Why OCD Isn’t Just Anxiety in Disguise

Is OCD an anxiety disorder: 3 Crucial Truths
More Than Just Worry
Is OCD an anxiety disorder? The short answer is no – and getting this wrong can derail your entire treatment plan.
Quick Answer:
- OCD is NOT an anxiety disorder (as of DSM-5, 2013)
- Previously classified as anxiety disorder in DSM-III and DSM-IV
- Now in its own category: “Obsessive-Compulsive and Related Disorders”
- Key difference: OCD has specific obsessions + compulsions, not just general worry
- Treatment differs: OCD needs specialized therapy (ERP), not standard anxiety treatment
If you’ve been told your intrusive thoughts and repetitive behaviors are “just anxiety,” you’re not alone in this confusion. For decades, mental health professionals grouped OCD with anxiety disorders because both involve intense worry and distress. But here’s what changed everything: researchers finded that OCD operates through a completely different brain circuit and responds to different treatments.
This isn’t just academic hairsplitting. Treating OCD like general anxiety can make symptoms worse. Standard talk therapy might validate obsessive thoughts when it should be challenging the compulsive responses. Anti-anxiety medications often fall short without the higher SSRI doses OCD typically requires.
The stakes are high. Misdiagnosis means months or years of ineffective treatment while OCD tightens its grip on your daily life. But when you understand OCD’s unique fingerprint – that obsession-compulsion cycle that sets it apart from broad anxiety – you can finally get the specialized care that actually works.
At Thrive Mental Health, our clinical leaders have seen countless clients finally break free from OCD once they received the right diagnosis and evidence-based treatment designed specifically for is OCD an anxiety disorder misconceptions. Our experience leading clinical strategy and specializing in complex presentations has shown us that understanding this distinction is often the turning point in recovery.
Essential is ocd an anxiety disorder terms:
The Big Reclassification: Why the DSM-5 Separated OCD from Anxiety Disorders
Here’s something that might surprise you: for decades, mental health professionals did consider OCD an anxiety disorder. If you’d asked this question in the 1980s or 1990s, the answer would have been a clear “yes.”
Both the DSM-III and DSM-IV – the diagnostic manuals that guided treatment for years – placed OCD squarely in the anxiety disorders category. And honestly, it made perfect sense at the time. Anyone who’s experienced OCD knows the crushing anxiety that comes with intrusive thoughts and the desperate need to perform rituals to make that anxiety stop.
But science has a funny way of evolving. As researchers dug deeper into how OCD actually works in the brain, they finded something fascinating: OCD operates through completely different neural pathways than traditional anxiety disorders. The obsession-compulsion cycle wasn’t just intense worry – it was something entirely unique.
This led to a groundbreaking decision in 2013. The American Psychiatric Association took OCD out of the anxiety disorders chapter and created a brand new category: “Obsessive-Compulsive and Related Disorders.” This wasn’t just shuffling papers around – it was based on solid evidence showing that OCD has distinct neurobiology, unique symptom patterns, and responds differently to treatment than conditions like generalized anxiety disorder or panic disorder.
You can read more about the APA’s explanation of the DSM-5 changes and explore the deeper meaning of OCD in light of this reclassification.
The Core Difference: Obsessions and Compulsions
What makes OCD so different from anxiety disorders? It all comes down to two specific features that work together like a broken record: obsessions and compulsions.
Obsessions are those unwanted thoughts, images, or urges that barge into your mind uninvited. They’re not just worries about real-life problems – they’re often bizarre, disturbing, or completely against your values. Think intrusive thoughts about contamination, harm coming to loved ones, or needing everything to be “just right.” These thoughts feel alien, like they’re coming from somewhere else entirely.
Then come the compulsions – the repetitive behaviors or mental acts you feel driven to perform to quiet those obsessions. Hand-washing until your skin is raw, checking the door lock fifteen times, arranging items until they feel perfect, or mentally repeating phrases to “undo” a bad thought. These rituals might provide temporary relief, but they’re often completely unconnected to the actual obsession or wildly excessive.
This obsession-compulsion cycle is OCD’s unique fingerprint. The obsession triggers intense anxiety, the compulsion temporarily reduces that anxiety, but then the obsession returns stronger than before. It’s exhausting, time-consuming, and completely different from the broad worries that characterize anxiety disorders.

A Look at the “OCD Spectrum”
Creating this new diagnostic category did something else important – it brought together a family of related conditions that share similar patterns of intrusive thoughts and repetitive behaviors.
Body Dysmorphic Disorder involves obsessing over perceived flaws in appearance and engaging in repetitive behaviors like mirror-checking or excessive grooming. Hoarding Disorder centers on the inability to discard possessions, leading to overwhelming accumulation. Trichotillomania is the recurrent urge to pull out one’s hair, while Excoriation Disorder involves compulsive skin-picking.
These conditions all share that same underlying pattern: intrusive thoughts or urges followed by repetitive behaviors that provide temporary relief but ultimately maintain the cycle. Grouping them together highlights that OCD isn’t just “bad anxiety” – it’s part of a distinct family of disorders that require specialized understanding and treatment approaches.
Spot the Difference: OCD’s Unique Footprint vs. Anxiety’s Broad Reach
Now that we know is OCD an anxiety disorder has a clear “no” answer, let’s dig into what makes these conditions so different. Think of it like comparing a laser pointer to a flashlight – both produce light, but one creates a precise, focused beam while the other casts a wide glow across everything.
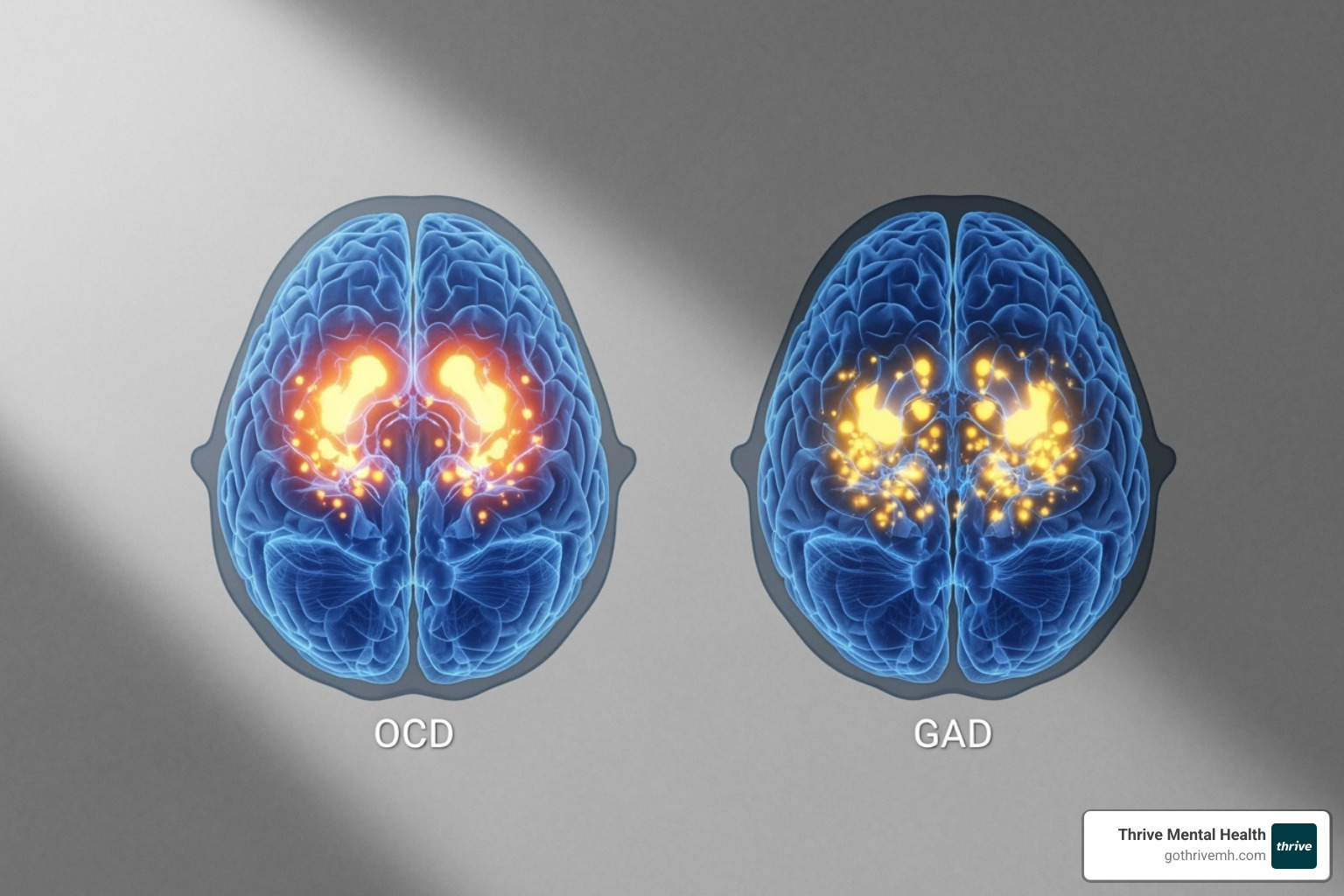
The brain imaging above tells a fascinating story. OCD activates specific neural circuits – primarily the orbitofrontal cortex, anterior cingulate cortex, and caudate nucleus. Anxiety disorders light up different areas and create more scattered patterns of activation. This isn’t just academic curiosity; it explains why these conditions need completely different treatment approaches.
The Nature of the Worry: Specific Intrusions vs. Generalized Fear
Here’s where things get really interesting. The thoughts that plague someone with OCD versus someone with generalized anxiety are like night and day.
OCD obsessions are ego-dystonic – a fancy term meaning they go against everything you believe about yourself. Picture a devoted mother who suddenly has intrusive thoughts about harming her baby. She’s horrified by these thoughts because they contradict her core identity as a loving parent. Or consider someone who’s deeply religious experiencing blasphemous thoughts that feel completely foreign and disturbing.
These obsessions often have a bizarre, almost “magical thinking” quality. You might feel convinced that if you don’t check the stove exactly seven times, your house will burn down – even though logically, you know this makes no sense.
Anxiety worries, on the other hand, are usually amplified versions of real concerns. Someone with generalized anxiety might lose sleep over job security, their child’s safety at school, or whether they said something embarrassing at last week’s meeting. These worries are excessive and persistent, but they’re rooted in actual life situations that most people think about occasionally.
The key difference? OCD thoughts feel alien and unwanted, while anxiety thoughts feel like “you” – just turned up to an unbearable volume.
Common OCD obsessions include contamination fears (what if I touched something dirty?), harm obsessions (what if I hurt someone?), sexual or religious intrusive thoughts that violate your values, symmetry and order needs (everything must be “just right”), and doubt obsessions (did I really lock the door?).
Anxiety worries typically center on job performance and career stability, family health and safety concerns, social judgment and embarrassment, financial security, and anticipating worst-case scenarios in everyday situations. You can learn more about these patterns in our guide to anxiety symptoms.
The Behavioral Response: Ritualistic Compulsions vs. Widespread Avoidance
The way people respond to these different types of distress creates another clear dividing line between OCD and anxiety disorders.
OCD compulsions are like following a strict recipe – there are specific steps, a particular order, and it must be done “just right” to provide relief. Someone with contamination obsessions might wash their hands for exactly three minutes, using a specific soap, in a precise pattern. If they get interrupted or it doesn’t feel right, they start over.
These compulsions can be physical actions (checking, washing, arranging) or mental rituals (counting, praying, repeating phrases silently). They’re directly tied to the obsession and performed with the desperate hope of reducing anxiety or preventing something terrible from happening.
Anxiety responses are more about escape and avoidance. If you have social anxiety, you might skip the office party entirely. If you’re worried about flying, you’ll drive everywhere instead. The goal is simply to get away from or avoid the anxiety-provoking situation altogether.
This distinction is crucial for treatment. Exposure and Response Prevention Therapy (ERP) specifically targets the compulsion cycle by helping people face their obsessions without performing their usual rituals. It’s like learning to sit with the discomfort until your brain realizes the feared catastrophe doesn’t actually happen.
What if I have both? Understanding Comorbidity
Here’s where answering “is OCD an anxiety disorder?” gets more complicated. About one-third of people with OCD also have a co-occurring anxiety disorder, according to research studies. It’s like having two different radio stations playing at the same time – both creating distress, but in distinctly different ways.
When OCD and anxiety disorders occur together, they can create a perfect storm. Someone with harm OCD might also have social anxiety, leading them to avoid social situations not just because of social fears, but also because they’re terrified of having intrusive thoughts around other people.
This is why accurate diagnosis matters so much. A dual diagnosis requires a treatment plan that addresses both the specific obsession-compulsion cycle of OCD and the broader worry patterns of anxiety disorders. You can’t treat one and ignore the other – they need to be tackled together with specialized approaches designed for each condition.
The good news? When mental health professionals understand these distinctions and create targeted treatment plans, recovery becomes much more achievable. It’s about using the right tools for each specific challenge rather than trying to fix everything with a one-size-fits-all approach.
Is OCD an Anxiety Disorder? The Critical Impact on Treatment
Getting the right diagnosis isn’t just about checking boxes on a form – it’s about getting your life back. When someone asks “is OCD an anxiety disorder?” the answer shapes everything that happens next in treatment. And here’s why this matters so much: the wrong approach can actually make things worse.
Why an Accurate Diagnosis is Non-Negotiable
Think about trying to use a screwdriver to hammer a nail. You might eventually get somewhere, but you’ll probably damage the wall and hurt your hand in the process. That’s exactly what happens when OCD gets treated like general anxiety.
I’ve seen this heartbreaking scenario play out countless times. Someone finally gets the courage to seek help for their intrusive thoughts and repetitive behaviors. They sit across from a well-meaning therapist who starts exploring the “deeper meaning” behind their obsessions. “Why do you think you have these thoughts about harming your child?” the therapist asks, genuinely trying to help.
But here’s the problem: this approach accidentally validates the obsession and reinforces the idea that the thought holds significant meaning. For someone with OCD, this is like pouring gasoline on a fire. The goal isn’t to understand why the thought exists – it’s to change how you respond to it.
Misdiagnosing OCD as general anxiety doesn’t just waste time and money. It steals hope. People spend months or years in therapy that inadvertently strengthens their symptoms, leaving them feeling like they’re broken or treatment-resistant. They’re not – they just need the right tools.
How is OCD an anxiety disorder treated differently?
OCD requires a completely different playbook than standard anxiety treatment, and the differences are crucial.
Exposure and Response Prevention (ERP) stands as the gold standard for OCD treatment. Think of it as systematic courage-building. You gradually face your feared obsessions while resisting the urge to perform your usual compulsions. It sounds terrifying at first, but here’s what happens: your brain learns that the anxiety naturally decreases without rituals, and those catastrophic outcomes you feared? They don’t actually happen.
This is radically different from anxiety treatment, which often focuses on relaxation techniques and avoiding triggers. With OCD, avoidance feeds the beast.
Medication approaches also differ significantly. While SSRIs help both conditions, OCD typically requires much higher doses than anxiety disorders. A dose that works perfectly for generalized anxiety might barely touch OCD symptoms. Plus, patience becomes essential – it can take 8 to 12 weeks to see full effectiveness, compared to the quicker response often seen in anxiety disorders.
Cognitive Behavioral Therapy (CBT) works beautifully for anxiety disorders, but for OCD, it absolutely must include that crucial “RP” component – Response Prevention. Without ERP, standard CBT might help you understand your thoughts better, but it won’t break the obsession-compulsion cycle that keeps OCD alive.
How is OCD an anxiety disorder diagnosed?
Getting an accurate diagnosis starts with finding a qualified mental health professional who understands the nuances between OCD and anxiety disorders. This isn’t something you can self-diagnose with an online quiz, though reflecting on your experiences can be a helpful starting point.
The diagnostic process involves detailed interviews about your symptoms, their duration, and how they impact your daily life. Mental health professionals use standardized tools and rating scales to measure the intensity of obsessions and compulsions, then compare your experiences against specific DSM-5 criteria.
For an OCD diagnosis, several key factors must be present. You need obsessions, compulsions, or both that consume significant time – typically more than an hour per day – or cause serious distress in your relationships, work, or other important areas of life. These symptoms can’t be better explained by substance use, medical conditions, or other mental health disorders.
The time factor often surprises people. Maybe your checking ritual only takes ten minutes, but you’re thinking about it, planning around it, and feeling distressed about it for hours each day. That all counts.
If you’re wondering whether your experiences align with OCD, exploring Do I Have OCD? can offer some initial insights, but remember – only a qualified professional can provide a definitive diagnosis. And that diagnosis? It’s your roadmap to the right treatment and, ultimately, your freedom from OCD’s grip.
Getting the Right Help: Specialized Care for OCD and Anxiety

Finding the right treatment when you’re struggling with OCD or anxiety can feel like searching for a needle in a haystack. The good news? Understanding that is OCD an anxiety disorder is a myth puts you ahead of the game. You’re no longer looking for just any therapist – you need someone who truly gets the difference between these conditions and knows how to treat each one effectively.
Finding Programs That Understand the Difference
When weekly therapy sessions aren’t enough, it’s time to consider stepping up your care. Intensive Outpatient Programs (IOP) and Partial Hospitalization Programs (PHP) offer the kind of structured, comprehensive support that can make all the difference for moderate to severe OCD or complex cases where anxiety joins the mix.
Think of these programs as your mental health boot camp – but in the best possible way. You’ll get multiple therapy sessions per week, often combining individual work with group support, all led by specialists who understand exactly why is OCD an anxiety disorder confusion has probably been holding back your progress.
These intensive programs shine particularly bright when you’re dealing with both OCD and anxiety disorders together. Instead of trying to juggle different therapists who might not coordinate their approaches, you get a unified treatment team that sees the whole picture.
The beauty of modern mental health care is that geography doesn’t have to limit your options. Thrive’s Virtual IOP for OCD brings expert-led treatment right to your living room. No commute, no waiting rooms, no excuses – just evidence-based care that fits your life.
Navigating Insurance for Mental Health Treatment
Let’s talk about the elephant in the room: cost. Mental health treatment can feel expensive, but here’s what many people don’t realize – your insurance likely covers more than you think. Major insurers like Cigna, Optum, and Florida Blue often provide robust coverage for IOP and PHP services, especially when these programs are medically necessary.
The key is understanding your specific benefits before you start treatment. This is particularly important for residents of Florida, where mental health parity laws ensure that insurance companies can’t discriminate against mental health treatment compared to medical care.
Don’t let insurance confusion keep you from getting help. Most quality treatment centers, including Thrive, have teams dedicated to helping you steer the benefits verification process. They’ll handle the paperwork jungle so you can focus on what matters most – your recovery.
A Note on Crisis: If you are in crisis or having thoughts of harming yourself, please call or text the 988 Suicide & Crisis Lifeline. You can connect with people who can support you. You are not alone.
Frequently Asked Questions about OCD and Anxiety
When people first learn that is OCD an anxiety disorder has a nuanced answer, they naturally have follow-up questions. These are the ones we hear most often from individuals seeking clarity about their symptoms and treatment options.
Is OCD a type of anxiety?
No, OCD is not classified as a type of anxiety disorder anymore. While it’s true that OCD causes intense anxiety – sometimes overwhelming anxiety – the mental health field moved it to its own category called “Obsessive-Compulsive and Related Disorders” in the DSM-5.
This reclassification happened because researchers finded that OCD’s core symptoms (those obsessions and compulsions we talked about earlier) operate through different brain mechanisms than traditional anxiety disorders like Generalized Anxiety Disorder or Panic Disorder. Think of it this way: both a sports car and a truck have engines, but they’re designed differently and need different maintenance approaches.
Can you have OCD without anxiety?
It’s highly unlikely to have OCD without experiencing anxiety. Here’s why: anxiety is essentially the emotional fuel that powers the entire OCD cycle. When an obsessive thought pops up – say, “Did I lock the front door?” – it triggers intense anxiety or distress. That uncomfortable feeling then drives the person to perform compulsions (like checking the lock multiple times) to get relief.
While anxiety is absolutely central to how OCD operates, the disorder itself is defined by that specific obsession-compulsion pattern, not just the anxiety alone. So you might say anxiety is a key player in OCD, but it’s not the whole story.
What is the main difference between OCD and Generalized Anxiety Disorder (GAD)?
The main difference comes down to the nature of the worry and how people respond to it.
With GAD, people experience persistent, excessive worry about a wide range of real-life concerns. They might constantly fret about job security, their children’s safety, financial stability, or health issues. These worries, while often exaggerated, are about plausible everyday problems.
OCD, on the other hand, involves very specific, intrusive obsessions that can feel bizarre or completely against the person’s values. Someone might have disturbing thoughts about harming a loved one (even though they would never want to do such a thing) or become convinced that touching a doorknob will lead to catastrophic illness. Then they perform specific, ritualistic compulsions – like washing hands in a particular sequence or checking something exactly seven times – to neutralize these obsessions.
The response patterns are different too. People with GAD tend to worry and avoid situations, while people with OCD get trapped in that cycle of obsession leading to compulsion, temporary relief, then back to obsession again.
Understanding these distinctions isn’t just academic – it’s the key to getting treatment that actually works for your specific situation.
Take Control with the Right Treatment Plan
Now that you understand is OCD an anxiety disorder has a definitive “no” as an answer, you’re already ahead of many people who struggle for years without proper treatment. This knowledge isn’t just academic – it’s your roadmap to recovery.
OCD’s unique neurological fingerprint means it responds to specific therapeutic approaches that are quite different from general anxiety treatment. Think of it this way: you wouldn’t use a screwdriver when you need a wrench. The wrong treatment tool can actually make OCD symptoms worse, while the right approach can be genuinely life-changing.
At Thrive Mental Health, we’ve built our programs around evidence-based therapies like Exposure and Response Prevention (ERP) – the gold standard treatment designed specifically to break the obsession-compulsion cycle that defines OCD. Our clinicians understand that when someone asks “is OCD an anxiety disorder,” they’re really asking whether their treatment plan is on the right track.
The truth is, you don’t have to fight this battle with the wrong tools anymore. Our virtual and hybrid IOP and PHP programs offer the intensive, specialized care that OCD demands, with the flexibility to fit your life. Whether you’re in Miami, Orlando, Tampa, or anywhere else in Florida, you can access expert-led treatment from clinicians who truly understand the difference between OCD and anxiety disorders.
Many of our clients tell us they wish they’d found specialized OCD treatment sooner. Don’t let another month pass wondering if your current approach is working. The right treatment exists, and it’s more accessible than you might think.
Ready for support? Thrive offers virtual and hybrid IOP/PHP with evening options. Verify your insurance in 2 minutes (no obligation) or call 561-203-6085. If you’re in crisis, call/text 988.