Feeling Overwhelmed? Understanding Emotional Distress

Emotional Distress: 7 Warning Symptoms to Know
Emotional Distress Is Real—And It’s Costing You
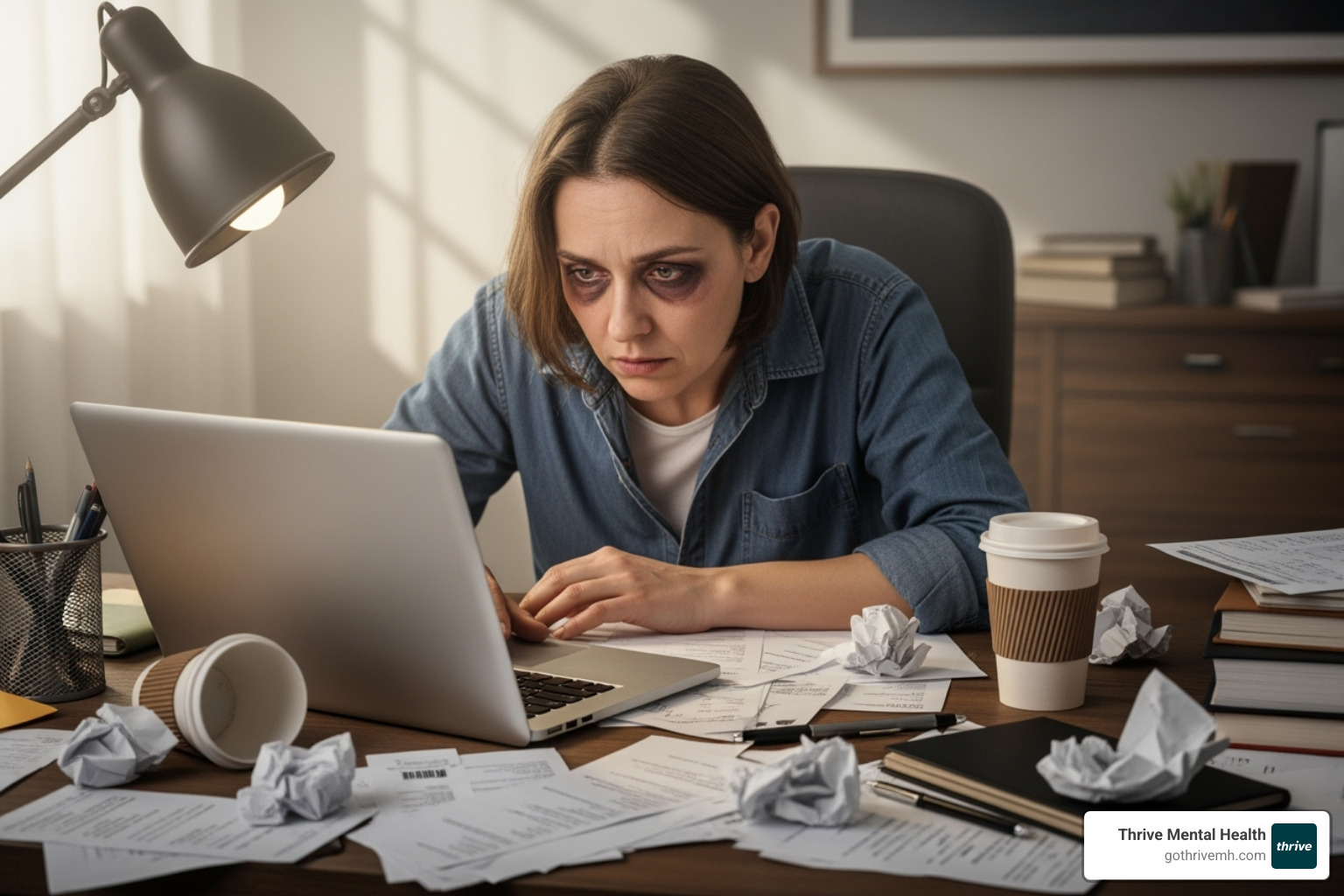
Emotional distress isn’t just a bad week. It’s a state of mental anguish that hijacks your sleep, work, and relationships. Left unchecked, it can spiral into clinical depression or anxiety disorders—and the warning signs are often hiding in plain sight.
It’s a prolonged emotional reaction—anguish, fury, or despair—that interferes with daily life, stemming from trauma, burnout, or conflict. Unlike everyday stress, emotional distress lingers, drains your energy, and can cause physical symptoms like headaches and chronic fatigue.
Key facts:
- 20% to 40% of cancer patients experience intense emotional distress.
- Working over 69 hours per week increases your risk of depression.
- Even low levels of distress can raise your risk of arthritis and cardiovascular disease.
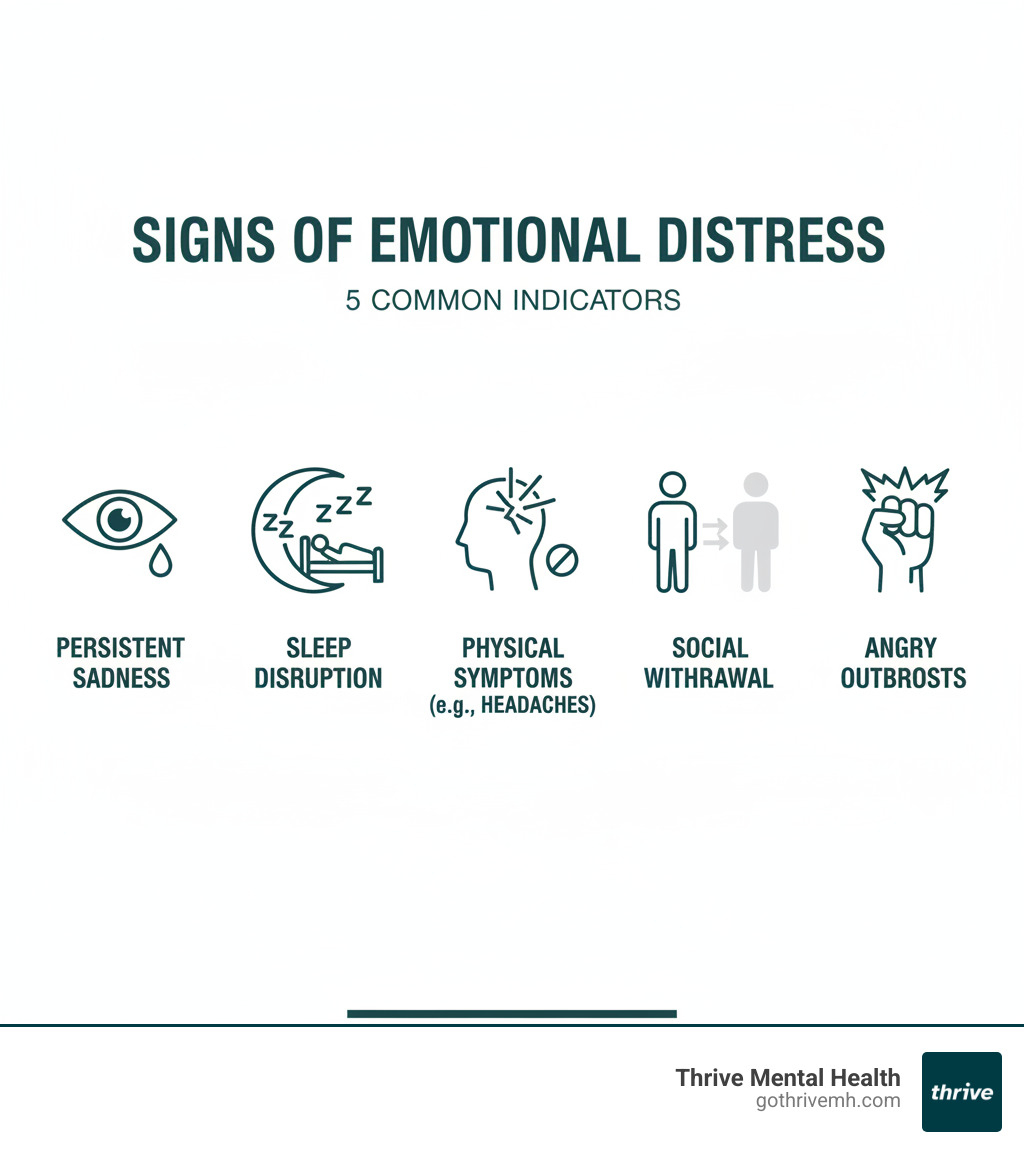
- Distress can trigger insomnia, weight changes, angry outbursts, and social withdrawal.
If you’re in crisis, call/text 988 right now. You are not alone.
I’m Anna Green, LMHC, LPC, Chief Clinical Officer at Thrive Mental Health. I’ve spent my career treating emotional distress, and I’ve seen how early intervention changes lives. This guide will show you the red flags, root causes, and the fastest path to relief.
Glossary for emotional distress:
What Are the Red Flags? 7 Symptoms of Emotional Distress You Must Know
When emotional distress takes hold, it doesn’t just live in your head. It rewires your thoughts, attacks your body, and changes how you act. Many people dismiss these signs as “just stress” until they can’t be ignored. Emotional distress speaks three languages: psychological, physical, and behavioral. Miss the signs, and you miss the message your mind and body are sending.

Psychological Symptoms: The Inner Turmoil
Your mind is the first battleground. Constant worry and racing thoughts take over as your brain replays worst-case scenarios. This anxiety hijacks your daily life, making focus impossible. You might feel sudden irritability and anger, snapping at loved ones over small things, followed by an unshakable sense of guilt or self-blame. Hopelessness and helplessness creep in, draining your motivation. Some experience crying spells, while others feel emotionally numb. Your ability to think and concentrate plummets, leaving you in a mental fog.
Physical Symptoms: When Your Body Speaks
Emotional pain often shows up as real physical symptoms, a process called somatization. You might suffer from pounding headaches, stomach cramps, or irritable bowel symptoms with no clear medical cause. You feel exhausted no matter how much you rest. Research shows this mind-body connection is undeniable. Sleep problems are nearly universal, along with chronic muscle pain in your neck and back. Your appetite may disappear or spike, leading to weight changes. These physical symptoms are your body’s alarm system screaming that something is wrong.
Behavioral Symptoms: Changes in How We Act
This is where others start to notice something is off. You might begin withdrawing socially, canceling plans and ignoring friends. At work or home, you neglect responsibilities as deadlines slip and chores pile up. Some people turn to alcohol or drugs to numb the pain, while others engage in high-risk behaviors like reckless spending or unsafe sex. Avoidance becomes your default strategy. Recognizing this pattern early is key—before it spirals.
Table: Emotional vs. Physical Symptoms—What to Watch For
| Category | Emotional Symptoms | Physical Symptoms |
|---|---|---|
| Psychological | Constant worry, racing thoughts, irritability, hopelessness, guilt, crying spells, difficulty concentrating, emotional numbness | Headaches, migraines, stomach pain, nausea, chronic fatigue, muscle tension, heart palpitations |
| Behavioral | Social withdrawal, neglecting work or family, increased substance use, high-risk behaviors, avoidance | Sleep disturbances, appetite changes, weight fluctuations, low energy |
If you see yourself in this list, you’re not broken. These symptoms respond to treatment. The faster you act, the faster you can reclaim your life. If you’re ready, Thrive’s virtual IOP and PHP programs are designed to provide flexible, evidence-based care.
Why Am I So Overwhelmed? Top Triggers and Risk Factors
Emotional distress often isn’t a single event but a slow accumulation of pressure—bills, a demanding boss, a crumbling relationship. Understanding what triggers it isn’t about blame; it’s about recognizing when you’re in the danger zone so you can act before you hit a wall.
When Work Becomes the Problem
When your job is a source of constant stress, it bleeds into everything. Long hours are a major culprit; a 2021 study linked working over 69 hours a week to higher rates of depression. Toxic workplace cultures—harassment, bullying, or a lack of support—are equally damaging. The World Health Organization identifies job insecurity, performance pressure, and lack of control as key factors that erode mental health. Pay inequity and financial struggles add another layer of demoralizing stress.
Financial Strain and Life’s Curveballs
Financial difficulties like debt or job loss create a constant state of anxiety. Major life changes, even positive ones like moving or becoming a parent, can be overwhelming. Painful events like divorce or the death of a loved one hit even harder. When your closest relationships are filled with conflict, you lose a critical buffer against stress, and emotional distress often follows.
Trauma, Discrimination, and Invisible Burdens
Past traumatic experiences like abuse or violence leave lasting marks. If you’re carrying unhealed wounds, you might benefit from reading about Healing from Childhood Trauma—What Works. Chronic stress also comes from societal burdens like discrimination and racism. Microaggressions based on race, gender, or sexual orientation create a relentless strain. Loneliness, social isolation, and chronic illness are other powerful, often overlooked, triggers.
List: 8 Most Common Causes of Emotional Distress
- Workplace Stress: Long hours, toxic environments, job insecurity.
- Financial Strain: Debt, job loss, inability to meet basic needs.
- Relationship Issues: Conflict, divorce, loneliness.
- Traumatic Events: Abuse, accidents, violence, harassment.
- Grief and Loss: Death of a loved one, loss of routine.
- Discrimination: Racism, prejudice, ableism.
- Major Life Changes: Moving, new parenthood, transitions.
- Chronic Illness/Pain: Ongoing health challenges.
Recognizing these triggers is about understanding when you need support. When stressors become chronic, your resilience wears thin. That’s not weakness; it’s being human.
Emotional Distress vs. Mental Health Disorder—What’s the Difference?
Many people confuse emotional distress with a mental health disorder. Understanding the difference is critical to getting the right help.
Distress Is a Reaction—Not Always a Diagnosis
Emotional distress is your mind and body’s alarm system—an overwhelming sense of anguish in response to life’s challenges. It’s a warning light, not a formal medical diagnosis found in the DSM-5. Distress can be temporary; it may lift once the stressor passes or you find ways to cope. Anyone can experience it without having a diagnosable disorder. The key questions are: how long does it last, and how much is it disrupting your life?
Mental Health Disorders: When It Becomes Medical
A mental health disorder is a specific, diagnosable medical condition with clear criteria. Think Major Depressive Disorder, Generalized Anxiety Disorder, or PTSD. These aren’t just rough patches; they are conditions with defined symptoms and duration requirements that significantly impair your ability to function. For example, a depression diagnosis requires at least five specific symptoms lasting for at least two weeks. These disorders involve a complex mix of genetics, brain chemistry, and environmental triggers, and they often require professional treatment.
The Dangerous In-Between: When Distress Becomes Disorder
Ignoring emotional distress is a mistake. Persistent distress wears down your coping mechanisms, flooding your body with stress hormones like cortisol. Over time, this can lead to physical health problems, sleep deprivation, and social isolation. When distress becomes so severe that you can’t function, you’re in the danger zone where it can morph into a clinical disorder like depression or anxiety. Don’t wait until the alarm bell becomes a full-blown crisis. For more on this, read our guide on How Mental Disorders Disrupt Your Life.
Table: Emotional Distress vs. Clinical Depression—Causes, Duration, Severity, Treatment
| Feature | Emotional Distress | Clinical Depression (Major Depressive Disorder) |
|---|---|---|
| Definition | Mental anguish in response to life stressors—a warning sign. | A diagnosable medical condition with persistent, specific symptoms. |
| Causes | Work stress, relationship conflict, trauma, financial strain. | Complex mix of genetics, brain chemistry, and environmental factors. |
| Duration | Often temporary; may resolve when stressor is addressed. | Symptoms last at least two weeks, nearly every day. |
| Severity | Ranges from mild to severe. | Severe enough to significantly impair daily functioning. |
| Diagnosis | Not a clinical diagnosis. | Diagnosed by a professional using DSM-5 criteria. |
| Treatment | Self-care, coping skills, short-term therapy. | Psychotherapy (CBT, DBT), medication, IOP/PHP. |
How to Take Back Control—Proven Treatments for Emotional Distress
When emotional distress feels like you’re drowning, it’s easy to feel powerless. But you’re not. Real, evidence-based treatments work, and the right combination can help you reclaim your life. The path forward isn’t one-size-fits-all, but it often involves a mix of daily self-care and professional support.
When Should You Get Professional Help?
How do you know if you need therapy? If you’re asking the question, it’s worth exploring. But these red flags mean it’s time to reach out:
- Symptoms last 2+ weeks: Your brain and body are telling you they need support.
- You can’t function: Missing deadlines, avoiding loved ones, or struggling to get out of bed are signs distress requires intervention.
- Coping skills aren’t working: When your usual tools fail, it’s time for professional guidance.
- You feel isolated or hopeless: Therapy is highly effective for this pervasive feeling.
- Thoughts of self-harm or suicide: This is always an emergency.
If you’re in crisis, call/text 988 right now. You are not alone.
Self-Management: Your Daily Toolkit for Resilience
Building a personal toolkit of coping strategies is essential. These aren’t just nice-to-haves; they are evidence-based practices that reduce distress.
- Grounding Techniques: Use the 5-4-3-2-1 method (name 5 things you see, 4 you touch, etc.) to pull your nervous system back to the present.
- Mindfulness & Meditation: Even five minutes of observing your breath can lower stress hormones.
- Exercise: A 20-minute walk releases endorphins and improves sleep. It’s one of the most underused treatments for distress.
- Sleep Hygiene: Aim for 7-8 hours of quality sleep. It’s foundational for coping.
- Journaling: Get swirling thoughts out of your head and onto paper to process emotions.
- Support Network: Connection is protective. Reach out to one trusted person or a support group.
Professional Help: Targeted Strategies for Lasting Change
Sometimes distress runs too deep for DIY solutions. Seeking professional help is a sign of strength.

- Therapy (Psychotherapy): This is the cornerstone of treatment. Cognitive Behavioral Therapy (CBT) helps you identify and reframe the thoughts that fuel distress. Dialectical Behavior Therapy (DBT) teaches practical skills for managing overwhelming emotions.
- IOP & PHP: Intensive Outpatient Programs (IOP) and Partial Hospitalization Programs (PHP) are for those who need more than weekly therapy but not 24/7 care. At Thrive, our virtual and hybrid programs in Florida offer structured, evidence-based treatment with flexible scheduling.
- Medication: Antidepressants or anti-anxiety medications can help regulate brain chemistry, especially when combined with therapy.
- Virtual Therapy: Online therapy is just as effective as in-person care, removing barriers like travel and wait times.
We work with major insurance providers in Florida, including Florida Blue, Cigna, Optum, and Aetna. You can Verify Your Insurance in 2 Minutes with no obligation.
6 Evidence-Based Treatments for Emotional Distress
- Cognitive Behavioral Therapy (CBT): Retrains thought patterns that fuel distress.
- Dialectical Behavior Therapy (DBT): Builds coping skills for intense emotions.
- Mindfulness-Based Practices: Develops present-moment awareness.
- Regular Exercise: Reduces stress hormones and boosts mood.
- Healthy Lifestyle Adjustments: Optimizes sleep, nutrition, and social connections.
- Intensive Outpatient (IOP) / Partial Hospitalization (PHP): Provides structured, high-level support.
If trauma is the cause, we offer specialized treatment. Start healing from trauma now.
Emotional Distress and the Law—What You Need to Know
While our focus is healing, the term emotional distress also has a specific meaning in the legal world. In some cases, the anguish you’ve suffered can be grounds for a lawsuit.
Legal vs. Psychological Definitions
Legally, emotional distress is a “highly unpleasant emotional reaction…which results from another’s conduct and for which damages may be sought.” Psychologically, it’s about your internal state of suffering. Courts now often recognize claims for emotional harm alone, especially in cases like sexual harassment where the primary damage is emotional.
When to Consider a Lawsuit
Claims typically fall into two categories:
- Intentional Infliction of Emotional Distress (IIED): When someone’s extreme and outrageous conduct deliberately or recklessly causes you severe emotional harm.
- Negligent Infliction of Emotional Distress (NIED): When someone’s carelessness causes severe emotional suffering, often requiring you to have been physically injured or in the “zone of danger.”
Common scenarios include accidents, workplace harassment, wrongful termination, or discrimination. Proving a case requires showing the defendant breached a duty of care, directly causing you severe, measurable harm. Evidence often includes medical records, expert testimony from mental health professionals, and your own account of how your life has been impacted.
Standards vary by state. For a detailed overview, you can refer to the Legal Definition of Emotional Distress.
Legal Disclaimer: This information is for educational purposes only and is not legal advice. If you believe you have a legal claim, consult a qualified attorney. We are here to help you heal emotionally; for legal matters, you need a lawyer.
FAQs—People Also Ask About Emotional Distress
How long does emotional distress last?
It’s often temporary. However, if it lasts more than a few weeks or disrupts your daily life, it’s a sign to seek professional help before it develops into a more serious mental health issue.
Can you get medication for emotional distress?
While distress itself isn’t a diagnosis, a doctor may prescribe medication (like antidepressants) for an underlying condition like depression or anxiety. Therapy is key for addressing the root causes.
What’s the fastest way to calm emotional distress?
For immediate relief, try grounding techniques (like the 5-4-3-2-1 method) or deep breathing. For lasting relief, you must address the root cause with therapeutic interventions and lifestyle changes.
Does insurance cover treatment for emotional distress?
Yes. In Florida, most health plans from providers like Florida Blue, Cigna, Optum, and Aetna cover mental health services like therapy and IOP/PHP. Thrive Mental Health works with these and other major insurers across Florida. Check your benefits now.
What if I’m having thoughts of self-harm?
This is a critical emergency. Please reach out for immediate help by calling or texting 988. You are not alone, and support is available 24/7. Once you are safe, Thrive can help you build a long-term recovery plan.
Summary—Don’t Wait. Emotional Distress Is Treatable.
Emotional distress is more than just stress—it’s a real health crisis that can disrupt your entire life. Left unchecked, it deepens, increasing your risk for clinical depression, anxiety, and chronic illness. But it is treatable.
Early action means faster recovery. Whether you’re dealing with burnout, trauma, or relationship conflict, there are proven paths forward, and you don’t have to walk them alone. We’ve covered the red flags, the triggers, and the treatments that work, from self-care to professional programs like IOP and PHP.
Waiting makes it harder. Reaching out can change your trajectory in days, not months.
Thrive Mental Health offers virtual and hybrid IOP/PHP programs for adults and young professionals across Florida. Our programs deliver expert care with flexible scheduling, and we accept major insurance plans, including Florida Blue, Cigna, Optum, and Aetna. If trauma is at the root of your distress, we specialize in evidence-based recovery. Start healing from trauma now.
You’ve already recognized something needs to change. Now it’s time to act.
Ready for support in Florida? Thrive offers virtual and hybrid IOP/PHP programs with evening options. Verify your insurance in 2 minutes (no obligation) → Start benefits check or call 561-203-6085. If you’re in crisis, call/text 988.