Therapy on a Budget: How to Find Mental Health Care Your Insurance Actually Covers

How to Find Covered Therapy: 5 Smart Steps
How to Find Mental Health Providers My Insurance Will Cover—and Maximize Benefits: 5-Step Playbook
Confusing insurance rules and hidden fees push too many people to overpay—or skip care. This guide shows exactly how to find mental health providers your plan actually covers so you can start treatment without surprise bills and fully use the benefits youre already paying for.
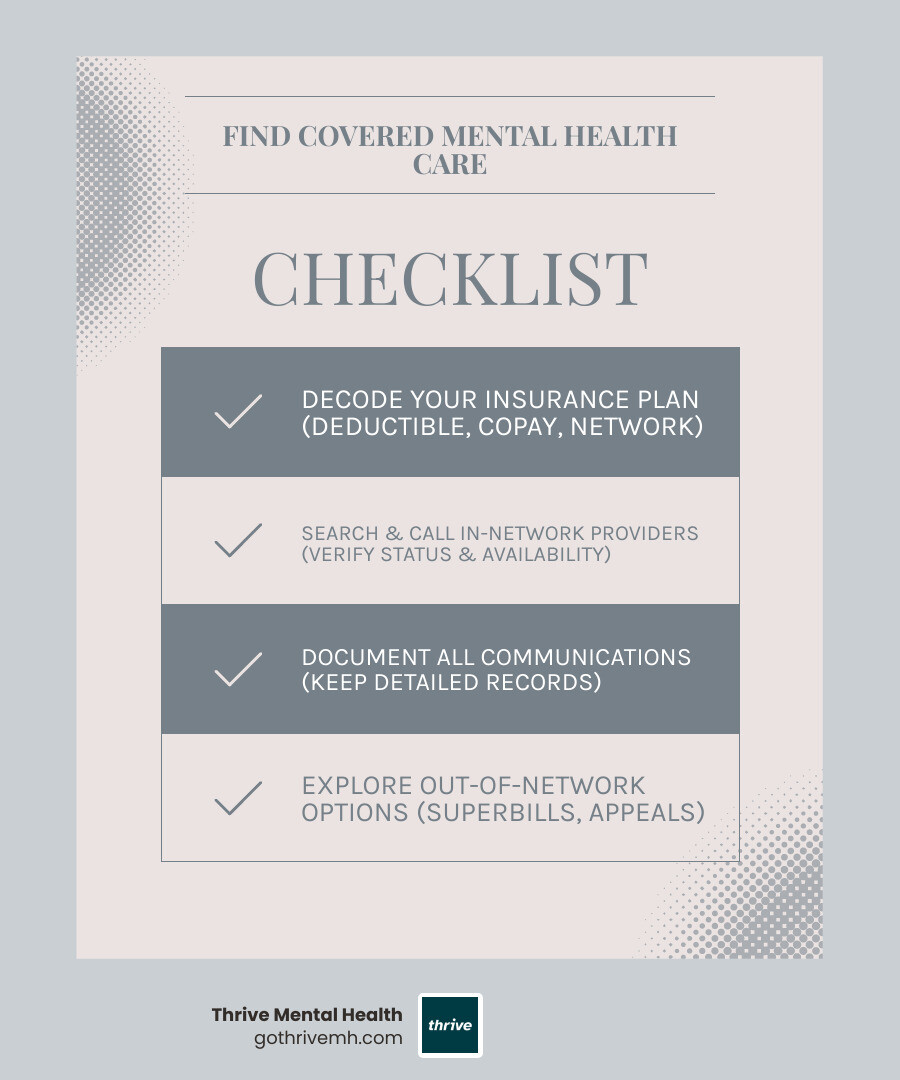
Quick Answer: 5 Steps to Find Covered Mental Health Care
- Check your plan details Look up your deductible, copay, and in-network benefits on your insurance card or member portal.
- Search your insurer’s provider directory Use filters for location and specialty, but be prepared to verify everything.
- Call providers to confirm Ask: “Are you in-network with [Your Plan Name]?” and “Are you accepting new patients?”
- Document everything Keep notes of who you called, when, and what they said.
- Use out-of-network benefits if needed Request a superbill for reimbursement if no in-network provider is available.
The reality is harsh: over 120 million Americans live in mental health shortage areas, and many therapists don’t accept insurance. Even when your plan lists “in-network” providers, you often encounter “ghost networks”outdated lists with retired clinicians or providers who no longer accept your plan.
Federal law says your insurance must cover mental health care at the same level as physical health care. The Mental Health Parity Act and the Affordable Care Act made mental health services an essential benefit for most plans. But knowing your rights and using them are two different things. This guide gives you the exact steps to verify coverage and get the therapy you need without surprise bills.
I’m Anna Green, LMHC, LPC, Chief Clinical Officer at Thrive Mental Health. For over a decade, I’ve helped thousands of people steer insurance barriers to access IOP and PHP programs. My mission is to make high-quality mental health care easier to start, stick with, and affordstarting with this article.
Understanding Your Mental Health Coverage: The Essentials
Trying to understand your mental health benefits can feel like decoding a secret language. The good news is that federal law is on your side, requiring insurance plans to treat mental and physical health care equally. Let’s break down what that means for you.
The Mental Health Parity and Addiction Equity Act (MHPAEA) of 2008 made it illegal for insurance companies to treat mental health care as a “lesser” benefit. If your plan covers mental health, it must do so on par with medical care, meaning equal financial requirements (deductibles, copays) and treatment limits.
Under the Affordable Care Act, mental health and substance use disorder services are considered Essential Health Benefits. This means most plans must cover behavioral health treatment (like therapy), mental health inpatient services, and substance use disorder treatment, including programs like IOP and PHP.
Furthermore, insurers can no longer deny you coverage, charge higher premiums, or exclude treatment for pre-existing conditions like depression or anxiety. Your coverage starts when your plan does. The ACA also eliminated lifetime or annual dollar limits on essential health benefits, so you don’t have to worry about your coverage running out.
Your care needs will determine whether you need inpatient or outpatient therapy. Outpatient care is typically weekly sessions, while inpatient care involves staying at a facility. A middle ground exists with Intensive Outpatient Programs (IOP) and Partial Hospitalization Programs (PHP), which offer structured daily therapy while you live at home. At Thrive Mental Health, we specialize in these flexible virtual and hybrid programs.
A tricky area is Non-Quantitative Treatment Limits (NQTLs)—rules like prior authorization or medical necessity reviews. Parity laws state these rules cannot be more restrictive for mental health than for physical health. If your plan doesn’t require prior authorization for a specialist visit, it shouldn’t for a therapy session.
Understanding how to find mental health providers my insurance will cover to maximize benefits begins with knowing these protections. For more details, see our guide: Do Insurance Plans Have to Offer Mental Health Benefits?
Your Rights Under Federal Law
These protections are law, not suggestions. If you have a Marketplace plan or a large employer plan, mental health parity rules apply to you.
Parity protections mean your financial requirements (copays, deductibles) and treatment limits (session counts) must be comparable for mental and physical health services. A $30 copay for your primary care doctor should mean a similar copay for your therapist, not $100.
Care management rules like prior authorization cannot be more burdensome for mental health care. If your plan requires extensive paperwork for therapy but not for a comparable medical procedure, it may be a parity violation. For more on federal requirements, visit: Coverage for mental health and substance abuse
Common Insurers in Florida
If you’re in Florida—a key state where Thrive Mental Health operates—you’ll likely encounter these major insurers:
Florida Blue is a dominant player across the state. Cigna and Optum (which often manages UnitedHealthcare’s behavioral benefits) also have large networks in major cities like Miami, Orlando, and Tampa.
These companies offer extensive networks, but your specific plan (HMO, PPO, EPO) determines which providers you can see and what you’ll pay. A Florida Blue plan in Jacksonville may have a different network than one in Fort Lauderdale. At Thrive Mental Health, we work with many of these insurers across Florida to provide accessible care. Learn more here: Exploring Mental Health Resources with Cigna and UnitedHealthcare
Step-by-Step: How to Find Mental Health Providers My Insurance Will Cover to Maximize Benefits
You know your rights; now it’s time to find a provider. This is where many people get stuck, but this guide will walk you through it.
Step 1: Decode Your Insurance Plan
Before you start your search, understand your plan to avoid costly mistakes.

First, learn these key terms:
- Deductible: The amount you pay out of pocket before your insurance begins to pay. This resets annually.
- Copay/Coinsurance: After meeting your deductible, you’ll pay either a copay (a flat fee, like $30) or coinsurance (a percentage of the cost, like 20%) for each session.
- Out-of-Pocket Maximum: The most you will pay for covered services in a year. Once you hit this limit, your insurance pays 100%.
- Precertification/Prior Authorization: Some plans require approval before you start treatment, especially for intensive programs like IOP or PHP. Skipping this step can lead to a denied claim.
- In-Network vs. Out-of-Network: In-network providers have contracts with your insurer and cost less. Out-of-network providers do not, and you will pay significantly more.
You can find this information on your insurance card, online member portal, or by calling customer service. For a detailed tutorial, read our guide: How to Read Mental Health Insurance Benefits. Also, find your Summary of Benefits and Coverage (SBC) online; it’s a detailed document explaining your plan’s coverage and costs.
Step 2: Find In-Network Providers (and Avoid Outdated Directories)
Finding an in-network therapist should be easy, but insurer directories are often inaccurate. These “ghost networks” list retired clinicians or providers who no longer take your insurance, wasting your time.
Start with your insurer’s online portal. Use the “Find a Provider” tool and filter by specialty, location, and availability. Make a list, but don’t stop there.
Next, call your insurance company directly. Ask for an up-to-date list of in-network mental health providers accepting new patients for your specific plan.
The golden rule: confirm everything directly with the provider’s office. Call each office and ask: “Are you currently in-network with [Your Insurance Company] for [Your Specific Plan Name]?” Give them your member ID to verify. Also, ask if they are accepting new patients and what their wait time is. This step prevents the shock of a large bill for a provider you thought was covered.
Document every call. Note the date, time, who you spoke with, and what they said. Use a worksheet to stay organized: Handy worksheet for tracking calls. This documentation is crucial. If you can’t find an available in-network provider after a “good faith effort” (5-10 calls), you have proof that your insurer may be violating network adequacy laws. With this proof, you can demand they help you find care or authorize an out-of-network provider at in-network rates.
Step 3: Choose the Right Type of Provider for Your Needs
Not all mental health providers offer the same services. Knowing the difference helps you find the right fit faster.
| Provider Type | Credentials | Focus & Services Offered | Can Prescribe Medication? |
|---|---|---|---|
| Psychiatrist | MD or DO | A medical doctor specializing in diagnosing mental illnesses and medication management. | Yes |
| Psychologist | PhD or PsyD | Specializes in diagnosing and treating conditions through psychotherapy (talk therapy). | Rarely (in some states) |
| Psychiatric Nurse | PMHN (RN); PMHNP (APRN) | PMHNs provide nursing care. PMHNPs can diagnose, treat, and prescribe medication. | PMHNP: Yes |
| Physician Assistant | PA | Works under a physician; can specialize in psychiatry, diagnose, treat, and prescribe. | Yes |
| Licensed Clinical Social Worker | LCSW (MSW + supervised clinical hours) | Provides assessment, diagnosis, and psychotherapy, focusing on social environment factors. | No |
| Licensed Professional Counselor | LPC (Master’s degree + supervised clinical hours) | Provides individual, group, and family counseling for various mental and emotional issues. | No |
| Marriage and Family Therapist | MFT (Master’s degree + supervised clinical hours) | Specializes in relational issues within families and couples. | No |
If you think you need medication, see a psychiatrist, psychiatric nurse practitioner (PMHNP), or physician assistant. If you’re looking for talk therapy (like CBT or DBT), you’ll likely work with a psychologist, LCSW, LPC, or MFT. Many people see both a prescriber and a therapist.
Look for providers who specialize in your specific concerns, such as trauma, anxiety, or substance use. Their expertise can make a significant difference in your treatment. Learn more here: Choosing a mental health provider. The goal is to find the right provider for you to truly maximize your benefits.
What to Do When You Can’t Find a Covered Provider
Even with your best effort, you might hit a wall. You’ve made the calls, but no one is available. It’s exhausting, and it’s not your fault. Here’s how to move forward when in-network options are scarce.
Leveraging Out-of-Network (OON) Benefits
If your ideal therapist isn’t in-network, you may still have financial help through your plan’s out-of-network benefits.
Here’s how it works: You pay the therapist their full fee upfront. They provide you with a superbill—a detailed, itemized receipt with all the necessary codes for insurance. You submit this superbill and a claim form to your insurance company for reimbursement. Always keep copies of everything you submit.
The catch: your out-of-network deductible is usually higher than your in-network one. Once you meet it, your insurer will reimburse you for a percentage of the allowed amount—the fee they deem reasonable for that service. This amount may be less than what your therapist charges, and you’ll be responsible for the difference.
For example: Your therapist charges $150, but your insurance’s allowed amount is $100. If your plan covers 60% of OON services, you’d get $60 back. Your out-of-pocket cost would be $90 per session. It’s not full coverage, but it’s better than paying the entire fee yourself.
Understanding OON benefits is especially important for specialized treatments like Dialectical Behavior Therapy (DBT). Learn more here: Understanding Insurance Coverage for Dialectical Behavior Therapy
Appealing a Denial: How to Fight for Coverage
An insurance denial is frustrating, but it’s not the final word. Many denials are overturned on appeal.
Denials often cite a lack of “medical necessity,” meaning the insurer doesn’t agree with the level of care your provider recommends. When you get a denial letter, read it carefully. It must explain the reason for the denial and your right to appeal, including strict deadlines.
Your first step is an internal appeal with your insurance company. To build a strong case, gather your call logs, the claim information, and a letter from your provider explaining why the treatment is medically necessary. Submit everything in a formal written appeal via certified mail. Be clear, factual, and reference the Mental Health Parity Act if you suspect discrimination.
If the internal appeal is denied, you have the right to an external review. An independent third party will review your case and make a binding decision. Your denial letter will explain how to request this.
You also have other allies. For fully insured plans, contact your state insurance department. They can investigate whether your insurer is following the law. For self-funded plans (common with large employers), contact the U.S. Department of Labor’s Employee Benefits Security Administration. They oversee compliance with federal laws like mental health parity. You can reach them here: U.S. Department of Labor’s Employee Benefits Security Administration
Finally, file a formal grievance with your insurance company whenever you encounter barriers like inaccurate directories or unreasonable denials. This creates an official record and helps hold insurers accountable. Fighting for the coverage you pay for is worth the effort.
Maximizing Your Benefits & Finding Affordable Alternatives
Beyond finding a covered provider, smart financial strategies and alternative options can make mental health care more affordable.
Smart Financial Planning for Therapy
Strategically using your benefits can save you money. Here’s how to find mental health providers my insurance will cover to maximize benefits by planning ahead:

- Meet Your Deductible: Once your deductible is met for the year (from any medical expenses), your out-of-pocket costs for therapy will drop significantly. Consider scheduling more intensive care, like our IOP or PHP programs, before the year ends to take advantage of this.
- Use Your Out-of-Pocket Max: If you’re close to hitting your annual out-of-pocket maximum, any further care will likely be covered at 100% by your insurance.
- Use Your HSA/FSA: Health Savings Accounts (HSA) and Flexible Spending Accounts (FSA) are tax-advantaged funds perfect for mental health expenses. FSA funds are often “use it or lose it,” so don’t let them expire at the end of the year.
- Plan During Open Enrollment: When choosing a plan for next year, review your anticipated mental health needs. A plan with a lower deductible or better mental health benefits might be worth it.
For more on finding budget-friendly plans, see our guide on Affordable Health Plans.
Exploring Low-Cost & Alternative Care Options
If insurance remains a barrier, don’t give up. Several other options exist:
- Employee Assistance Programs (EAP): Many employers offer free, confidential, short-term counseling and referrals through an EAP.
- Sliding-Scale Fees: Ask providers if they offer fees based on your income. Many do.
- Telehealth and Virtual Therapy: Virtual therapy is often just as effective as in-person care and expands your provider options. Our virtual IOP and PHP programs at Thrive Mental Health offer expert-led care from anywhere.
- Certified Community Behavioral Health Clinics (CCBHCs): These clinics provide comprehensive services at free or low cost, regardless of your ability to pay. Find one near you with this tool: Find a CCBHC near you.
To understand how insurance covers virtual care, read more here: Virtual IOP Insurance.
Frequently Asked Questions about Finding Covered Mental Health Care
You’re serious about understanding how to find mental health providers my insurance will cover to maximize benefits. Here are answers to the most common questions.
How do I know if a therapist really takes my insurance?
Call the therapist’s office directly. Ask, “Are you currently in-network with [Your Specific Plan Name]?” and provide your member ID. Insurer directories are often outdated, so direct confirmation is the only way to be certain. A two-minute call can save you from a surprise bill.
What’s the difference between a copay, deductible, and out-of-pocket maximum?
- Deductible: The amount you pay out-of-pocket before your insurance starts paying.
- Copay: A flat fee you pay per session after your deductible is met (e.g., $30).
- Out-of-Pocket Maximum: The absolute most you’ll pay for covered care in a year. After you hit this limit, your insurance pays 100% for the rest of the year.
Can my insurance limit how many therapy sessions I have?
Not arbitrarily. Thanks to parity laws, limits on mental health sessions must be comparable to those for medical care. However, your plan may require a “medical necessity” review after a certain number of sessions, where your therapist provides justification for continued care. If you feel the limits are unfair, it could be a parity violation you can appeal.
What if I can’t find an in-network therapist in my area?
This is a potential “network adequacy” violation. Document your search (5-10 calls to different providers). If you can’t find an available provider, contact your insurer with your call log and request a network adequacy review. They may be required to authorize an out-of-network provider at in-network rates to fill the gap in their network.
Does Thrive Mental Health accept my insurance?
We work to be in-network with most major insurance providers for our Intensive Outpatient (IOP) and Partial Hospitalization (PHP) programs. The easiest way to find out is to Verify your insurance in 2 minutes. There’s no obligation, and you’ll get a clear answer about your coverage. You can also call us at 561-203-6085 to walk through your benefits.
Get the Support You Deserve
Navigating insurance for mental health care is challenging, but you have more power than you think. By following the steps in this guide—from decoding your plan to verifying providers and appealing denials—you are taking control of how to find mental health providers my insurance will cover to maximize benefits.
Your mental health is not a luxury. The system isn’t always easy to steer, with its ghost networks and confusing terms, but now you know how to push back. You know your rights under federal law and that mental health care must be treated equally to physical health care.
Keep your documentation organized, make the necessary calls, and remember that advocating for yourself is a sign of strength.
Ready for support? Thrive offers virtual and hybrid IOP/PHP with evening options designed for real life—care that fits your schedule. Verify your insurance in 2 minutes (no obligation) or call 561-203-6085 to speak with someone who can walk you through your benefits. We’re here to make this process as smooth as possible.
If you’re in crisis, call/text 988 right now. You are not alone.
For more information about our programs and how insurance works with intensive care, explore these resources: Virtual IOP Insurance, Affordable Health Plans, Verify Insurance, and Exploring Mental Health Resources with Cigna and UnitedHealthcare.
You deserve care that works. And now you know how to get it.