve to live free from the weight of trauma, to experience relationships without fear, and to feel at home in your own mind and body again.
Ready for support? Thrive offers virtual and hybrid IOP/PHP with evening options. Verify your insurance in 2 minutes (no obligation) → Start benefits check or call 561-203-6085.
If you’re in crisis, call/text 988 right now. You are not alone.