When Thoughts Turn Dark: Active vs Passive Suicidality

Understanding the Spectrum of Suicidal Thoughts
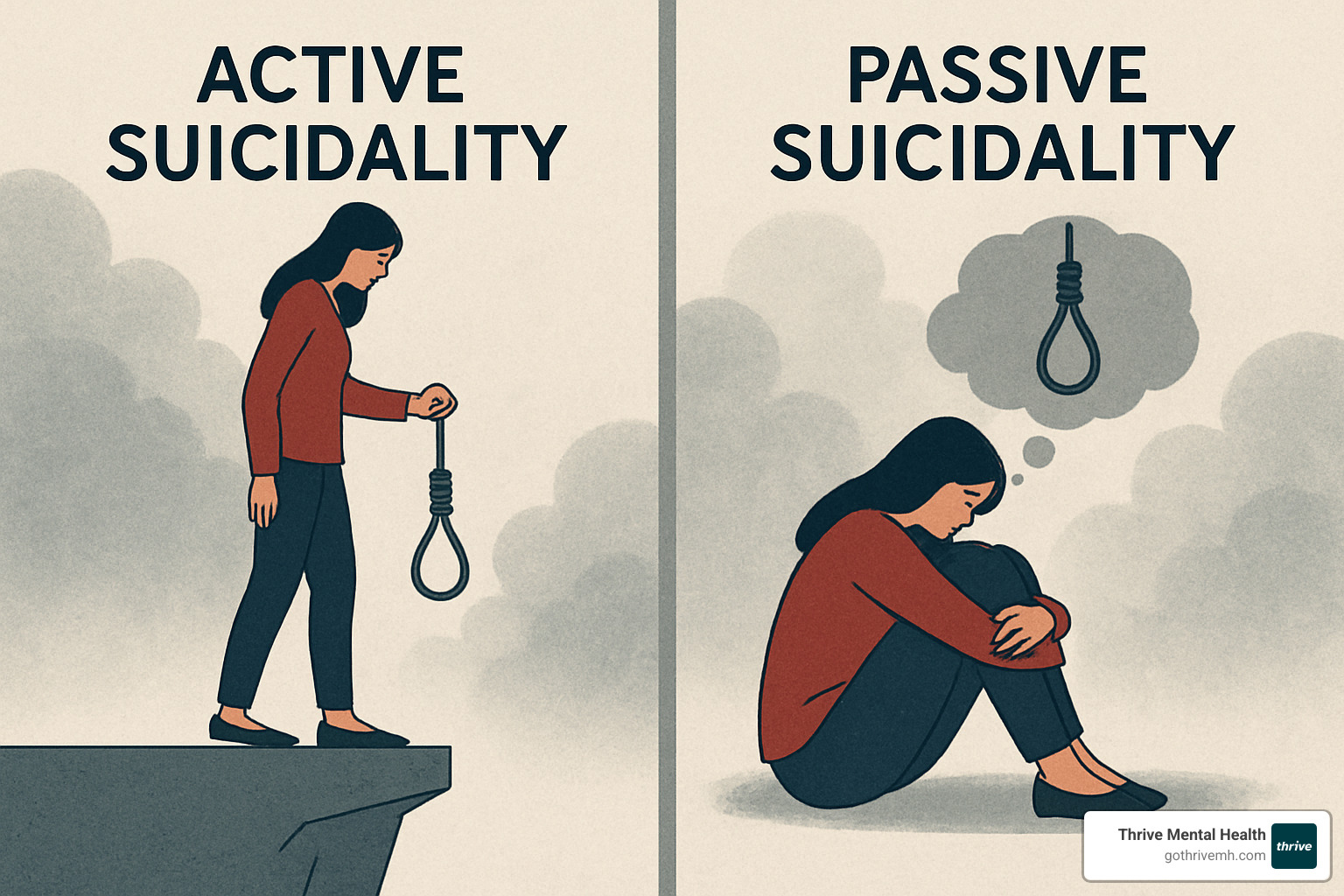
Active vs passive suicidality refers to two distinct types of suicidal thinking that differ primarily in intent and planning:
| Type | Definition | Risk Level | Warning Signs |
|---|---|---|---|
| Passive Suicidality | Thoughts about death without specific plans (e.g., “I wish I wouldn’t wake up tomorrow”) | Lower immediate risk but still serious | Expressions of hopelessness, withdrawal, sleep changes |
| Active Suicidality | Thoughts about suicide with concrete plans and intent (e.g., researching methods, collecting means) | Higher immediate risk requiring emergency intervention | Giving away possessions, acquiring lethal means, talking explicitly about methods |
Suicidal thoughts exist on a spectrum, and understanding the difference between passive and active suicidal ideation is crucial for proper assessment and intervention. While passive thoughts involve a desire to die without specific plans to act, active thoughts include both the desire and concrete planning. Both forms require attention and support, though active suicidality typically demands more urgent intervention.
“Most people assume that saying you’re suicidal means you’ll act on it immediately—but they’re wrong,” notes one individual with lived experience. This common misconception can prevent people from seeking help or talking openly about their struggles.
It’s important to recognize that passive suicidal thoughts, while representing lower immediate danger, should never be dismissed or minimized. Research shows that passive ideation can progress to active ideation under certain circumstances, and both forms are associated with increased risk of suicide attempts.
I’m Nate Raine, CEO of Thrive Mental Health, where our team has extensive experience helping clients steer the complex terrain of active vs passive suicidality through evidence-based approaches that emphasize safety, support, and recovery. My work in behavioral health has focused on creating accessible pathways to care for those experiencing suicidal thoughts of any intensity.

Suicidal Ideation 101: Definitions, Spectrum & Prevalence
When we talk about suicidal ideation, we’re referring to thoughts about ending one’s life—a mental experience that ranges from fleeting considerations to detailed planning. These thoughts aren’t binary but exist on a complex spectrum that affects millions of Americans each year.
Think of suicidal thoughts like an iceberg. What we typically see in statistics—completed suicides—represents only the visible tip. Beneath the surface lies a much larger reality: countless individuals experiencing various intensities of suicidal thinking, from vague wishes to concrete plans.

The numbers from the CDC tell a sobering story about our nation’s mental health. In 2021 alone, approximately 12.3 million adults reported serious thoughts of suicide. Of those, about 3.5 million made a plan, 1.7 million attempted suicide, and tragically, over 48,000 people died by suicide.
These statistics might seem abstract, but they represent real people—our neighbors, colleagues, friends, and family members. Research shows that suicidal thoughts are more common than many realize, with studies finding that 36.5% of adults have experienced suicidal ideation at some point in their lives, and 13.9% reported such thoughts within just the past month.
Mental health professionals use “ideation-to-action” frameworks to understand how and why some people move from thinking about suicide to attempting it. These models help identify distinct processes that contribute to developing thoughts versus acting on them—a crucial distinction in prevention efforts.
Passive Thoughts at a Glance
Passive suicidal ideation involves a wish to die without specific plans to make it happen. You might recognize it in statements like “I wish I could just go to sleep and never wake up” or “Sometimes I think everyone would be better off without me.”
People experiencing passive thoughts often describe a profound sense of hopelessness—feeling that life lacks meaning or purpose. They may not actively plan to harm themselves, but they wouldn’t mind if life somehow ended. These thoughts reflect significant emotional pain that deserves compassionate attention.
What surprises many is how common these experiences are, especially among those struggling with depression, anxiety disorders, or chronic health conditions. The suffering is real and substantial, affecting quality of life and daily functioning.
Passive thoughts, while representing lower immediate danger than active planning, should never be dismissed as “just thoughts” or considered normal. They’re meaningful signals that someone needs support—windows into genuine psychological distress.
Active Thoughts at a Glance
When passive thoughts evolve into active suicidal ideation, the risk level changes significantly. Active thoughts include specific intent and concrete planning—not just wishing to die, but developing a method to make it happen.
Active suicidal thoughts typically involve:
* Concrete plans for ending one’s life
* Intent to act on these plans
* Preparations like gathering means or putting affairs in order
* Setting a time or choosing a location
The warning signs of active suicidal thinking can be subtle or obvious: someone might start giving away valued possessions, making unexpected amends, putting financial affairs in order, or researching methods online. Sometimes, paradoxically, a person might appear suddenly calm after a period of distress—potentially signaling they’ve made a decision that gives them a sense of relief.
Research consistently shows that restricting access to lethal means is one of our most effective prevention strategies. When someone experiences active suicidal thoughts and has easy access to methods like firearms or large quantities of medication, the risk increases substantially.
Understanding the difference between active vs passive suicidality isn’t just academic—it saves lives by helping us recognize when and how to intervene. Both require compassionate response, but active thoughts often necessitate immediate professional intervention.
For more comprehensive information about suicide statistics and prevention, the CDC’s suicide facts page provides valuable resources and insights based on the latest research.
Active vs Passive Suicidality: Recognizing Key Differences
Understanding the difference between active vs passive suicidality isn’t just academic—it can literally save lives. While both types involve thoughts about death, they differ in crucial ways that affect how we respond and provide support.
Think of suicidal thoughts as existing on a continuum rather than in separate boxes. Research shows that passive thoughts can sometimes evolve into active ones, especially during times of increased stress, after drinking alcohol or using substances, or when mental health symptoms worsen.
What really sets active vs passive suicidality apart are five key elements:
First, there’s intent. Passive thoughts involve wishing you were dead without planning to make it happen, while active thoughts include a clear intention to end your life. It’s the difference between “I wish I could just not exist” and “I’m going to end my life.”
Second is planning. Someone with active thoughts has specific methods in mind—they’ve thought about how, when, and where. Passive thoughts lack this concrete planning element.
Third, look at behavior. Active suicidal thoughts often lead to preparation—gathering pills, purchasing a weapon, or giving away cherished possessions. With passive thoughts, you typically don’t see these action steps.
Fourth is the immediacy of risk. Active suicidal ideation generally represents a more urgent danger requiring emergency intervention, while passive thoughts, though serious, may not pose the same immediate threat.
Finally, the language people use offers important clues. Passive thoughts tend to be expressed more indirectly, while active thoughts are often more explicit and detailed.

Active vs Passive Suicidality in Real-World Language
The way someone talks about their dark thoughts can tell us a lot about what they’re experiencing and what kind of help they might need.
When someone is experiencing passive suicidal thoughts, you might hear phrases like “I just don’t want to wake up tomorrow” or “I wish I could disappear.” They might wonder aloud “What’s the point of living?” or say something like “Sometimes I think everyone would be better off without me.” These statements reflect suffering but don’t indicate immediate planning.
In contrast, active suicidal ideation sounds more direct and specific. Someone might say, “I can’t take it anymore and I know exactly how I’m going to end it” or “I’ve been researching ways to overdose.” They might mention writing goodbye letters or talk about collecting pills “for when I’m ready.” These statements signal both intent and planning—a dangerous combination requiring immediate intervention.
Social media can also provide windows into someone’s mental state. Posts expressing hopelessness or feeling like a burden may signal passive thoughts, while more direct statements about suicide methods or posting what seems like final goodbyes could indicate active suicidal ideation.
Not everyone will state their thoughts clearly, though. Watch for behavioral changes like withdrawal from friends and activities, increased substance use, or a sudden sense of calm after a period of visible distress—this last sign can sometimes mean someone has made a decision and feels relief.
Assessing Active vs Passive Suicidality Clinically
Mental health professionals don’t rely on guesswork when evaluating suicide risk. Instead, they use structured, evidence-based assessment tools to distinguish between passive and active suicidal thoughts and determine appropriate next steps.
The Columbia-Suicide Severity Rating Scale (C-SSRS) stands as one of the most widely used and validated tools for assessing suicide risk. It methodically evaluates several factors: whether suicidal thoughts are present, how intense these thoughts are, if there’s intent to act, whether a specific plan exists, any preparatory behaviors, and past suicide attempts.
What makes the C-SSRS particularly valuable is how clearly it differentiates between passive and active thoughts. It specifically distinguishes between having a “wish to be dead” (passive) and experiencing “active suicidal thoughts with method and intent” (active).
Other common assessment tools include the PHQ-9, which contains a specific question about thoughts of death or self-harm; the SIDAS (Suicidal Ideation Attributes Scale), which measures factors like frequency and controllability of suicidal thoughts; and the Beck Scale for Suicide Ideation, which explores various dimensions of suicidal thinking.
These assessments help clinicians make critical decisions about the appropriate level of care—from outpatient therapy for someone with passive thoughts to immediate hospitalization for someone with active thoughts, a plan, and intent.
At Thrive Mental Health, we use comprehensive, evidence-based assessments to evaluate both passive and active suicidal thoughts. This thorough approach allows us to create personalized treatment plans that address each client’s specific needs and level of risk. Our goal is always to meet you where you are and provide the right level of support when you need it most.
Risk, Progression & Underlying Theories
When we talk about suicidal thoughts, understanding what factors contribute to them—and how passive thoughts might progress to active ones—is crucial for effective prevention and support.
Several evidence-based theories help us make sense of how suicidal thoughts develop and potentially escalate:
The Interpersonal Theory of Suicide (IPTS) suggests that suicidal desire emerges from two painful experiences: feeling like a burden to others and feeling disconnected from supportive relationships. What’s important to understand is that this theory separates the desire for suicide from the capability to attempt it—the latter develops through repeated exposure to painful or frightening experiences.
The Three-Step Theory (3ST) offers a slightly different perspective, proposing that suicidal thoughts develop when pain and hopelessness combine. The progression to attempts requires developing the capability for suicide—essentially overcoming our natural survival instinct.
Fluid Vulnerability Theory reminds us that suicide risk isn’t static—it ebbs and flows over time as background vulnerabilities interact with current stressors in our lives.

Research has identified several key risk factors that increase vulnerability to both active vs passive suicidality:
Mental health conditions play a significant role, with depression present in approximately 60% of suicide cases. Other conditions like bipolar disorder, anxiety disorders, PTSD, borderline personality disorder, and schizophrenia also increase risk substantially.
Substance use significantly amplifies suicide risk in two ways: substances can increase impulsivity while lowering inhibitions, creating a dangerous combination. Studies show that about 22% of deaths by suicide involve alcohol intoxication.
Trauma and adverse experiences leave lasting imprints that can increase vulnerability. Childhood abuse, sexual assault, domestic violence, combat exposure, and prolonged stress all create pathways that can lead to suicidal thinking.
When we look at demographic and social factors, prior suicide attempts stand out as the strongest single risk factor. Family history of suicide, social isolation, major life transitions, access to lethal means, and exposure to suicide (including through media) also contribute significantly to risk.
The journey from passive to active suicidal ideation isn’t inevitable, but it can happen when emotional pain intensifies without relief, coping resources become depleted, hopelessness deepens, or acute stressors overwhelm existing coping mechanisms.
Fortunately, there are protective factors that can interrupt this progression. Strong social connections, effective coping skills, access to mental health care, cultural or religious beliefs that discourage suicide, restricted access to lethal means, and having a sense of purpose all help build resilience against suicidal thoughts.
At Thrive Mental Health, we focus on strengthening these protective factors while addressing risk factors through our comprehensive treatment programs. We recognize that understanding the complex interplay between risk factors, protective factors, and personal vulnerabilities is essential to creating effective, individualized care plans for those experiencing suicidal thoughts of any intensity.
Assessment, Intervention & Resources
When someone experiences suicidal thoughts—whether passive or active—appropriate assessment and intervention are crucial. The approach may differ based on the nature and severity of the thoughts, but all suicidal ideation warrants attention and support.
Professional Assessment
A thorough professional evaluation typically includes:
- Comprehensive suicide risk assessment using validated tools like the C-SSRS
- Mental status examination to evaluate mood, thought content, and cognitive functioning
- Exploration of risk and protective factors
- Assessment of immediate safety needs
- Evaluation of co-occurring conditions (depression, substance use, etc.)
Based on this assessment, a mental health professional can determine the appropriate level of care:
- Outpatient treatment: Often suitable for passive suicidal ideation without immediate risk
- Intensive outpatient programs (IOP): For moderate risk requiring more support than traditional outpatient care
- Partial hospitalization programs (PHP): For higher risk requiring daily structured treatment
- Inpatient hospitalization: For active suicidal ideation with plan and intent
Evidence-Based Interventions
Several evidence-based approaches have proven effective in treating suicidal thoughts:
Cognitive Behavioral Therapy (CBT): Helps identify and modify negative thought patterns and develop healthier coping strategies.
Dialectical Behavior Therapy (DBT): Particularly effective for suicidal thoughts, DBT combines acceptance and change strategies, teaching skills in four key areas:
* Mindfulness
* Distress tolerance
* Emotion regulation
* Interpersonal effectiveness
Collaborative Assessment and Management of Suicidality (CAMS): A therapeutic framework specifically designed for suicidal individuals.
Safety Planning: Developing a written plan that includes:
* Warning signs that a crisis may be developing
* Internal coping strategies
* People and social settings that provide distraction
* People to ask for help
* Professionals or agencies to contact during a crisis
* Making the environment safe (means restriction)
Medication: Psychiatric medications may help address underlying conditions like depression or anxiety.
Crisis Response
For active suicidal ideation with plan and intent, immediate crisis intervention is necessary:
- Call the 988 Suicide and Crisis Lifeline (available 24/7)
- Text “HOME” to the Crisis Text Line at 741741
- Go to the nearest emergency room
- Call 911
These resources provide immediate support and can help connect individuals with appropriate care.
The Role of Family and Loved Ones
Family members and friends play a crucial role in supporting someone with suicidal thoughts:
- Maintain open, non-judgmental communication
- Take all talk of suicide seriously
- Help secure the environment by removing potential means of self-harm
- Assist in accessing professional help
- Follow up consistently and show ongoing support
- Learn about warning signs and risk factors
- Take care of their own mental health
At Thrive Mental Health, we involve family members (with client consent) in treatment planning and provide education about supporting loved ones with suicidal thoughts.
Self-Help & Loved-Ones’ Action Steps
If you’re experiencing suicidal thoughts yourself:
- Reach out immediately: Tell someone you trust or contact a crisis resource
- Create distance from means: Remove or secure items that could be used for self-harm
- Implement coping strategies: Use techniques that have helped in the past
- Focus on getting through the moment: Suicidal crises are often temporary
- Practice self-care: Attend to basic needs like sleep, nutrition, and physical activity
- Seek professional help: Connect with a mental health provider
If you’re concerned about someone else:
- Ask directly: “Are you thinking about suicide?” Research shows this does not increase risk
- Listen without judgment: Allow them to express their feelings openly
- Determine if thoughts are passive or active: Ask if they have a plan or intent
- Stay with them if they’re at immediate risk
- Help them secure their environment: Remove access to lethal means
- Assist them in getting professional help: Offer to make calls or accompany them
- Follow up consistently: Show ongoing support and check in regularly
Crisis Resources List:
* 988 Suicide and Crisis Lifeline: Call or text 988
* Crisis Text Line: Text HOME to 741741
* Veterans Crisis Line: Call 988, then press 1
* Trevor Project (LGBTQ+ youth): Call 1-866-488-7386 or text START to 678678
* Local emergency services: 911
* Nearest emergency room

At Thrive Mental Health, we offer specialized programs for individuals experiencing suicidal thoughts. Our understanding of passive suicidal ideation and effective strategies for managing trauma and its triggers inform our comprehensive approach to treatment.
Conclusion
Understanding the distinction between active vs passive suicidality isn’t just academic—it’s literally life-saving. While passive thoughts involve wishes to die without specific plans, active suicidal thoughts include concrete intent and planning that demand immediate intervention.
Both forms deserve our full attention and compassionate care. The research is clear: suicidal thoughts—whether passive or active—signal significant psychological distress that should never be dismissed as “just a phase” or “looking for attention.”
Throughout this article, we’ve explored how suicidal thoughts exist on a spectrum, with passive ideation sometimes progressing to active thoughts under certain circumstances. We’ve seen how professional assessment plays a crucial role in determining the right level of support, and how evidence-based treatments like CBT and DBT can make a real difference in recovery.
Perhaps most importantly, we’ve emphasized that no one needs to face these struggles alone. Crisis resources are available 24/7, ready to provide immediate support when darkness feels overwhelming. Both professional intervention and the support of caring friends and family create the safety net that catches people when they’re falling.
At Thrive Mental Health, we see the person behind the pain. Our flexible, evidence-based care through virtual and in-person Intensive Outpatient Programs (IOP) and Partial Hospitalization Programs (PHP) serves Tampa Bay, St. Petersburg, and throughout Central Florida. Our team specializes in addressing suicidal thoughts through treatment plans as unique as you are—combining therapy, practical skill-building, and unwavering support.
We know that reaching out takes tremendous courage, especially when your mind is telling you there’s no hope. Our approach creates a safe harbor where healing can begin.

If you or someone you love is experiencing suicidal thoughts of any kind, please reach out today. Recovery isn’t just possible—it happens every day in our programs. Effective treatment can help quiet suicidal thoughts while building the resilience needed for lasting wellness.
For more information about our evidence-based depression programs and how we can walk alongside you on your journey toward healing, contact Thrive Mental Health today.
Remember: You are not alone. Your thoughts do not define you. And with proper support and treatment, there is always reason to hope for a brighter tomorrow.