The Hidden Scars: Recognizing Post-Traumatic Stress Disorder

Post traumatic stress disorder symptoms: 2025 Guide
It’s Not in Your Head, It’s a Reaction to Trauma
Post traumatic stress disorder symptoms are your mind and body’s way of trying to protect you after an overwhelming experience. They are not a sign of weakness—they’re a normal response to an abnormal event.
Quick answer: The four main categories of post traumatic stress disorder symptoms are:
- Re-experiencing symptoms – Flashbacks, nightmares, and intrusive memories.
- Avoidance symptoms – Actively avoiding anything related to the traumatic event.
- Negative changes in thinking and mood – Persistent guilt, shame, distorted beliefs, and emotional numbness.
- Arousal and reactivity symptoms – Being constantly on edge, irritable, hypervigilant, and having trouble sleeping.
For a diagnosis of PTSD, symptoms must last more than one month and significantly interfere with daily life.
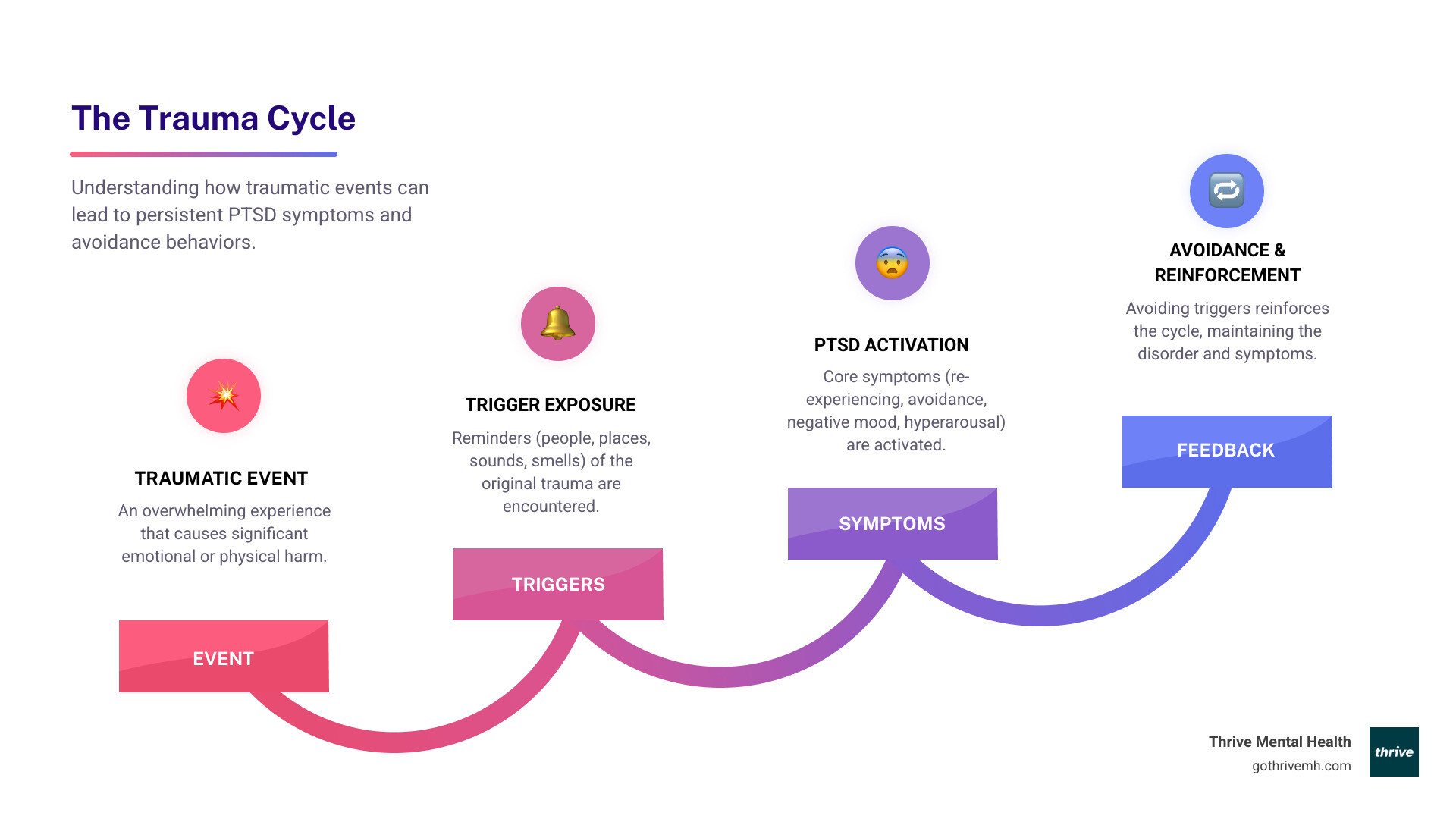
PTSD develops when your brain’s natural fight-or-flight response gets stuck in overdrive. After a traumatic event, most people experience some distress. But for about 6% of people, those reactions don’t fade. Your brain keeps sounding the alarm even when the danger has passed, making you feel like you’re constantly reliving the trauma.
Here’s what matters most: PTSD is treatable. With the right support, most people see significant improvement. Evidence-based therapies like Cognitive Behavioral Therapy (CBT) and Eye Movement Desensitization and Reprocessing (EMDR) can help your brain process the trauma. For many, intensive outpatient programs (IOPs) deliver faster results than traditional weekly therapy.
I’m Nate Raine, CEO of Thrive Mental Health. Our mission is to change access to quality behavioral healthcare by providing effective, evidence-based solutions for treating post traumatic stress disorder symptoms.
Beyond “Just Stress”: The 4 Core Clusters of Post-Traumatic Stress Disorder Symptoms
If you are having thoughts of harming yourself, call or text 988 immediately to connect with the 988 Suicide & Crisis Lifeline. You are not alone.
PTSD isn’t just feeling stressed out. Post traumatic stress disorder symptoms follow specific patterns that mental health professionals use for diagnosis.
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) breaks PTSD into four distinct symptom clusters:
- Intrusion Symptoms: The trauma keeps forcing its way back into your thoughts.
- Avoidance Symptoms: You go out of your way to dodge anything trauma-related.
- Negative Changes in Cognition and Mood: Your worldview shifts to become darker and more negative.
- Arousal and Reactivity Symptoms: Your nervous system stays locked in high-alert mode.
For a clinical diagnosis, a person must experience a specific number of symptoms from each category for more than one month. Crucially, these symptoms must be severe enough to disrupt your ability to function at work, in relationships, or in other important areas of your life.
This time requirement is what separates PTSD from acute stress disorder. Your brain needs time to process what happened, but when symptoms persist and interfere with your life, it’s a sign that professional help is needed. Understanding which symptoms you’re experiencing helps clinicians at places like Thrive’s trauma-focused virtual IOP, available to residents throughout Florida, create a targeted treatment plan to help you heal.
1. Re-Experiencing Symptoms: The Trauma on Repeat
Re-experiencing means the trauma doesn’t stay in the past. It forces its way into your present, uninvited and unwanted. This is one of the most distressing aspects of post traumatic stress disorder symptoms.
- Flashbacks: These aren’t just memories; they are episodes where you feel like the traumatic event is happening all over again. You might see, hear, or smell things from that moment, and your body reacts as if the danger is real.
- Nightmares: You may have terrifying dreams about the event or variations of it, waking up with a racing heart and lingering fear. Many people with PTSD begin to avoid sleep to prevent these nightmares.
- Intrusive Thoughts: Unwanted images or memories from the trauma flash through your mind without warning, making it hard to focus on daily life.
- Physical and Emotional Reactions: Encountering a reminder of the trauma (a trigger) can cause intense emotional distress or physical reactions like a racing heart, sweating, nausea, or trouble breathing.
Common triggers for re-experiencing include:
- Sounds like sirens, fireworks, or slamming doors
- Smells such as smoke, perfume, or gasoline
- Places that are similar to where the trauma occurred
- Dates like anniversaries of the event
- Sensations like being touched unexpectedly
These symptoms are your brain’s misguided attempt to keep you safe. Therapies like trauma-focused care can help you process these memories so they lose their power, allowing you to encounter reminders without being pulled back into the trauma.
2. Avoidance Symptoms: Running from Reminders
When post traumatic stress disorder symptoms feel overwhelming, your brain’s instinct is to avoid anything connected to the trauma. While this provides short-term relief, it strengthens PTSD over time by reinforcing that the reminders are dangerous.
Avoidance can manifest in two main ways:
-
Avoiding External Reminders: You actively stay away from people, places, conversations, or situations that remind you of the trauma. A veteran might avoid crowds, or an accident survivor might take a longer route to work. This can make your world feel smaller and smaller.
-
Avoiding Internal Reminders: You try to suppress thoughts, feelings, or memories related to the event. This often leads to emotional numbing, where you feel disconnected from others and unable to experience positive emotions like joy or love. You might feel hollow or like you’re just going through the motions.
Many people also use work, hobbies, or other activities as a way to constantly distract themselves and keep their minds occupied. This becomes a problem when the busyness is a strategy to avoid processing what happened.
Trauma-focused therapy helps you break this cycle by gradually and safely facing trauma-related thoughts and reminders, allowing you to reclaim the parts of your life that avoidance has taken away.
3. Negative Changes in Cognition & Mood: How Trauma Warps Your Worldview
Trauma can fundamentally change how you see yourself, others, and the world. These shifts are some of the most insidious post traumatic stress disorder symptoms because they quietly erode your sense of self.
Common changes include:
- Persistent Negative Beliefs: Developing core beliefs like “I am bad,” “No one can be trusted,” or “The world is completely dangerous.”
- Distorted Blame: Blaming yourself for the event (“It was my fault”) or misplacing blame on others, which keeps you stuck in guilt and shame.
- Memory Problems: Being unable to recall important parts of the traumatic event, a form of dissociative amnesia.
- Persistent Negative Emotions: Constantly feeling fear, anger, guilt, or shame, even in safe situations.
- Loss of Interest (Anhedonia): Losing interest in hobbies and activities that once brought you joy.
- Feeling Detached: Feeling estranged from friends and family, as if you’re watching your life from behind a pane of glass (depersonalization/derealization).
These cognitive and mood symptoms are not a personal failing; they are a direct result of trauma’s impact on the brain. Therapies like Cognitive Behavioral Therapy (CBT) and EMDR are specifically designed to challenge these distorted thoughts and help your brain reprocess the trauma. Our trauma-focused care programs work intensively on these symptoms to help you rebuild a more compassionate view of yourself and the world.
4. Arousal & Reactivity Symptoms: Constantly on High Alert
Living with arousal and reactivity symptoms feels like your body’s alarm system is stuck in the “on” position. Your nervous system remains in a state of fight-or-flight, constantly scanning for threats even when you’re safe. This is one of the most physically and mentally exhausting aspects of post traumatic stress disorder symptoms.
Key symptoms include:
- Irritability and Angry Outbursts: Small frustrations can trigger intense anger because your nervous system interprets everything as a potential threat.
- Reckless or Self-Destructive Behavior: Engaging in behaviors like substance abuse or dangerous driving as a way to cope with internal distress or feel something other than numbness.
- Hypervigilance: Constantly scanning your environment for danger, making it impossible to relax. You might always need to sit with your back to a wall or monitor exits.
- Exaggerated Startle Response: Having an intense physical reaction (jumping, heart racing) to loud noises or sudden movements.
- Problems with Concentration: Struggling to focus on tasks or conversations because your brain is prioritizing perceived survival needs.
- Sleep Disturbances: Difficulty falling or staying asleep, or having restless sleep that leaves you exhausted.
These symptoms are a sign that your nervous system is overwhelmed. Trauma-focused care uses evidence-based therapies to help regulate your threat response, teaching your body that it’s safe to turn down the alarm and finally rest.
When Trauma Hits Home: Recognizing PTSD Symptoms in Children & Teens

Because their brains are still developing, post traumatic stress disorder symptoms in children and teens can look very different from those in adults. Symptoms can also be misdiagnosed as other conditions, like ADHD, so an evaluation from a childhood trauma specialist is crucial.
For younger children (under 6):
Trauma often shows up in their behavior. Look for:
- Repetitive play that re-enacts the traumatic event.
- Frightening dreams that may or may not be about the event itself.
- Developmental regression, such as bedwetting after being potty-trained.
- Unusual clinginess or fear of being separated from a parent.
For older children and teens (ages 7-18):
Symptoms may be more similar to adults but can also include:
- Disruptive or disrespectful behavior at home or school.
- Intense guilt or thoughts of revenge related to the trauma.
- Depression, anxiety, or social withdrawal.
- Reckless behavior, such as substance use or dangerous driving.
- A sudden drop in grades or problems with friends.
Kids and teens have an incredible capacity for healing, especially with early intervention. If you’re concerned about your child, the National Child Traumatic Stress Network offers excellent resources. For teens in Florida needing more intensive support, Thrive’s virtual IOP programs offer flexible scheduling that works around school.
Why Me? Understanding the Causes and Risk Factors for PTSD
Developing PTSD is not about being weak or strong. It’s a complex interaction of the traumatic event and various risk factors. While most people experience trauma in their lives, only about 5-10% develop PTSD.
What kinds of events can trigger PTSD?
Any event that involves actual or threatened death, serious injury, or sexual violence can be a trigger. This includes:
- Combat exposure
- Physical or sexual assault
- Serious accidents (car crashes, workplace injuries)
- Natural disasters, such as the hurricanes common in Florida
- Racial trauma and discrimination
- Learning that a loved one experienced a violent or accidental trauma
Why do some people develop PTSD and others don’t?
Several factors can increase your risk:
- Previous trauma, especially in childhood
- Lack of social support after the event
- A family history of mental illness
- High levels of stress at the time of the trauma
Conversely, resilience factors like strong social support and positive coping strategies can protect against PTSD. Understanding these factors helps recognize PTSD as a treatable medical condition.
PTSD vs. Acute Stress Disorder (ASD): What’s the Difference?
ASD and PTSD have similar symptoms, but the key difference is timing. ASD is a short-term reaction, while PTSD is a long-term condition.
| Feature | Acute Stress Disorder (ASD) | Post-Traumatic Stress Disorder (PTSD) |
|---|---|---|
| Onset & Duration | Symptoms last from 3 days to 1 month after the trauma. | Symptoms last for more than 1 month. |
| Prognosis | About half of people with ASD go on to develop PTSD. | Requires treatment; can become chronic if untreated. |
Early intervention is key. Getting support soon after a traumatic event can prevent ASD from developing into long-term PTSD.
From Recognition to Recovery: Your Next Steps [2025 Guide]

Recognizing post traumatic stress disorder symptoms is the first step. The next is getting the right help. PTSD is one of the most treatable mental health conditions, and with evidence-based care, most people see significant improvement.
When to Seek Help
If symptoms have lasted for more than a month and are affecting your work, relationships, or daily life, it’s time to talk to a professional. Early treatment can prevent symptoms from worsening.
If you are having thoughts of harming yourself, call or text 988 immediately.
What Effective Treatment Looks Like
The gold standard for PTSD treatment is trauma-focused psychotherapy, sometimes combined with medication.
- Psychotherapy: Therapies like Cognitive Behavioral Therapy (CBT), Prolonged Exposure (PE), and Eye Movement Desensitization and Reprocessing (EMDR) are proven to help you process traumatic memories and change negative thought patterns.
- Medication: FDA-approved antidepressants like SSRIs (Zoloft, Paxil) can help manage symptoms of anxiety, depression, and sleep problems, making it easier to engage in therapy.
Why Intensive Programs Deliver Faster Results
For many, once-a-week therapy isn’t enough to build momentum. Intensive Outpatient Programs (IOP) and Partial Hospitalization Programs (PHP) offer a higher level of care—multiple therapy sessions per week—while you continue to live at home.
Thrive Mental Health’s virtual and hybrid IOP/PHP programs are designed for adults in Florida who need more intensive support. We provide evidence-based treatments like CBT and EMDR with the frequency needed to create real change. We work with major insurance providers like Florida Blue, Cigna, and Optum, making treatment accessible across the state. We also serve residents in California, Indiana, Arizona, and South Carolina.
Learn more about our trauma-focused care and start your recovery journey.
Frequently Asked Questions about Post-Traumatic Stress Disorder Symptoms
How long do post-traumatic stress disorder symptoms last?
To be diagnosed with PTSD, symptoms must last for more than one month. Without treatment, PTSD can become a chronic condition lasting for years. However, with effective, evidence-based therapies like CBT and EMDR, many people see significant improvement and can dramatically shorten their recovery time.
Can you develop PTSD from a non-life-threatening event?
Yes. The defining factor of a traumatic event is the individual’s perception of it as physically or emotionally harmful or threatening. Events like the sudden death of a loved one, emotional abuse, infidelity, or experiencing racial discrimination can absolutely cause PTSD. Your trauma is valid regardless of whether your life was in danger.
What is the difference between C-PTSD and PTSD?
Traditional PTSD often stems from a single traumatic event. Complex PTSD (C-PTSD) results from prolonged, repeated trauma where escape was difficult or impossible, such as long-term childhood abuse or domestic violence. In addition to the core post traumatic stress disorder symptoms, C-PTSD involves severe difficulties with:
- Emotional regulation (intense, uncontrollable emotions)
- Negative self-concept (deep feelings of worthlessness)
- Relationships (profound issues with trust and intimacy)
Treatment for C-PTSD must address these additional areas. Thrive’s trauma-focused IOP programs, available to residents throughout Florida, are equipped to handle both PTSD and C-PTSD.
When should I seek emergency help for PTSD symptoms?
Seek immediate help if you are experiencing:
- Suicidal thoughts or have a plan to end your life. Call or text 988 or go to the nearest emergency room.
- Thoughts of harming yourself or others.
- Feeling completely overwhelmed, out of control, or losing touch with reality.
These are medical emergencies. Reaching out for urgent support is a sign of strength.
Your Path Forward Starts Now
If you’re reading this, you know that post traumatic stress disorder symptoms don’t just go away on their own. But you don’t have to face this alone, and recovery is happening for people every single day.
At Thrive Mental Health, we’ve built our programs to deliver the right intensity of care to residents of Florida. Our virtual and hybrid IOP/PHP programs offer more support than traditional weekly therapy, with the flexibility to fit your life. We provide evidence-based care for adults across Florida, and also serve residents in California, Indiana, Arizona, and South Carolina.
We’re here to help you process what happened, reclaim your sense of safety, and build a future that feels worth living again. Taking the first step is the hardest part, but it’s also the most important.

Ready for support? Thrive offers virtual and hybrid IOP/PHP programs with evening options for Florida residents. Verify your insurance in 2 minutes (no obligation) → Start benefits check or call 561-203-6085. We work with major insurance providers including Florida Blue, Cigna, and Optum to make treatment accessible. If you’re in crisis, call/text 988.