Care with Compassion – Understanding Trauma-Informed Care

What is Trauma-Informed Care? [The Shift That Changes Everything]
What is trauma informed care is a question more people are asking as they search for mental health support that truly understands their experiences. Here’s what you need to know:
Trauma-Informed Care (TIC) is an approach that:
- Recognizes that trauma is widespread and affects how people respond to care
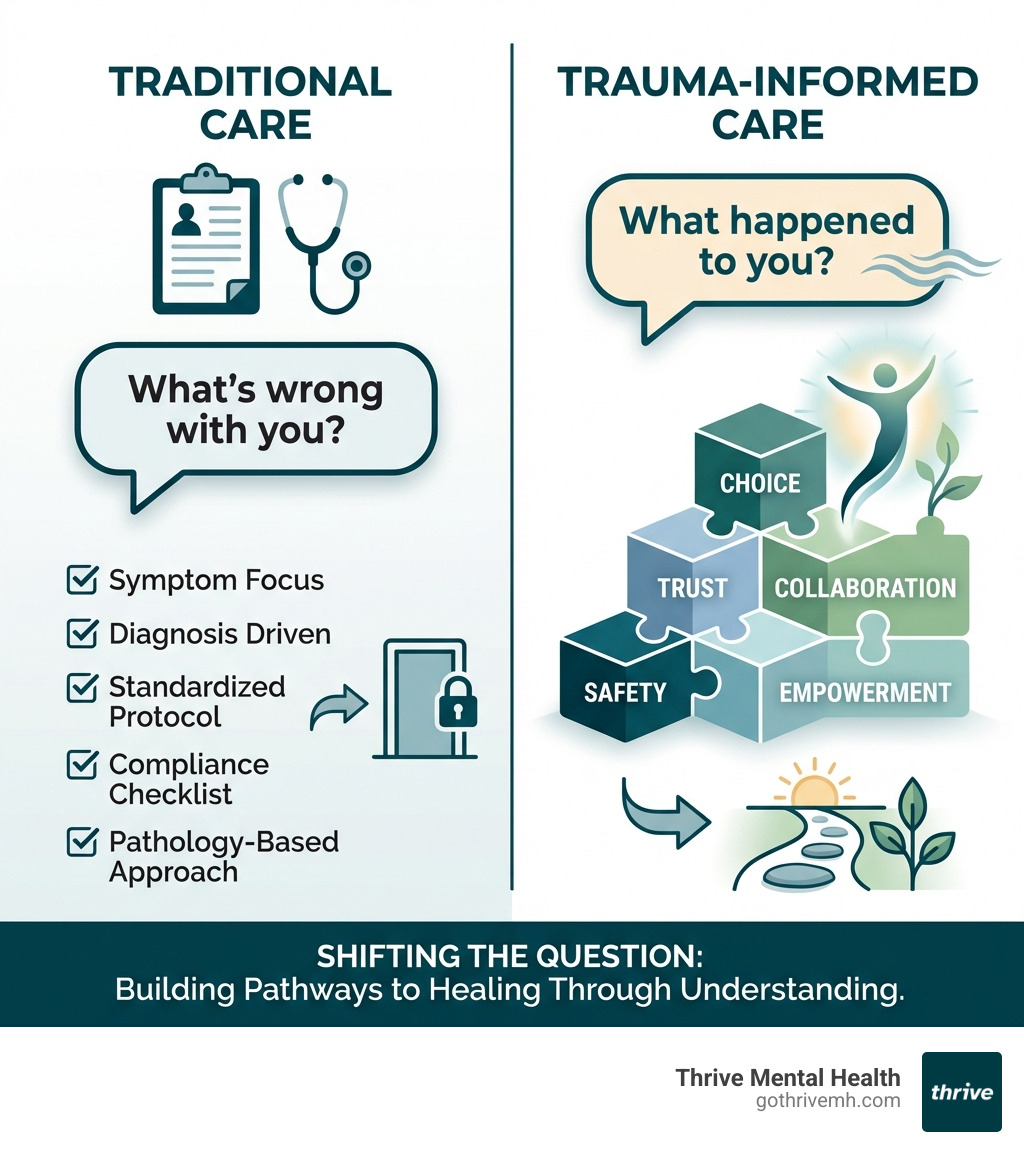
- Shifts the question from “What’s wrong with you?” to “What happened to you?”
- Creates safe environments that avoid re-traumatizing individuals
- Empowers recovery through principles like safety, trust, collaboration, and choice
- Benefits everyone—not just those with diagnosed trauma
Trauma isn’t limited to catastrophic events. It can be anything that overwhelms a person’s capacity to cope—from childhood neglect to systemic discrimination to intimate partner violence. Globally, 1 in 3 women have experienced physical or sexual violence. In Canada, 32% of adults report childhood abuse. These aren’t rare experiences—they’re woven into the fabric of our communities.
Traditional care often focuses on symptoms and diagnoses. Trauma-informed care asks a different question entirely. Instead of labeling behavior as “difficult” or “non-compliant,” it asks: What has this person survived? How are they trying to protect themselves? This paradigm shift changes everything—from the way intake forms are designed to how providers respond when someone misses an appointment.
The consequences of getting this wrong are serious. Re-traumatization doesn’t just cause additional harm—it leads to less engagement in services, higher rates of self-harm, staff burnout, and people giving up on getting help altogether. But when organizations accept trauma-informed principles, outcomes improve dramatically for both clients and staff.
I’m Nate Raine, CEO of Thrive Mental Health, and throughout my career leading behavioral health innovation and evidence-based treatment programs, I’ve seen how understanding what is trauma informed care transforms lives by creating the safety and trust people need to heal. At Thrive, we’ve built our entire approach—from our virtual IOP programs to our in-person services across Florida—on these foundational principles.
Quick look at what is trauma informed care:
What is Trauma-Informed Care? [A Fundamental Shift in Healing]
At its core, what is trauma informed care is an organizational change process that requires all individuals, practices, protocols, and environments to engage in universal precaution for trauma. Think of it like this: just as healthcare professionals wear gloves as universal precautions for pathogens, a trauma-informed approach means putting on metaphorical gloves by changing interactions, policies, and environments to prevent the possibility of re-traumatization. We understand that trauma is pervasive, and we work to integrate this knowledge into every aspect of our functioning.
This isn’t just a clinical technique; it’s a fundamental shift in perspective. It moves away from asking “What’s wrong with you?” to “What happened to you?” This paradigm recognizes that behaviors are often adaptive responses to traumatic experiences, not inherent flaws. Our goal is not necessarily to “treat” trauma in every interaction, but to minimize harm and create an environment where healing can naturally unfold. For a deeper dive, you can explore our More info on understanding trauma.
The Substance Abuse and Mental Health Services Administration (SAMHSA) outlines a clear framework for a trauma-informed approach, often summarized as the “Four R’s”:
- Realize: We realize the widespread impact of trauma and understand potential paths for recovery.
- Recognize: We recognize the signs and symptoms of trauma in clients, families, staff, and others involved with the system.
- Respond: We respond by integrating knowledge about trauma into policies, procedures, and practices.
- Resist Re-traumatization: We actively resist re-traumatization of clients and staff.
This comprehensive approach is why becoming a trauma-informed organization is best equated to a journey rather than a destination. It typically takes a minimum of three to five years for organizations to embed these values and principles into all aspects of functioning, reflecting a deep, continuous commitment to fostering healing and growth.
How Trauma-Informed Care Prevents Re-traumatization
One of the most crucial aspects of what is trauma informed care is its explicit aim to prevent re-traumatization. Re-traumatization refers to any procedure, interaction, situation, or environment that literally or symbolically replicates someone’s history of trauma, activating the body’s survival response and associated emotions, body responses, and cognitions.
This can happen through obvious practices, like the use of restraints or isolation, but also through less obvious triggers. Imagine a specific smell, a loud sound, or even an interaction that replicates themes like being unseen, unheard, or experiencing a lack of transparency. For someone with a history of trauma, these seemingly innocuous elements can activate a powerful, involuntary survival response.
When re-traumatization occurs, it doesn’t just cause additional harm; it has far-reaching negative consequences. It’s associated with less engagement in services, higher rates of self-harm and injury in individuals receiving services, staff turnover, lower staff morale, and reduced organizational commitment. This is why we, at Thrive Mental Health, prioritize creating an environment free from such triggers, ensuring that our therapeutic settings in Florida are places of safety and trust.
The Critical Role of Systemic and Historical Trauma
Understanding what is trauma informed care also requires us to consider the profound impact of historical, racial, and systemic trauma. Trauma is not just an individual experience; it can be transmitted across generations and inflicted by societal structures. This includes:
- Racial Trauma: The cumulative stress and psychological harm resulting from experiences of racism, discrimination, and systemic oppression.
- Intergenerational Trauma: The passing down of trauma responses and effects from one generation to the next, even if direct exposure to the original traumatic event didn’t occur.
- Systemic Violence: Practices and policies within systems (like healthcare, justice, or education) that perpetuate harm, exclusion, or discrimination, such as exclusionary practices, lack of cultural considerations, microaggressions, and non-inclusive language.
Individuals from groups with historical, racial, and systemic trauma can be re-traumatized by these factors. For example, Transgender people experience much higher rates of domestic and community violence than the general population and face extensive barriers to service. A truly trauma-informed approach must center considerations of diversity, equity, inclusion, accessibility, and justice (DEIAJ) when applying its values and principles.
This means we actively work to create cultural safety—an environment where individuals feel safe and respected, and where their cultural identities, values, and experiences are acknowledged and affirmed. This involves addressing unconscious biases, educating our staff on culturally responsive practices, and ensuring our services are accessible and welcoming to all individuals, regardless of their background.

The 6 Core Principles That Make Care Truly Trauma-Informed
The Substance Abuse and Mental Health Services Administration (SAMHSA) has identified six key principles that guide a trauma-informed approach. These principles form the bedrock of our practice at Thrive Mental Health, promoting resilience, fostering healing, and supporting growth for every individual we serve.
Here are the 6 core principles:
- Safety
- Trustworthiness and Transparency
- Peer Support
- Collaboration and Mutuality
- Empowerment, Voice, and Choice
- Cultural, Historical, and Gender Issues
Let’s explore each of these in more detail.
1. Safety: Creating a Secure Foundation
Safety is the absolute cornerstone of what is trauma informed care. Without a foundational sense of security, true healing cannot begin. This principle extends beyond mere physical safety to encompass psychological and emotional well-being. We strive to create environments in our virtual and in-person programs that feel welcoming, predictable, and non-threatening. This means:
- Physical Safety: Ensuring our physical spaces are calm, clean, and free from perceived threats.
- Psychological Safety: Fostering an atmosphere where individuals feel safe to express themselves without fear of judgment, ridicule, or invalidation.
- Emotional Safety: Providing consistent expectations, clear boundaries, and predictable interactions to reduce anxiety and promote a sense of control.
Our goal is for every client to feel safe enough to engage in the vulnerable work of healing, knowing they are in a protected and supportive space.
2. Trustworthiness and Transparency: Building Authentic Connections
Trust is often deeply fractured by trauma, making trustworthiness and transparency vital in trauma-informed care. We build authentic connections by being open, honest, and consistent in all our interactions. This involves:
- Clear Communication: Explaining processes, expectations, and therapeutic approaches in an understandable way.
- Openness: Being transparent about our roles, intentions, and any limitations.
- Consistency: Following through on commitments and maintaining predictable patterns of care.
- Honesty: Providing truthful information, even when it’s difficult, in a compassionate manner.
By consistently demonstrating trustworthiness, we help clients rebuild their capacity for healthy relationships and engage more fully in their recovery journey.
3. Peer Support: The Power of Lived Experience
The principle of peer support recognizes the profound healing power of shared experience. Connecting with others who have steerd similar challenges can be incredibly validating and empowering. In our programs, we integrate peer support to:
- Foster Shared Understanding: Creating spaces where individuals feel understood and less alone.
- Normalize Experiences: Helping clients realize that their reactions to trauma are common and understandable.
- Instill Hope: Demonstrating that recovery is possible through the lived experience of others.
- Reduce Isolation: Counteracting the isolating effects of trauma by building community.
Peer support is a powerful component, offering a unique blend of empathy and practical guidance. It helps individuals see a path forward and reinforces the idea that they are not defined by their past. For more on overcoming past experiences, see our article on overcoming PTSD.
4. Collaboration and Mutuality: Healing Together
Trauma often involves experiences where control was taken away. Therefore, collaboration and mutuality are essential principles in trauma-informed care. This means actively partnering with clients in their healing journey, rather than dictating it. We practice:
- Power-Sharing: Recognizing and actively working to reduce inherent power differentials between providers and clients.
- Joint Decision-Making: Involving clients in setting goals, choosing interventions, and making decisions about their care.
- Valuing Client Input: Respecting and integrating client perspectives, preferences, and strengths into treatment plans.
Our approach is about working with clients, ensuring they are active participants in their recovery, fostering a sense of shared responsibility and respect.
5. Empowerment, Voice, and Choice: Restoring Control
Empowerment, voice, and choice are critical for restoring a sense of agency that trauma often diminishes. We actively create opportunities for clients to regain control over their lives and their healing process by:
- Providing Options: Offering choices in treatment modalities, scheduling, and participation.
- Respecting Autonomy: Honoring clients’ decisions and self-determination, even if they differ from what we might initially recommend.
- Building on Strengths: Identifying and leveraging clients’ inherent strengths and resiliencies.
- Validating Client’s Voice: Ensuring clients feel heard, respected, and that their perspectives matter.
- Fostering Self-Advocacy Skills: Supporting clients in developing the ability to speak up for their needs and preferences.
By emphasizing these elements, we help clients rebuild confidence, make informed decisions, and actively shape their path to well-being.
6. Cultural, Historical, and Gender Issues: Acknowledging the Full Context
The sixth principle underscores the importance of acknowledging the complex interplay of cultural, historical, and gender issues in shaping an individual’s experience of trauma and their healing journey. We understand that trauma is not a monolithic experience, and its impact is deeply influenced by social context. This means:
- Cultural Sensitivity: Providing care that respects and integrates clients’ cultural backgrounds, beliefs, and practices.
- Gender-Responsive Care: Recognizing and addressing the unique ways gender influences trauma experiences, recovery needs, and access to services. For instance, while women and men experience emotional/psychological intimate partner violence at similar rates, men often face fear of ridicule and humiliation.
- Recognizing Stereotypes and Addressing Biases: Actively challenging and dismantling assumptions and prejudices that can hinder effective care.
- Creating Inclusive Services: Ensuring our programs are designed to be accessible and supportive for all diverse populations, including those who have experienced systemic oppression.
By integrating these considerations, we ensure that our care is not only clinically effective but also deeply respectful and relevant to each individual’s unique life context.
The Dual Payoff of Trauma-Informed Care [For Patients and Providers]

Adopting a trauma-informed approach is not merely a best practice; it’s a game-changer for everyone involved in the healing process. The benefits extend far beyond individual clients, creating a ripple effect that improves the entire care ecosystem. We see dual benefits: improved outcomes for patients and improved well-being for our dedicated providers and staff.
Consider the prevalence of trauma: Globally, 1 in 3 women experienced physical and/or sexual violence by a partner or sexual violence by a non-partner. In Canada, 32% of adults report that they experienced abuse in childhood. These statistics highlight the widespread need for care that understands the profound impact of such experiences. When care is trauma-informed, it fundamentally improves the quality of life for those seeking help in Florida, and creates a more sustainable, compassionate work environment for those providing it. This is why leading insurance providers like Cigna and Optum cover these evidence-based approaches.
Benefits for Patients: A Pathway to Real Recovery
For patients, a trauma-informed approach offers a pathway to real, lasting recovery by fostering an environment where they can truly heal. When we shift from “What’s wrong with you?” to “What happened to you?”, we create profound benefits:
- Increased Engagement in Services: Patients are more likely to participate and stay committed to treatment, like our accessible virtual IOP programs, when they feel safe, respected, and understood. This leads to better adherence and continuity of care.
- Better Long-Term Health Outcomes: By addressing the root causes and impacts of trauma, rather than just symptoms, patients experience more comprehensive healing, leading to improved mental, physical, and emotional health over time.
- Reduced Self-Harm and Injury: Preventing re-traumatization and providing empowering, collaborative care can significantly reduce the likelihood of self-harm and other maladaptive coping mechanisms.
- Stronger Patient-Provider Relationships: Trust, transparency, and collaboration build robust therapeutic alliances, making patients feel heard and validated. This fosters a sense of partnership in their healing journey.
- Feeling Heard and Validated: For many who have experienced trauma, their narratives have been dismissed or minimized. Trauma-informed care validates their experiences, empowering them to reclaim their story and agency.
These benefits collectively create a more effective and humane system of care, moving individuals toward genuine well-being.
Benefits for Providers and Staff: Preventing Burnout and Vicarious Trauma
The advantages of trauma-informed care aren’t limited to clients; they significantly impact the well-being of our dedicated healthcare providers and staff. Working with individuals who have experienced trauma can take a heavy toll, leading to what’s known as secondary trauma or compassion fatigue. A trauma-informed approach actively mitigates these risks, leading to:
- Reduced Staff Turnover: When staff feel supported, understood, and equipped to handle the emotional demands of their work, they are more likely to stay in their roles. Re-traumatization is associated with staff turnover, so reducing it benefits everyone.
- Higher Morale: A workplace culture that prioritizes the well-being of both clients and staff fosters a more positive and supportive environment, boosting morale and job satisfaction.
- Increased Job Satisfaction: Providers feel more effective and fulfilled when they can deliver care that truly makes a difference and when they feel supported in doing so.
- Addressing Secondary Trauma: Trauma-informed organizations recognize that secondary trauma is a normal occupational hazard. They implement strategies to address it, such as regular supervision, debriefing, and access to support resources.
- Promoting Staff Wellness and Self-Care: We actively encourage and provide resources for self-care, understanding that our providers can only offer compassionate care if their own well-being is prioritized. Organizations like Thrive Mental Health invest in strategies to improve wellness and address burnout, vicarious/indirect trauma, and compassion fatigue/empathic strain. We recognize that being trauma-informed is about the workforce as much as individuals receiving services. You can listen to professionals speak about self-care to understand its importance.
By caring for our caregivers, we create a stronger, more resilient team capable of providing the highest quality of care.
Building a Culture of Safety: How Organizations Implement Trauma-Informed Care
Implementing trauma-informed care is a comprehensive journey, not a quick fix. It requires deep organizational commitment and visible leadership investment to truly embed its principles into every facet of operations. As noted in the research, becoming a trauma-informed organization is best equated to a journey rather than a destination, and it typically takes a minimum of three to five years for organizations to embed trauma-informed values and principles into all aspects of functioning. This long-term commitment ensures a sustainable culture of safety and healing.
At Thrive Mental Health, we integrate SAMHSA’s official guidance for a Trauma-Informed Approach into our strategic planning and daily operations across our virtual and in-person centers in Florida. It’s about building a culture where every staff member, from administrative support to clinical leadership, understands and applies trauma-informed principles.
Key Steps for Implementation
For organizations committed to becoming trauma-informed, several key steps are essential:
- Oversight Committee: Establishing a dedicated committee or task force to guide the implementation process, ensuring accountability and consistent progress.
- Policy Review: Systematically reviewing and revising all organizational policies, procedures, and protocols through a trauma-informed lens to identify and eliminate potential re-traumatizing practices.
- Staff Training: Providing comprehensive, ongoing training for all staff members—not just clinicians—on trauma prevalence, its impact, and the principles of trauma-informed care. This includes training on cultural sensitivity and addressing microaggressions.
- Creating a Safe Physical Environment: Assessing and modifying physical spaces to promote a sense of safety, calm, and de-escalation for clients and staff. This could mean attention to lighting, noise levels, privacy, and welcoming decor.
- Including Client Voice: Actively involving individuals with lived experience in the planning, implementation, and evaluation of services to ensure they are genuinely client-centered and effective.
- Evaluation and Monitoring: Regularly evaluating the effectiveness of trauma-informed initiatives and monitoring progress, using feedback from both staff and clients to continuously improve.
What does a trauma-informed organization look like in practice?
In a trauma-informed organization like Thrive Mental Health, these principles translate into tangible practices that improve care:
- Screening for Trauma: We incorporate universal routine screenings for trauma at intake, conducted sensitively and with an understanding of potential emotional responses. This helps us tailor care from the very beginning.
- Strengths-Based Planning: Our treatment plans focus on identifying and building upon each client’s unique strengths and resilience, fostering their capacity for coping and growth.
- Flexible Scheduling: Recognizing that life circumstances can be complex, especially for those managing trauma, we offer flexible scheduling, including virtual and evening options for our IOP and PHP programs. This makes care accessible across Florida.
- Accessible Care: We strive to make our evidence-based treatment accessible anywhere, anytime. This includes accepting major insurance providers like Cigna, Optum, Aetna, and Florida Blue, removing financial barriers to care.
- Client-Centered Environments: Our physical and virtual spaces are designed to be calming and respectful, prioritizing client comfort and choice. This is paramount, whether you’re joining us from your home via our virtual programs or at one of our in-person centers in Florida.
A trauma-informed organization is one that embodies compassion, understanding, and respect in every interaction, creating a true sanctuary for healing.
Frequently Asked Questions about Trauma-Informed Care
What is the main goal of trauma-informed care?
The primary goal is not to treat specific traumas but to create a safe, supportive environment that avoids re-traumatization and empowers individuals. It shifts the focus from “What’s wrong with you?” to “What happened to you?” to understand the full context of a person’s life and behaviors.
How is trauma-informed care different from trauma-specific treatment?
Trauma-informed care is a universal framework or approach that shapes an entire organization’s culture and practices. Trauma-specific treatment, like Complex PTSD Counselling, refers to targeted clinical interventions designed to directly address and resolve trauma symptoms. An organization can be trauma-informed without offering trauma-specific services, but any trauma-specific service should always be delivered within a trauma-informed framework.
Can anyone be trauma-informed?
Yes. While it’s often discussed in healthcare, any person or organization can adopt trauma-informed principles. This includes schools, workplaces, and community centers. It’s about recognizing the widespread impact of trauma and consciously choosing to interact with others in a way that promotes safety, trust, and empowerment.
What are the “universal precautions” in trauma-informed care?
Similar to medical universal precautions, trauma-informed universal precautions mean assuming that everyone you encounter may have a history of trauma. This leads to proactively designing all interactions, policies, and environments to prevent re-traumatization, fostering safety, trustworthiness, and choice for all, regardless of their known trauma history.
Take the First Step: Find Trauma-Informed Care That Works
What is trauma informed care is more than just a buzzword; it’s a profound and necessary shift in how we approach healing. It creates environments where healing is not just possible, but prioritized, acknowledging the courage it takes to seek help and meeting that courage with safety, respect, and collaboration. By focusing on “what happened” instead of “what’s wrong,” providers at organizations like Thrive Mental Health can build the trust needed for true recovery. We are committed to making evidence-based treatment accessible and effective, ensuring every individual feels seen, heard, and supported on their journey to well-being.
Ready for support? Thrive offers virtual and hybrid IOP/PHP programs with evening options. Verify your insurance in 2 minutes (no obligation) → Start benefits check or call 561-203-6085. If you’re in crisis, call/text 988.