Detailed Reviews of Top 10 Treatment Centers for Autism & Depression

Top 10 Vital Autism & Depression Treatment for Adults 2025
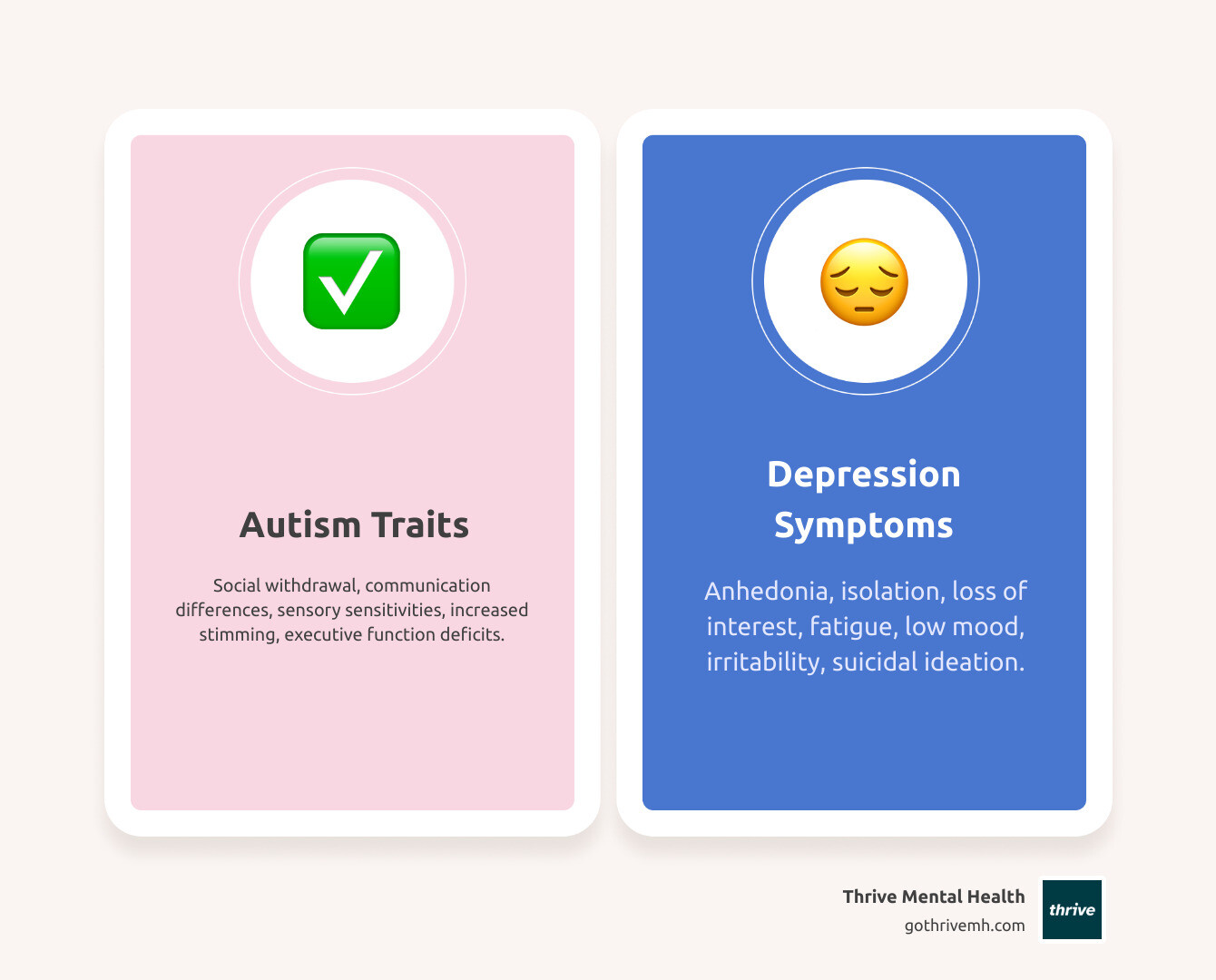
Why Adults with Autism and Depression Face a Hidden Mental Health Crisis
What are the best treatment centers for adults with co-occurring autism and depression? The answer depends on finding programs that offer neurodiversity-affirming care, dual-diagnosis expertise, sensory-friendly environments, and integrated support services. Here’s what to look for:
Key Features of Top Treatment Centers:
- Specialized Staff Training – Clinicians experienced in both adult autism and depression
- Neurodiversity-Affirming Approach – Strengths-based care that accommodates communication and sensory differences
- Flexible Therapeutic Modalities – Adapted CBT, DBT, and social skills training
- Sensory Accommodations – Quiet spaces, dim lighting, reduced noise
- Integrated Support Services – Vocational training, life skills coaching, family involvement
- Virtual and Hybrid Options – Evening scheduling for busy professionals
- Insurance Coverage – Accepts major plans including Cigna, Optum, and Florida Blue
Adults with autism are four times more likely to experience depression than the general population. Yet many struggle to access appropriate care.
Why? Because depression often looks different in autistic adults. Instead of expressing sadness verbally, they might withdraw further, increase repetitive behaviors, or lose interest in their special interests. Physical complaints like headaches or stomach pain can mask emotional distress.
Diagnostic overshadowing is a major problem. Clinicians may attribute symptoms like social withdrawal or flat affect to autism itself—missing the co-occurring depression entirely. This leaves adults without the targeted support they desperately need.
The consequences are serious. Autistic adults are nine times more likely to experience suicidal thoughts than non-autistic individuals. They use psychiatric emergency services nearly five times more often than adults without developmental disabilities. And despite seeking help at higher rates, 20-40% report unmet mental healthcare needs.
The barriers are real: lack of autism-trained providers, rigid treatment protocols that don’t accommodate sensory sensitivities, and complex healthcare systems that are hard to steer. Many autistic adults experience autistic burnout—a state of chronic exhaustion from masking their traits and managing sensory overload—which can mimic or worsen depression.
But here’s the truth: specialized care works. When treatment centers understand how autism and depression interact, when they adapt therapies to accommodate literal thinking and sensory needs, when they create environments that reduce overwhelm instead of adding to it—recovery is possible.
As Anna Green, LMHC, LPC, Chief Clinical Officer at Thrive Mental Health, I’ve spent my career developing neurodiversity-affirming programs for complex presentations, including what are the best treatment centers for adults with co-occurring autism and depression. I’ve seen how the right support transforms lives—and how the wrong approach can leave people feeling more isolated than ever.
The Unique Struggles of Dual Diagnosis
Content Warning: This section mentions suicidal ideation. If you or someone you know is in crisis, call or text 988 to reach the Suicide and Crisis Lifeline. You are not alone.
Living with both autism and depression presents a unique set of challenges that specialized treatment centers are best equipped to address. One significant hurdle is diagnostic overshadowing, where mental health symptoms are mistakenly attributed solely to autism, leading to missed or delayed depression diagnoses. This is often compounded by alexithymia, a common trait in autistic individuals that makes it difficult to identify and express emotions verbally. An autistic adult might experience deep sadness but report it as physical discomfort or irritability, making traditional diagnostic interviews less effective.
Sensory overload is another major factor. Autistic individuals often have heightened sensitivities to their environment, and the constant effort to manage these inputs can be exhausting. This chronic stress can contribute to depressive symptoms. Furthermore, social camouflaging (masking), the conscious or unconscious effort to appear neurotypical in social situations, is emotionally draining and can lead to increased stress, anxiety, and depression. The effort required to mask can deplete an individual’s energy, leaving them vulnerable to mental health crises.
Many autistic adults also face executive function deficits, which can impact their ability to plan, organize, and initiate tasks. When combined with depression, these challenges can become overwhelming, affecting daily functioning, self-care, and the ability to seek or maintain treatment. Tragically, autistic adults are significantly more likely to experience suicidal ideation compared to the general population, making specialized and sensitive care critically important. Finally, autistic burnout, a state of intense physical and mental fatigue resulting from prolonged masking and sensory overload, can closely mimic depression, requiring clinicians to distinguish between the two for accurate treatment.
What Are the Best Treatment Centers for Adults with Co-Occurring Autism and Depression?
Finding the best treatment centers for adults with co-occurring autism and depression isn’t about choosing the fanciest facility or the one with the longest waitlist. It’s about finding a place that truly gets how these conditions interact and creates space for you to heal without having to mask who you are.
At Thrive Mental Health, we’ve built our programs around neurodiversity-affirming care—a philosophy that respects autism as a natural variation of human neurology, not a problem to fix. We’re not here to make you “less autistic.” We’re here to help you manage depression while honoring your neurological differences. That means we adapt our approach to work with how your brain operates, not against it.
The centers that do this work well share a few essential qualities. They create individualized treatment plans that recognize you’re not a checklist of symptoms—you’re a whole person with unique strengths, challenges, communication styles, and sensory needs. They have dual diagnosis expertise, meaning their staff actually understand both autism and depression, how they overlap, and how to treat both without mistaking one for the other. This is huge, because diagnostic overshadowing is all too common in general mental health settings.
Effective treatment centers also provide integrated support services that go beyond the therapy room. Life doesn’t pause for treatment, and recovery isn’t just about managing symptoms—it’s about building a life that works for you. That might include vocational support, help with independent living skills, or guidance navigating relationships. At Thrive, we offer both Intensive Outpatient Program (IOP) and Partial Hospitalization Program (PHP) options, with flexible scheduling including evening sessions for professionals who can’t take time off work.
Perhaps most importantly, specialized centers create sensory-friendly environments where you don’t have to spend energy managing overwhelming stimuli on top of everything else. Adjustable lighting, quiet spaces, options to move or fidget, clear expectations about what to expect—these aren’t luxuries. They’re necessities that make treatment accessible rather than an additional source of stress.
We also offer Virtual Therapy options for adults across Indiana, California, and nationwide. Virtual care can be particularly helpful for autistic adults who find the sensory demands of in-person settings exhausting or who need the comfort of their own environment to engage fully in treatment. And we accept major insurance plans including Cigna, Optum, and Florida Blue—you can verify your insurance in just two minutes with no obligation.
The goal isn’t just symptom reduction. It’s creating a space where you feel understood, where your needs are anticipated rather than dismissed, and where you can focus on healing without constantly translating yourself for clinicians who don’t speak your language.

Key Features of an Effective Treatment Program
When you’re looking for a program that will actually help, certain features matter more than others. Staff trained in adult autism is non-negotiable. Not just clinicians who’ve read about autism, but professionals who understand how it presents in adults—the masking, the burnout, the way depression might show up as increased stimming or loss of interest in special interests rather than tears.
Flexible communication options make the difference between being heard and being misunderstood. Some days you might be able to talk through things. Other days, writing or using visual supports might work better. The best programs meet you where you are, offering processing time, written communication options, and concrete language instead of abstract therapy-speak.
A strengths-based approach shifts the focus from what’s “wrong” with you to what’s working and how to build on it. Your intense interests aren’t symptoms to eliminate—they’re potential sources of joy and connection. Your pattern recognition and attention to detail aren’t deficits—they’re strengths that can support your recovery.
Family and caregiver involvement matters too, when that’s part of your support system. Education helps the people around you understand what you’re experiencing and how to help. It reduces those frustrating moments when well-meaning loved ones say exactly the wrong thing because they don’t understand how autism and depression interact.
Vocational and life skills support recognizes that mental health doesn’t exist in a vacuum. Maybe you’re struggling at work because executive function challenges make organization difficult. Maybe you’re isolated because social situations feel impossible. Programs that address these practical realities—employment support, independent living skills, financial literacy, relationship education—give you tools for building a life, not just managing symptoms.
Finally, crisis planning designed specifically for autistic adults can be lifesaving. Standard crisis protocols often make things worse for autistic people—too much sensory input, too many people talking at once, expectations to make eye contact or explain feelings you can’t name. Specialized programs create crisis plans that account for communication differences, sensory needs, and the specific triggers that might lead to a mental health emergency.
Specialized vs. General Mental Health Services
Here’s the truth: general mental health services work for some people, but they often fail autistic adults. Not because the clinicians are bad at their jobs, but because they’re applying a one-size-fits-all approach to people who don’t fit that size.
| Feature | Specialized Centers | General Clinics |
|---|---|---|
| Staff Training | Autism & depression expertise | General mental health |
| Therapeutic Approach | Neurodiversity-affirming, adapted therapies | Standard protocols |
| Environment | Sensory-friendly, flexible | Standard settings |
| Communication Methods | AAC, visual supports, literal language | Verbal focus |
| Support Services | Life skills, vocational, family | Limited or none |
In a general clinic, you might get a therapist who means well but attributes your social withdrawal to autism when it’s actually depression. They might use abstract metaphors that leave you confused. They might schedule you in a bright, noisy office with fluorescent lights humming overhead while expecting you to open up about your deepest struggles.
Specialized centers like Thrive take a different approach. Our staff receive specific training in adult autism—not just the childhood presentation most people learn about, but how it shows up in adults who’ve spent years masking and compensating. We use neurodiversity-affirming, adapted therapies like modified CBT and DBT that work with autistic thinking patterns rather than trying to force neurotypical frameworks.
Our environments are designed to reduce sensory overload, not add to it. We understand that communication can take many forms—augmentative and alternative communication (AAC), visual schedules, written exchanges, or simply giving you time to process before expecting a response. We speak literally and clearly, avoiding idioms and ambiguous language that can cause confusion.
And we provide comprehensive support services that recognize you need more than weekly talk therapy. That might mean connecting you with vocational rehabilitation, teaching executive function strategies, or involving family members who want to help but don’t know how. For California and Indiana residents, we accept insurance including Cigna, Optum, and Florida Blue, making specialized care more accessible.
The difference isn’t subtle. It’s the difference between feeling like you’re constantly translating yourself and feeling understood. Between environments that exhaust you and spaces where you can focus on healing. Between generic treatment protocols and care designed for how your brain actually works.
If you’re ready to explore whether Thrive is the right fit, you can verify your insurance in 2 minutes with no obligation, or call 561-203-6085 to speak with someone who gets it.
In-Depth Reviews: Top 10 Treatment Centers for Autism & Depression in 2025
Finding what are the best treatment centers for adults with co-occurring autism and depression shouldn’t feel like an impossible task. The truth is, there aren’t ten truly specialized centers that meet all the criteria we’ve discussed—and we’re not going to pretend there are.
What matters more than a numbered list is knowing what to look for so you can evaluate any program you’re considering. We’ll start with what we know works—our own program at Thrive—and then give you the framework to assess other options with confidence.
Each quality program should clearly communicate:
- Location and accessibility (including virtual options)
- Insurance accepted (Cigna, Optum, Florida Blue, etc.)
- Program types (IOP, PHP, Virtual Therapy)
- Sensory accommodations and how they’re implemented
- Staff training in adult autism and depression
- Unique features that make care more accessible

Thrive Mental Health
At Thrive Mental Health, we’ve built our programs specifically around the needs of adults with complex presentations—including those navigating both autism and depression. We offer virtual and hybrid Intensive Outpatient Programs (IOP) and Partial Hospitalization Programs (PHP) that actually work with your life, not against it.
Our evening and flexible scheduling options recognize that many autistic adults are managing jobs, relationships, and other responsibilities. You shouldn’t have to choose between getting help and maintaining your daily life. We’ve designed our programs to be sensory-friendly from the ground up—not as an afterthought. That means quiet breakout spaces, adjustable lighting options, and the ability to turn off your camera during group sessions if eye contact or seeing yourself on screen feels overwhelming.
Our clinical team practices neurodiversity-affirming care, which means we understand that autism isn’t something to fix. We’re here to help you manage depression and build skills that work with your neurology, not against it. We accept a wide range of insurance providers, including Cigna, Optum, Florida Blue, and many others, and we serve clients nationwide—with particular strength in Indiana and California.
Whether you choose our Partial Hospitalization Program (PHP) for more intensive support or our Intensive Outpatient Program (IOP) for structured care that fits around work, we meet you where you are. Our Virtual Therapy options eliminate the sensory overwhelm of commuting and unfamiliar environments. You can verify your insurance in about two minutes, with no obligation—we know that reducing barriers matters.
Other Top Centers to Consider
When you’re evaluating other centers, you need to ask the right questions. Not every program that treats depression or mentions autism will truly understand what are the best treatment centers for adults with co-occurring autism and depression actually provide.
Start by asking about dual-diagnosis expertise for adults specifically. Some centers work primarily with children or adolescents, and the approaches that work for younger populations don’t always translate. You want a team that understands how depression presents differently in autistic adults—how it might show up as increased stimming, loss of interest in special interests, or autistic burnout rather than traditional “sadness.”
Sensory accommodations should be concrete, not vague promises. Ask exactly what they offer: Do they have quiet spaces? Can you control lighting in therapy rooms? Are there options for breaks? Can you use fidget tools? If they can’t give you specific answers, that’s a red flag.
Flexible scheduling, including evenings, makes treatment actually accessible. Many autistic adults are employed or have other commitments that make traditional 9-to-5 programs impossible. Virtual and hybrid care options are especially important if you live in states like Indiana or California where specialized in-person options might be hours away.
The staff’s training matters more than almost anything else. Ask: “How do you adapt your therapeutic approaches for autistic adults with alexithymia?” or “What training has your team received in neurodiversity-affirming care?” The quality of their answer will tell you whether they truly understand the population they’re serving.
Insurance coverage can make or break your ability to access care. Verify they accept your specific plan—whether that’s Cigna, Optum, Florida Blue, or another provider. Don’t assume coverage is the same across all programs. Some centers that work with one plan won’t work with another.
Look for integrated life skills and vocational support beyond just traditional therapy. Depression doesn’t exist in a vacuum—it affects your ability to work, manage daily tasks, and maintain relationships. Quality programs recognize this and offer practical support in these areas.
Family and caregiver involvement should be optional but available. For some adults, family support is crucial; for others, it’s not appropriate. The program should be flexible enough to accommodate either situation and offer education to families who want to better understand and support their loved one.
Finally, ask about crisis planning and aftercare. What happens if you’re in crisis during treatment? What support exists after you complete the program? A comprehensive approach doesn’t just end when your last session does.
Here’s a tip that can save you time: When you’re calling programs, start with this question: “How many adults with co-occurring autism and depression have you treated in the past year?” If they can’t give you a clear answer or the number is very low, keep looking. Experience matters, especially with a dual diagnosis this complex.
You deserve care that sees all of you—not just your depression, not just your autism, but the whole person navigating both. That’s what quality treatment centers provide, and that’s the standard you should hold every program to.
Effective Therapeutic Approaches for a Dual Diagnosis
Treating co-occurring autism and depression isn’t about applying a one-size-fits-all approach. It requires understanding how these conditions interact in each person’s life. Adapting therapies for neurodivergence means meeting people where they are—respecting how autistic brains process information, experience emotions, and communicate.
The reality is that autism and depression influence each other in complex ways. Addressing the interplay of symptoms is crucial because what looks like withdrawal from depression might actually be sensory overload triggering a shutdown. Executive function challenges can make it harder to implement coping strategies, which can deepen feelings of hopelessness. Our clinicians understand these connections and tailor treatment accordingly.
Perhaps most importantly, effective treatment depends on building a therapeutic alliance based on trust and understanding. For autistic adults, this means working with therapists who use concrete language, respect the need for processing time, and understand that eye contact isn’t necessary for engagement. We create predictable, non-judgmental spaces where individuals can be themselves without the exhausting effort of masking.

What Specialized Treatment Approaches Work for Adults with Both Autism and Depression?
When it comes to what are the best treatment centers for adults with co-occurring autism and depression, the answer often lies in how they adapt evidence-based therapies. Several approaches have shown real promise when modified thoughtfully for autistic adults.
Adapted Cognitive Behavioral Therapy (CBT) forms the foundation of many successful treatment plans. Traditional CBT focuses on identifying and challenging negative thought patterns, but for autistic adults, this needs adjustment. We use more visual aids and concrete examples, breaking down abstract concepts into manageable steps. This is especially helpful for individuals with alexithymia who may struggle to connect thoughts with feelings. Instead of asking “How does that make you feel?” we might say “When that happened, did you notice changes in your body? Did your heart beat faster? Did you want to leave?”
Dialectical Behavior Therapy (DBT) offers powerful skills for emotion regulation, distress tolerance, interpersonal effectiveness, and mindfulness. These are particularly valuable when sensory overload triggers intense emotions or when social interactions feel overwhelming. The structured, skill-based nature of DBT often resonates with autistic individuals who appreciate clear frameworks and concrete techniques.
Acceptance and Commitment Therapy (ACT) helps people accept difficult thoughts and feelings rather than fighting them, while committing to actions aligned with their values. For autistic adults who experience chronic stress from navigating a neurotypical world, ACT can reduce the exhausting effort of trying to “fix” themselves and instead focus on meaningful living.
Social skills training addresses a common contributor to depression: isolation and misunderstanding. While it doesn’t directly treat depression, improving practical strategies for navigating social situations can reduce loneliness and build connections. We focus on authentic communication styles that work for each person, not forcing neurotypical social norms.
Mindfulness-based interventions teach individuals to observe thoughts and feelings without judgment. When adapted to accommodate sensory sensitivities—perhaps through body-based awareness rather than focusing on breath, or using special interests as anchors—mindfulness becomes a powerful tool for managing both anxiety and depression.
How Treatment Centers Accommodate Autistic Needs
Creating a truly supportive environment goes far beyond good intentions. Specialized centers make concrete accommodations that reduce barriers and promote healing.
Sensory accommodations are non-negotiable. This means offering dim lighting and reduced noise in therapy spaces, providing quiet rooms for breaks, and having sensory tools available—weighted blankets, fidget items, noise-canceling headphones. We recognize that sensory overload isn’t a minor inconvenience; it can completely derail treatment progress and worsen depressive symptoms.
Flexible scheduling acknowledges that autistic adults benefit from routine but may also need accommodations for processing time, fatigue, or sensory needs. Evening options help those balancing work commitments. Virtual sessions eliminate the stress of travel and unfamiliar environments. Some people need shorter, more frequent sessions rather than the standard 50-minute hour.
For individuals who find verbal communication challenging, we use Augmentative and Alternative Communication (AAC) methods. This might include visual schedules, picture cards, text-based communication, or written responses. The AAC approach ensures everyone can express themselves fully and participate meaningfully in their treatment.
Our therapists are trained in using concrete and literal language. We avoid metaphors, sarcasm, and abstract concepts that can create confusion. When we say “Let’s explore that,” we explain exactly what we mean. This direct communication builds trust and reduces the anxiety of trying to decode hidden meanings.
Finally, we believe in incorporating special interests as therapeutic tools. Whether it’s trains, astronomy, art history, or coding, these interests can be bridges to engagement, sources of comfort during difficult moments, and pathways to practicing new skills. Your passion isn’t a distraction from therapy—it’s an asset that makes treatment more effective.
At Thrive Mental Health, we’ve designed our Intensive Outpatient Program (IOP) and Partial Hospitalization Program (PHP) with these accommodations built in from the start. Because effective treatment isn’t about changing who you are—it’s about supporting you to thrive as yourself.
Building a Comprehensive, Long-Term Support System
Effective treatment for co-occurring autism and depression isn’t a one-and-done deal. It’s about creating a holistic care model that supports every part of your life—not just what happens in a therapy session. Think of it as building a safety net with many strands: medication management when appropriate, life skills development to help you steer daily challenges, family education so your loved ones understand how to support you, and peer support groups where you can connect with others who truly get it.
Recovery isn’t linear, and lasting well-being requires addressing the practical realities of life alongside clinical treatment. When you’re managing both autism and depression, having support that extends into your workplace, your home, and your community makes all the difference. The goal is to help you not just survive, but genuinely thrive.

The Role of Medication in a Dual-Diagnosis Treatment Plan
Medication isn’t for everyone, but for many adults with co-occurring autism and depression, it can be a helpful tool in recovery. Here’s what you need to know: medication is used to target depressive symptoms and related conditions like anxiety—not autism itself. Autism is a neurological difference, not an illness, so the focus is on treating the depression that’s causing distress.
The most commonly prescribed medications are SSRIs (Selective Serotonin Reuptake Inhibitors) and SNRIs (Serotonin-Norepinephrine Reuptake Inhibitors). These antidepressants work by regulating neurotransmitters in the brain that affect mood. However, autistic individuals often respond differently to medication than neurotypical people. You might be more sensitive to side effects, or you might need a lower dose to achieve the same benefit.
That’s why careful medication management is absolutely essential. You need an autism-informed psychiatrist who understands these differences and won’t just prescribe the standard dose and send you on your way. The right provider will monitor side effects closely, adjust dosages gradually, and work collaboratively with you to find what works best for your unique brain and body. It’s a partnership, not a prescription pad.
Crucial Support Services for Lasting Recovery
Clinical therapy and medication are important pieces of the puzzle, but they’re not the whole picture. What are the best treatment centers for adults with co-occurring autism and depression? The best ones offer comprehensive support services that help you build a life worth living. Here’s what that looks like in practice:
Vocational training helps you identify your strengths and find meaningful work that accommodates your needs. Many autistic adults have incredible talents that employers value—attention to detail, pattern recognition, deep focus—but traditional job-seeking processes can be overwhelming. Supported employment programs bridge that gap, reducing financial stress and boosting self-esteem.
Independent living skills coaching covers the practical stuff that can make or break your day: budgeting, meal prep, household management, using public transportation. When you’re dealing with executive function challenges and depression, these tasks can feel impossible. Having someone teach you strategies and help you build routines makes a huge difference.
Financial literacy is another game-changer. Understanding how to manage money, pay bills on time, and build savings reduces anxiety and creates a sense of control. Money stress can worsen depression, so this kind of practical support is genuinely therapeutic.
Relationship and sexuality education matters too. Autistic adults want connection, intimacy, and love just like anyone else. Education on healthy relationships, boundaries, and consent improves social well-being and reduces isolation. You deserve to have fulfilling relationships, and learning these skills helps make that possible.
Finally, self-advocacy skills empower you to communicate your needs, set boundaries, and speak up for yourself in healthcare settings, at work, and in social situations. Being able to advocate for yourself is one of the most important long-term skills you can develop. It’s the difference between feeling helpless and feeling empowered.
At Thrive, our intensive outpatient programs integrate these essential life skills into treatment. We believe that recovery isn’t just about symptom reduction—it’s about building a life that feels meaningful, connected, and authentically yours.
How to Find and Access the Right Care for You
Searching for mental health support when you’re dealing with both autism and depression can feel overwhelming. The healthcare system is complex, and finding providers who truly understand dual diagnosis is harder than it should be. But you don’t have to do this alone. At Thrive Mental Health, we’ve helped countless adults find their way to the care they deserve, and we’re here to guide you through the process.
The first thing to know is that what are the best treatment centers for adults with co-occurring autism and depression? isn’t just about finding any provider—it’s about finding the right one. That means looking for programs with specialized training, sensory-friendly environments, and a genuine understanding of how autism and depression interact. It means finding a place where you won’t have to mask or translate yourself to be understood.
Understanding your insurance coverage is a crucial early step. Most major plans—including Cigna, Optum, and Florida Blue—cover dual-diagnosis treatment, including IOP and PHP programs. But coverage details vary widely, so it’s worth taking the time to verify your specific benefits. We’ve made this easier with our quick online verification tool, and our team is always available to help you understand your options.

How to Find Treatment Centers for Co-Occurring Autism and Depression
Start by consulting specialists who understand adult autism. A developmental psychologist, neurologist, or autism-informed therapist can point you toward programs that actually have the expertise you need. General mental health directories often list centers that claim to treat autism, but many lack specific training in dual diagnosis for adults.
When you contact potential centers, vet them thoroughly for dual-diagnosis experience. Don’t be shy about asking direct questions. How many autistic adults have they treated? What specific adaptations do they make to therapy? How do they handle sensory sensitivities during sessions? A good program will answer these questions confidently and specifically, not with vague reassurances.
Your questions during intake matter enormously. Ask about staff training in adult autism, not just child-focused approaches. Inquire about their experience with alexithymia and communication differences. Find out what sensory accommodations they offer—not just whether they have them, but what specifically they provide. Ask whether they integrate vocational support, life skills coaching, and family involvement into treatment. These details reveal whether a center truly understands what you’re facing.
Verifying your insurance benefits shouldn’t be an afterthought. Call your provider directly or use our online tool to verify your insurance. Ask specifically about coverage for Intensive Outpatient Programs (IOP), Partial Hospitalization Programs (PHP), and virtual therapy. Understanding your financial responsibility upfront removes one major source of stress from an already difficult process.
For many adults, virtual options dramatically improve accessibility. If you experience sensory overload in unfamiliar environments, if transportation is challenging, or if you simply process better in your own space, virtual and hybrid programs can be life-changing. At Thrive Mental Health, we’ve designed our virtual and hybrid IOP and PHP programs to deliver the same expert care as in-person treatment, with added flexibility for evening sessions. This is especially valuable for working professionals who can’t take time off during business hours.
We’re proud to serve clients nationwide, with particular expertise in meeting the needs of Indiana and California residents. We understand the insurance landscapes in these states and work with major providers to ensure accessible, affordable care.
Long-Term Recovery Prospects and Refinding Hope
Here’s what I want you to know: recovery is real. With specialized, neurodiversity-affirming care, adults with co-occurring autism and depression can experience profound, lasting improvements in their lives.
You can expect to see reduced depressive symptoms—not just temporarily, but through learning strategies that work with your autistic brain, not against it. Custom therapies like adapted CBT and DBT, combined with appropriate medication management when needed, lead to meaningful reductions in both the severity and frequency of depressive episodes.
Perhaps more importantly, you’ll gain improved self-understanding and acceptance. Many adults we work with describe a sense of relief when they finally understand how autism and depression interact in their own experience. This insight reduces self-criticism and opens the door to genuine self-compassion. You’re not broken. You’re not doing life wrong. You’re neurodivergent navigating a world not designed for you, and that requires different strategies—not more willpower.
Your quality of life improves when both conditions are addressed together. You’ll find it easier to engage in activities that matter to you, whether that’s work, creative pursuits, or simply enjoying quiet time without the weight of unmanaged depression. Daily tasks become more manageable when you have support for executive function challenges and coping strategies for sensory overload.
Building meaningful relationships becomes possible when you’re not constantly depleted by masking or overwhelmed by untreated depression. With improved emotional regulation and reduced anxiety, you can form connections that feel authentic and sustainable. You’ll learn to communicate your needs more effectively and recognize relationships that truly support your well-being.
And yes, you can work toward achieving personal and professional goals that may have felt out of reach. With comprehensive support—including vocational training, life skills development, and ongoing therapeutic care—you’re better equipped to pursue what you actually want from life, not just what you think you should want.
Recovery isn’t about becoming neurotypical. It’s about building a life where you can thrive as your authentic self, with the support and strategies you need to manage depression effectively. That’s the hope we offer, and it’s a hope grounded in evidence and experience.
Ready to take the first step? Explore our flexible virtual PHP and IOP programs designed specifically for adults with co-occurring autism and depression. We offer evening options, sensory-friendly care, and expert support from wherever you feel most comfortable.
Frequently Asked Questions about Autism and Depression Treatment
You have questions—and that’s completely natural. Finding the right care for co-occurring autism and depression can feel confusing, especially when every person’s experience is unique. We’ve gathered the most common questions we hear from adults and families seeking support, and we’re here to answer them honestly and clearly.
What does depression look like in an autistic adult?
Depression doesn’t always announce itself with tears or verbal expressions of sadness—especially in autistic adults. Instead, you might notice an increase in repetitive behaviors (stimming) as a way to self-soothe, or a person might withdraw even more than usual, pulling away from activities and relationships. One of the most telling signs is a loss of interest in special interests—the things that once brought joy and focus suddenly feel meaningless.
Physical signs matter too. Depression can show up as heightened sensory sensitivities, where lights feel too bright, sounds too loud, or textures unbearable. Many autistic adults also experience what’s known as autistic burnout, a state of profound exhaustion from prolonged masking and sensory overload that closely mimics depression. Complaints like headaches, stomach pain, or chronic fatigue might actually be the body’s way of expressing emotional distress when words don’t come easily.
What is the best therapy for an autistic adult with depression?
The best therapy isn’t one-size-fits-all—it’s individualized and neurodiversity-affirming. That means meeting you where you are, respecting how your brain works, and adapting proven approaches to fit your needs. Adapted Cognitive Behavioral Therapy (CBT) is often highly effective because it can be modified to use concrete examples, visual aids, and literal language instead of abstract concepts. This makes it accessible for autistic thinkers while still addressing the core patterns of depression.
Dialectical Behavior Therapy (DBT) is another powerful option, particularly for managing intense emotions, sensory overload, and social stress. DBT’s structured, skill-based format resonates well with many autistic individuals. The key is finding a therapist who understands both conditions and can adjust their approach—using clear communication, respecting processing time, and incorporating your strengths and interests into the work.
Can you be misdiagnosed with depression if you have autism?
Absolutely—and it happens more often than it should. This problem is called diagnostic overshadowing, and it occurs when a clinician mistakenly attributes symptoms like social withdrawal, flat affect, or difficulty expressing emotions solely to autism, missing the separate, co-occurring depression entirely. An autistic person might be experiencing profound sadness, hopelessness, and loss of interest, but because they’re already autistic, these symptoms get dismissed as “just part of autism.”
This is why it’s crucial to seek assessment from a professional experienced in adult autism who understands how the two conditions can present together and knows how to distinguish between them. A thorough evaluation considers the full picture—changes in behavior, baseline functioning, and the unique ways depression manifests in autistic individuals.
Does insurance cover autism and depression treatment for adults?
Good news: many insurance plans do cover dual-diagnosis treatment for adults with co-occurring autism and depression. Plans like Cigna, Optum, and Florida Blue often include coverage for Intensive Outpatient Programs (IOP), Partial Hospitalization Programs (PHP), and virtual therapy options. However, coverage varies widely depending on your specific plan, so verify your benefits before starting treatment.
At Thrive Mental Health, we make this process easier. You can check your coverage quickly, and our team can help you understand what’s included. Don’t let insurance uncertainty stop you from getting help—most plans recognize the medical necessity of treating both conditions together.
How do I start with Thrive Mental Health?
Starting is simple, and there’s no pressure. You can verify your insurance in 2 minutes with no obligation—just a quick check to see what’s covered. If you prefer to talk with someone directly, call 561-203-6085 to speak with a care coordinator who can answer your questions, explain our programs, and help you take the first step.
We offer virtual and hybrid IOP/PHP programs with evening options, making it easier to fit treatment into your life. Whether you’re in Indiana, California, or anywhere nationwide, our neurodiversity-affirming care is designed for adults like you. You deserve support that understands both autism and depression—and we’re here to provide it.
Take the First Step Toward Healing
You’ve made it this far, and that matters. Reading about co-occurring autism and depression, learning what specialized care looks like, understanding your options—that takes courage. And it means you’re ready to consider something different.
Finding the right support for co-occurring autism and depression isn’t just about managing symptoms or checking boxes on a treatment plan. It’s about something much bigger: creating a life of purpose and connection. It’s about waking up with energy to pursue your interests, building relationships that feel genuine, and navigating your world without constantly feeling overwhelmed or misunderstood.
Specialized, neurodiversity-affirming care that integrates therapy, life skills, and personalized support is the key to long-term well-being. When treatment centers understand how your brain works—when they adapt their approach to accommodate your sensory needs, communication style, and executive function challenges—recovery stops being a distant hope and becomes a real, achievable path forward.
You don’t have to steer this journey alone. At Thrive Mental Health, we’ve built our programs specifically for adults like you who are asking, “What are the best treatment centers for adults with co-occurring autism and depression?” We offer virtual and hybrid Intensive Outpatient (IOP) and Partial Hospitalization (PHP) programs with evening options, making it easier to fit treatment into your life rather than forcing your life to fit around treatment.
Our team understands that traditional therapy settings can be overwhelming. That’s why we’ve created sensory-friendly environments, offer flexible scheduling, and use communication methods that actually work for autistic adults. We accept major insurance providers including Cigna, Optum, and Florida Blue, and we serve clients nationwide, with specialized support for Indiana and California residents.
If you’re curious about how to choose the right program for your specific needs, our related article on How to Choose the Right Virtual IOP for Autism & Depression offers additional guidance.
Ready to take the next step? You can verify your insurance in 2 minutes with no obligation—just answers about what’s possible. Or if you’d prefer to talk with someone directly, call us at 561-203-6085 to speak with a care coordinator who understands what you’re going through.
If you’re in crisis right now, please call or text 988 to reach the Suicide and Crisis Lifeline. You deserve support, and help is available 24/7.
Your path to healing starts with one small step. We’re here when you’re ready to take it.