Growing Pains: Understanding the Impact of Childhood Trauma

Childhood Trauma: 3 Ways to Heal & Thrive
Childhood Trauma [2025]: 5 Proven Treatments, Insurance Coverage, and How to Start This Week
If you’re in crisis, call/text 988 right now. You are not alone.
Summary: Childhood trauma affects 61% of adults. This guide shows you 5 evidence-based treatments, how to use insurance in Florida, and the fastest ways to start care this week.
Childhood trauma includes frightening or dangerous events that threaten a child’s safety, such as abuse, neglect, or household dysfunction. These adverse experiences can alter brain development, leading to lifelong health challenges.
Key facts about childhood trauma:
- 61% of adults had at least one Adverse Childhood Experience (ACE) before age 18.
- 17% experienced four or more types of traumatic events.
- Common types: physical/sexual abuse, emotional neglect, and witnessing violence.
- Long-term effects: increased risk for depression, anxiety, PTSD, and chronic diseases.
- Good news: The brain can heal with trauma-informed therapy.
When children face ongoing stress, their bodies enter survival mode. This toxic stress can rewire the brain, affecting learning, relationships, and health for decades. Research shows a clear link between adverse childhood experiences and adult struggles with anxiety, depression, substance use, and chronic conditions like heart disease.
But here’s what matters most: healing is possible. The brain’s plasticity allows for recovery and growth with the right support.
I’m Anna Green, LMHC, LPC, Chief Clinical Officer at Thrive Mental Health. I specialize in complex trauma using evidence-based therapies like EMDR. Through my work with childhood trauma survivors, I’ve seen the profound change that happens with proper care.
Explore more about childhood trauma:
What Counts as Childhood Trauma? Unpacking the Types and Causes
Childhood trauma is any experience that overwhelms a child’s ability to cope and threatens their sense of safety or well-being. Because their brains are still developing, children are highly vulnerable to events that an adult might find manageable.
SAMHSA’s “Three E’s” framework helps explain this: the Event, the child’s Experience of it as harmful, and the lasting Effects. This is why two children can react differently to similar situations.
Trauma can take many forms:
- Abuse: Physical (non-accidental injury), emotional (criticism, humiliation), or sexual (any sexual act involving a child).
- Neglect: Physical (failure to provide basic needs) or emotional (withholding love and support).
- Household Dysfunction: Growing up with parental substance abuse, mental illness, domestic violence, or an incarcerated family member. This turns the home into a source of fear.
- Other Traumas: Bullying, community violence, medical trauma, and systemic issues like poverty or racism create chronic stress and shatter a child’s sense of safety.
What matters most is the child’s perception of the event. A resilient child with strong support may weather an experience that deeply affects another. The National Child Traumatic Stress Network offers more information on these trauma types.
Understanding complex childhood trauma
When trauma is not a single event but a pattern of repeated experiences, it’s called Complex Trauma (C-PTSD). It often involves caregivers who should be sources of safety, creating profound confusion about relationships and self-worth.
Unlike a single incident, complex trauma becomes woven into a child’s identity and worldview. It affects everything: their ability to trust, regulate emotions, and form healthy relationships. The Facts for Caregivers on Complex Trauma resource provides deeper insights.
The role of Adverse Childhood Experiences (ACEs)
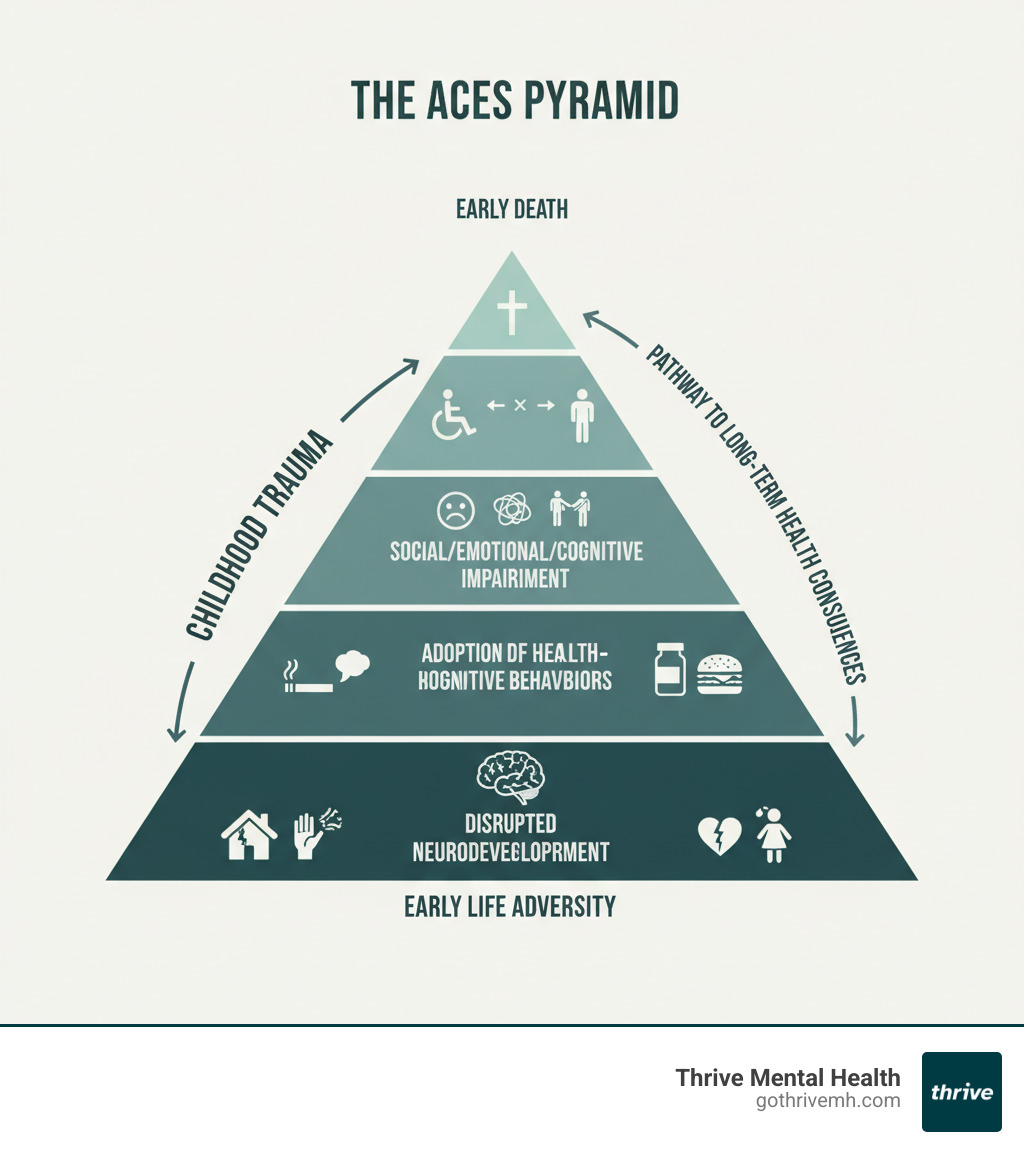
The CDC-Kaiser Permanente ACE Study revealed a powerful link between childhood adversity and adult health problems. The study identified ten types of ACEs, including abuse, neglect, and household dysfunction.
Researchers found a strong “dose-response relationship”: the more ACEs someone has, the higher their risk for physical and mental health issues. While 61% of adults have at least one ACE, and 17% have four or more, an ACE score is a risk factor, not a life sentence. Many people with high scores lead healthy lives, especially with proper support. The ACE framework helps identify those who need extra support and validates the lasting impact of childhood experiences. You can learn more about this influential research through the CDC’s information about the ACE Study.
The Ripple Effect: How Trauma Rewires a Child’s Brain and Body
When a child experiences childhood trauma, their developing brain changes how it processes the world. Harmful experiences can leave deep, lasting impressions on its moldable structure.
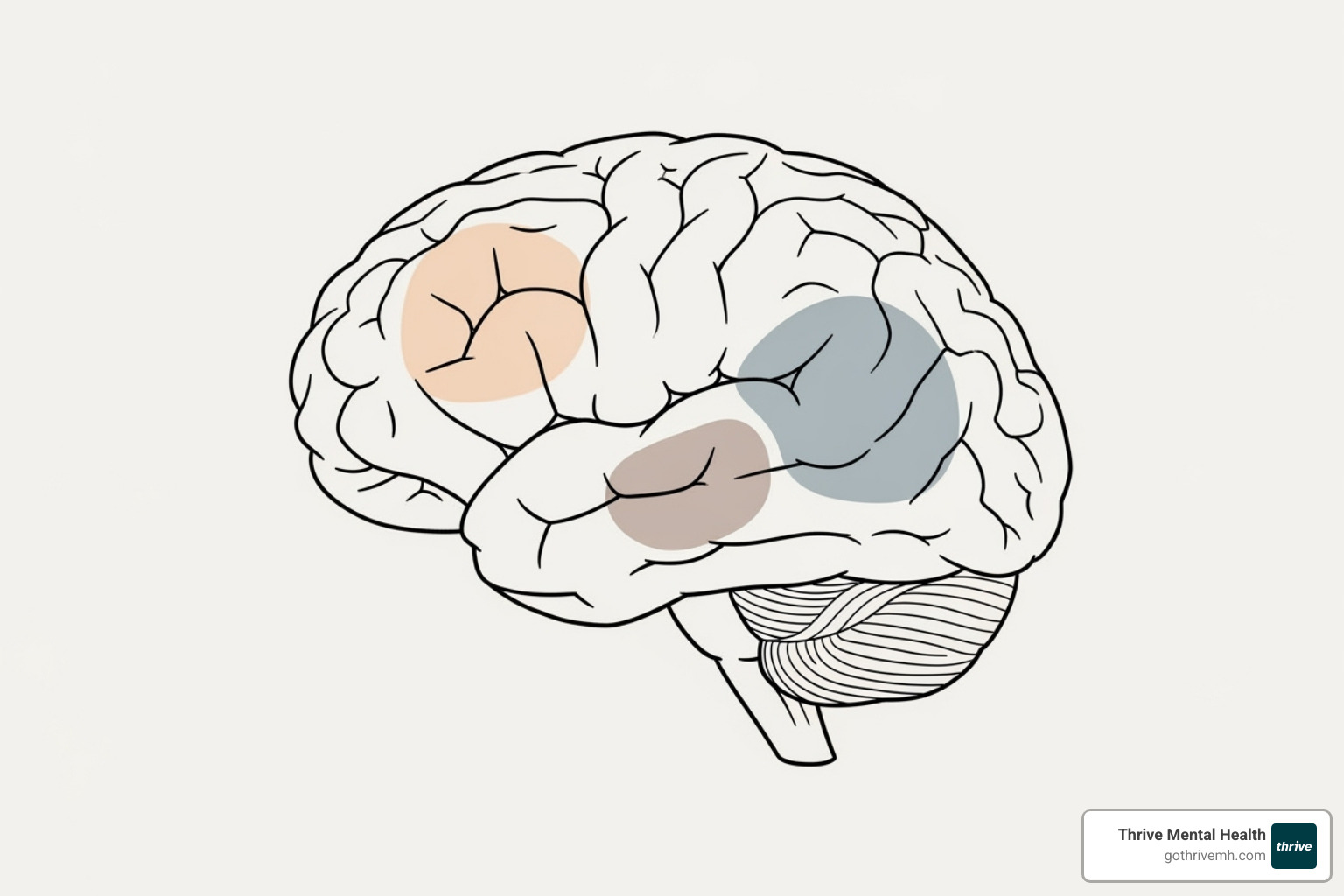
The brain’s alarm system—the fight-flight-freeze response—becomes hyperactive. The body’s stress response system (the HPA axis) floods the body with cortisol, the primary stress hormone. This constant state of alarm reshapes key brain areas:
- The amygdala (fear center) becomes overactive, leading to anxiety and hypervigilance.
- The hippocampus (memory and learning) can shrink, making it harder to concentrate.
- The prefrontal cortex (decision-making, impulse control) can be underdeveloped, causing struggles with emotional regulation.
These changes are not a sign of a child being difficult; their brain hasn’t had the safety needed to develop these skills. Research detailed in The biological effects of childhood trauma shows how these changes can persist without intervention.
Mental and emotional developmental impact
The emotional world of a traumatized child is often chaotic. They may experience emotional dysregulation, with feelings swinging from zero to ten instantly. Attachment issues can arise when caregivers are also sources of fear, leading to a confusing push-pull for connection. Children often internalize blame, leading to deep low self-esteem and shame. To cope, some may dissociate, or mentally “check out,” which can interfere with daily life. These struggles frequently lead to anxiety and depression.
Signs and symptoms in children and adolescents
Children often express trauma through their behavior. Recognizing these signs is key to getting them help.
- Infants and Toddlers: Feeding issues, excessive crying, and sleep disturbances.
- Preschoolers: Regression to earlier behaviors (like bedwetting), repetitive traumatic play, and intense separation anxiety.
- School-Age Children: Difficulty concentrating, declining grades, behavioral outbursts, social withdrawal, and physical complaints like headaches or stomachaches.
- Adolescents: Risk-taking behaviors (substance use, reckless driving), self-harm, eating disorders, and severe depression or anxiety.
These symptoms are often mislabeled as behavioral problems when they are actually normal responses to abnormal situations.
The Long Shadow: Adult Consequences of Unresolved Trauma
The impact of childhood trauma extends into adulthood, influencing health, relationships, and well-being. The body keeps the score, and a brain adapted for survival continues to operate on high alert even when the danger is gone.

Adults with a history of trauma face higher rates of chronic diseases like heart disease, diabetes, and autoimmune disorders. The chronic stress and inflammation take a physical toll, and studies show that high ACE scores are linked to premature mortality. You can read more about the Link between ACEs and chronic disease.
Mentally, unresolved childhood trauma is a major risk factor for conditions like Post-Traumatic Stress Disorder (PTSD), with its flashbacks and hypervigilance, and Borderline Personality Disorder (BPD), characterized by emotional instability and a fragmented sense of self. Depression, anxiety disorders, eating disorders, and higher rates of suicidal ideation and self-harm are also common.
The connection between childhood trauma and addiction
Substance use disorders are strongly linked to childhood trauma. The self-medication hypothesis suggests people use drugs or alcohol to numb emotional pain or quiet intrusive thoughts. What begins as a coping mechanism can quickly become an addiction. For many survivors, substances provide temporary relief from internal pain at a tremendous cost. If you or a loved one needs help, you can Find substance use and mental health treatment.
Impact on relationships and life skills
Childhood trauma shapes how adults steer relationships. When early connections involved pain or betrayal, forming healthy bonds is challenging.
- Fear of intimacy and difficulty trusting others are common.
- Survivors may unconsciously repeat unhealthy relationship patterns from their past.
- Vulnerability can feel dangerous, making deep connection difficult.
These struggles affect all areas of life, leading to career instability, financial difficulties, and lower educational attainment. Understanding these patterns is the first step toward healing and building the stable, healthy life you deserve.
The Path to Healing: Evidence-Based Therapies and Support
While the weight of childhood trauma is heavy, healing is possible. The brain’s plasticity creates pathways for recovery. Resilience can be built, and your experiences don’t have to define your future. The key is finding professional support that understands the complexity of trauma.
Effective therapeutic approaches for childhood trauma
Modern trauma therapy offers specific, evidence-based treatments that help the brain and body heal.
- Trauma-Focused Cognitive Behavioral Therapy (TF-CBT): Helps process memories safely while learning coping skills.
- Eye Movement Desensitization and Reprocessing (EMDR): Uses guided eye movements to help the brain reprocess trauma, reducing its emotional charge. Our clinicians at Thrive Mental Health specialize in EMDR therapy.
- Somatic Experiencing: Focuses on releasing trapped traumatic energy from the body.
- Dialectical Behavior Therapy (DBT): Teaches skills for managing overwhelming emotions and improving relationships.
- Internal Family Systems (IFS): A compassionate approach to healing different “parts” of yourself.
The National Child Traumatic Stress Network provides more information on these Trauma Treatments from NCTSN.
Finding the right level of care
Sometimes, weekly therapy isn’t enough for deep-rooted childhood trauma. If you’re struggling with daily functioning, more intensive support may be needed.
- Intensive Outpatient Programs (IOP): Provide structured treatment several days a week while you maintain your daily life.
- Partial Hospitalization Programs (PHP): Offer more comprehensive care, operating most of the day, several days a week.
These immersive programs provide the time, space, and peer support to dig deep and practice new skills. Thrive Mental Health’s virtual IOP and PHP programs offer flexible evening options, so you can access expert care without rearranging your life. Prefer fully online care? Explore our Virtual Therapy option.
Insurance and Accessibility in Florida
Cost should not be a barrier to healing. Most major insurance plans cover IOP and PHP programs for trauma treatment.
Thrive Mental Health accepts major insurers like Cigna, Optum, and Florida Blue in Florida. Whether you’re in Miami, Orlando, Tampa, or elsewhere in the state, our virtual programs make expert trauma care accessible. Our team will help you understand and maximize your benefits. You can verify your insurance coverage in 2 minutes with no obligation.
Building a Safety Net: How to Support Survivors

Recovery from childhood trauma flourishes with support. Whether you’re a parent, teacher, or friend, your role is vital. The foundation of support is trauma-informed care, an approach that acknowledges trauma’s impact and actively works to create safe environments.
This approach is guided by five principles: Safety, Trustworthiness, Peer Support, Collaboration, and Empowerment. The goal is to create relationships and spaces where survivors feel secure, heard, and in control of their healing journey.
For parents, caregivers, and educators
Your steady presence can be an anchor for someone who has experienced childhood trauma. This requires patience and consistency.
- Build trust: Show up, keep promises, and create predictable routines to provide stability.
- Co-regulate emotions: Your calm presence can help a child’s overwhelmed nervous system settle down.
- Listen actively: Validate their feelings without trying to fix them. A simple “That sounds really hard” can make a huge difference.
- Seek your own support: You can’t pour from an empty cup. Ensure you have your own support system.
For educators, understanding how trauma affects learning is crucial. A student’s defiance may actually be a survival response. The NCTSN’s Child Trauma Toolkit for Educators offers practical strategies.
Creating trauma-informed schools and communities
Effectively addressing childhood trauma requires a community-wide shift. Instead of asking, “What’s wrong with this child?” trauma-informed schools and communities ask, “What happened to this child?”
This involves implementing school policies that avoid re-traumatization, providing staff training on trauma, and creating community prevention programs that support families before a crisis occurs. By promoting protective factors like stable housing, quality education, and positive relationships, communities can become healing environments where children don’t just survive, but thrive.
Frequently Asked Questions about Childhood Trauma
Note for developers: Implement JSON-LD FAQ schema for this section. Suggested JSON-LD example is included below.
What are the 3 main types of trauma?
Acute (single event), chronic (repeated events), and complex (multiple, often relational traumas over time).
How do I know if childhood trauma is affecting me now?
Common signs include anxiety, depression, emotional swings, dissociation, relationship struggles, and health issues that don’t have a clear cause.
What is the fastest effective treatment for childhood trauma?
Evidence-based options like EMDR, TF-CBT, and DBT skills can reduce symptoms quickly for many people. The right fit depends on your history and goals.
Can you fully heal from childhood trauma?
Yes. You can process memories, regulate emotions, and build healthy relationships. Healing means the trauma no longer runs your life.
Does insurance cover trauma therapy in Florida?
Often yes. Thrive accepts Cigna, Optum, Florida Blue, and more. You can verify your benefits in 2 minutes.
Suggested JSON-LD (developers can adapt):
{
“@context”: “https://schema.org”,
“@type”: “FAQPage”,
“mainEntity”: [
{
“@type”: “Question”,
“name”: “What are the 3 main types of trauma?”,
“acceptedAnswer”: {“@type”: “Answer”, “text”: “Acute (single event), chronic (repeated events), and complex (multiple, often relational traumas over time).”}
},
{
“@type”: “Question”,
“name”: “How do I know if childhood trauma is affecting me now?”,
“acceptedAnswer”: {“@type”: “Answer”, “text”: “Common signs include anxiety, depression, emotional swings, dissociation, relationship struggles, and unclear health issues.”}
},
{
“@type”: “Question”,
“name”: “What is the fastest effective treatment for childhood trauma?”,
“acceptedAnswer”: {“@type”: “Answer”, “text”: “EMDR, TF-CBT, and DBT skills often reduce symptoms quickly. The best option depends on your history and goals.”}
},
{
“@type”: “Question”,
“name”: “Can you fully heal from childhood trauma?”,
“acceptedAnswer”: {“@type”: “Answer”, “text”: “Yes. With evidence-based care, you can process trauma so it no longer controls daily life.”}
},
{
“@type”: “Question”,
“name”: “Does insurance cover trauma therapy in Florida?”,
“acceptedAnswer”: {“@type”: “Answer”, “text”: “Often yes. Thrive accepts Cigna, Optum, Florida Blue, and more. Verify benefits online in 2 minutes.”}
}
]
}
From Surviving to Thriving: Your Path Forward
Childhood trauma may have shaped your past, but it does not have to define your future. Healing is about integration—weaving your experiences into a new story where you are the author.
This journey takes courage, but it is achievable. The same resilience that helped you survive can now help you thrive. With evidence-based therapies like EMDR and structured support from programs like IOP or PHP, you can teach your brain and body new ways of being in the world that allow for trust, connection, and peace.
Asking for help is a sign of strength. You are not broken; you are a survivor who deserves to heal and flourish. Your story isn’t over.
Ready for support? Thrive offers virtual and hybrid IOP/PHP with evening options. Verify your insurance in 2 minutes (no obligation) → Start benefits check or call 561-203-6085. If you’re in crisis, call/text 988.