Beyond the Surface: A Guide to Active and Passive Suicidal Ideation

Essential 1: difference between active vs passive suicidal thoughts
Understanding When Thoughts Cross the Line
If you or someone you know is in crisis, call or text 988 right now. You are not alone.
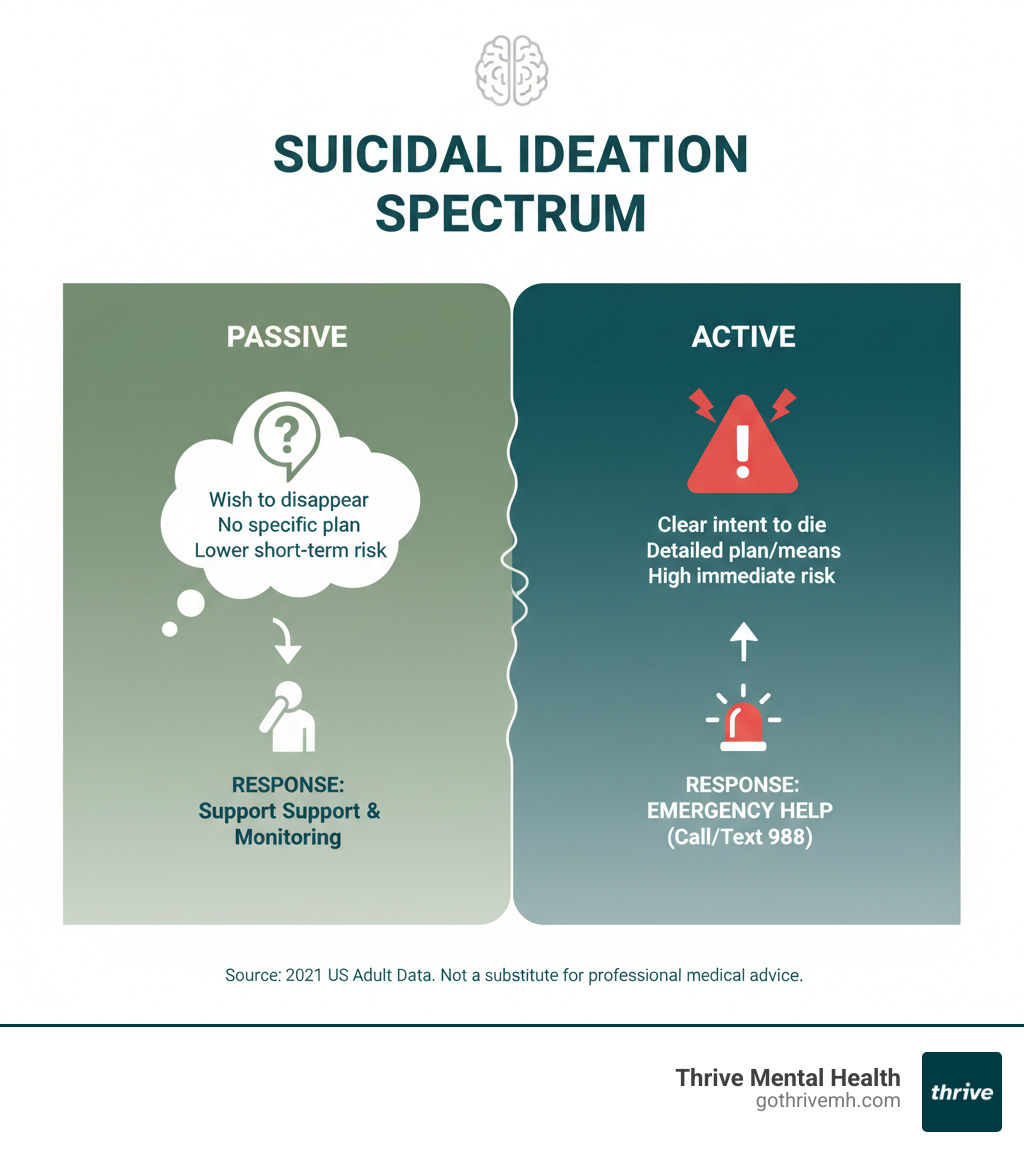
The difference between active vs passive suicidal thoughts comes down to intent, planning, and immediacy. While any thought of suicide is a serious sign of distress, knowing the distinction is critical for getting the right help.
| Type | Intent to Die | Specific Plan | Access to Means | Immediate Risk |
|---|---|---|---|---|
| Passive Suicidal Ideation | Wishes for death but no intent to act | No | No | Lower, but a serious warning sign |
| Active Suicidal Ideation | Clear intent to end life | Yes | Yes, or actively seeking | High—requires emergency intervention |
Suicidal thoughts exist on a spectrum. Passive ideation includes thoughts like “I wish I could just disappear,” signaling deep pain without a plan. Active ideation is a psychiatric emergency that includes a desire to die, a specific plan, and the intent to act.
In 2021, 12.3 million U.S. adults had suicidal thoughts, but far fewer had active plans. Understanding this gap helps clinicians, families, and individuals determine the right level of care. It’s the key to saving lives and showing that recovery is possible.
I’m Anna Green, LMHC, LPC, Chief Clinical Officer at Thrive Mental Health. My work focuses on evidence-based, stigma-free care for individuals across the spectrum of suicidal ideation. We help people move from crisis to building lives they want to live.
What is Suicidal Ideation? More Than Just a Passing Thought
Suicidal ideation is the clinical term for thinking about ending your own life. It’s not a single type of thought but a spectrum of intensity, from vague wishes to die to detailed plans. It’s also far more common than most people realize.
In 2021, 12.3 million U.S. adults (4.3% of the population) reported suicidal thoughts. Among youth, 18% have considered suicide before age 18. With suicide rates climbing 36% over the last two decades nationally, it is now the second leading cause of death for adolescents and young adults, according to data from the CDC. This crisis is deeply felt here in Florida, where communities across the state are impacted.
These thoughts are a serious warning sign of deep distress. However, having them doesn’t automatically mean someone will attempt suicide. Early recognition and professional care are key. Understanding the difference between active vs passive suicidal thoughts helps determine the right level of intervention. If you’re seeing warning signs, our guide on Understanding Early Warning Signs and Symptoms can help.
How Intrusive Thoughts Differ From Suicidal Ideation
It’s crucial to distinguish suicidal ideation from intrusive thoughts. Intrusive thoughts are unwanted, involuntary mental images or urges that are ego-dystonic—meaning they conflict with your values and desires. You don’t want them, and they often cause distress or disgust.
For example, a fleeting, unwanted thought of jumping while on a high balcony is an intrusive thought. There is no intent to act.
Suicidal ideation, in contrast, involves a desire to die. The thought is not just an unwelcome flash; it can become a recurring focus or be seen as a solution to pain.
Intrusive thoughts are common in anxiety disorders and Obsessive-Compulsive Disorder (OCD), where individuals may get stuck trying to suppress them. You can learn more in our article on OCD Symptoms. Mistaking one for the other can lead to unnecessary panic or, worse, missing a real cry for help.
The Critical Difference Between Active vs Passive Suicidal Thoughts
Understanding the difference between active vs passive suicidal thoughts is the framework that guides an effective response. Both signal deep distress and require professional attention, but the presence of intent and a plan dictates the urgency and type of help needed.
Passive ideation is a wish for pain to stop, while active ideation is a plan to end one’s life. Recognizing this gap allows clinicians to assess risk accurately, helps families ask the right questions, and ensures people get the level of care they need.
Passive Suicidal Ideation: When You Wish It Would All Just End
Passive suicidal ideation is about wanting unbearable emotional pain to stop, not necessarily about wanting to die. It’s a feeling of exhaustion and hopelessness, often expressed as a wish for an external event to end one’s life.
People experiencing passive ideation might think or say things like:
- “I wish I could go to sleep and not wake up.”
- “Everyone would be better off without me.”
- “I wish I was never born.”
- “I hope I get into an accident.”
These thoughts reflect a sense of being a burden and a desperate desire for escape, but they lack a specific plan or intent to act. Our guide on Why Do I Feel Like a Burden and How to Heal? explores this feeling.
The danger is that these thoughts are easily dismissed. However, they are a serious warning sign. Without intervention, passive thoughts can escalate into active planning, especially with added stress. Seeking help at this stage is crucial. Learn more in our article on Passive Suicidal Ideation.
Active Suicidal Ideation: When Thoughts Turn into Plans
Active suicidal ideation is when the desire to die becomes a concrete intention. It’s not just “I wish I were dead,” but “I am going to end my life, and this is how.” The person has a method, may have access to means, and intends to act. This is a mental health emergency.
Someone might say, “I’m going to jump off that bridge tonight” or “I have a gun, and I’m going to use it.”
Warning signs that require immediate action include:
- Giving away prized possessions or settling affairs.
- Saying goodbye in a way that feels final.
- A sudden, unexplained calmness after a period of distress, which may signal a decision has been made.
- Acquiring means like stockpiling pills or buying a weapon.
- Writing a suicide note or researching methods.
If you see these signs, do not wait. Call 988 or take the person to an emergency room. Our resource on Crisis Intervention for Suicidality provides guidance on how to respond.
Why Do These Thoughts Happen? Risk Factors and Professional Assessment
Suicidal thoughts arise from a complex mix of pain, stress, and circumstances that feel overwhelming. They are a desperate signal that a person’s pain has exceeded their ability to cope. Understanding the underlying causes is key to finding a path to relief.

Common Triggers and Risk Factors for Suicidal Ideation
While every person’s story is unique, certain factors significantly increase the risk of suicidal thoughts:
- Mental Health Conditions: About 90% of people who die by suicide have an underlying psychiatric illness. Conditions like depression, bipolar disorder, severe anxiety, and PTSD can make death feel like the only escape.
- Childhood Trauma: Research shows that abuse, neglect, and other adverse childhood experiences are strong predictors of suicidal ideation in adulthood.
- Substance Use Disorders: Alcohol and drugs impair judgment and intensify negative emotions. Alcoholism rates are dramatically higher among those who die by suicide.
- Major Life Stressors: Job loss, financial crisis, relationship breakdowns, or chronic illness can feel catastrophic and push someone past their breaking point.
- Social Isolation: Feeling alone magnifies all other risks. Strong social support is a powerful protective factor, making people more than 30% less likely to attempt suicide.
- Identity-Related Stress: Vulnerable populations face higher risks. For example, 45% of LGBTQIA+ youth seriously considered suicide in the past year due to discrimination and rejection.
- ADHD and Emotional Dysregulation: Particularly in adolescents, research links ADHD to impulsivity and difficulty managing emotions, which can contribute to suicidal thoughts.
How Professionals Assess Risk: The difference between active vs passive suicidal thoughts
When a clinician assesses suicidal ideation, the goal is to understand the depth of the person’s pain, determine their level of risk, and create a plan for safety and treatment.
The assessment involves:
- Asking Direct Questions: Discussing suicide openly and without judgment does not increase risk; it reduces it. We ask about the frequency, intensity, and duration of the thoughts.
- Distinguishing Active vs. Passive Ideation: We determine if the person is wishing for death (passive) or has a plan to die (active). This distinction is critical.
- Evaluating Plans and Intent: If a plan exists, we ask about the specifics: the method, access to means, and the strength of their intent to act. Removing lethal means is a key prevention strategy.
- Identifying Protective Factors: We also explore reasons for living—connections, responsibilities, and past coping strategies that can serve as anchors.
- Using Standardized Tools: We often use scales like the Columbia-Suicide Severity Rating Scale (C-SSRS) to systematically evaluate risk.
- Creating a Safety Plan: The assessment always concludes with a personalized safety plan. This is a concrete roadmap for managing crises, including warning signs, coping strategies, and emergency contacts like the 988 Lifeline.
Our team of Expert Mental Health Professionals is trained to steer these conversations with clinical precision and deep compassion.
From Ideation to Action: Treatment That Saves Lives
Here’s the most important thing to know: treatment works. Whether you’re experiencing passive wishes for it to end or have an active plan, evidence-based interventions offer real hope. Recovery isn’t about “thinking happy thoughts”—it’s about addressing the root causes of distress and building skills to create a life you want to live.
Immediate Steps vs. Long-Term Treatment: The difference between active vs passive suicidal thoughts
The difference between active vs passive suicidal thoughts dictates the response. Active ideation is an emergency; passive ideation requires urgent clinical care.
For Active Suicidal Ideation (An Emergency):
- Call or text 988 immediately. If someone is in immediate danger, call 911. This is a life-saving action.
- Remove lethal means. Secure firearms, lock up medications, and remove anything that could be used in a crisis. This simple step creates a crucial window of time.
- Seek emergency evaluation. Active ideation typically requires evaluation at a hospital to ensure safety and begin stabilization. This is a protective measure, not a punishment. Our team can help guide families through this process, as detailed in our resource on Crisis Intervention for Suicidality.
For Long-Term Recovery (Passive and Post-Crisis Active Ideation):
Once a person is safe, the work of healing begins. Psychotherapy is the cornerstone of long-term recovery.
- Cognitive Behavioral Therapy (CBT): This therapy helps identify and challenge the negative thought patterns fueling suicidal ideation. Research shows CBT is highly effective at reducing suicidal thoughts and preventing attempts by teaching practical coping and problem-solving skills.
- Dialectical Behavior Therapy (DBT): DBT is especially powerful for those with intense emotions or a history of self-harm. It teaches skills in mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness, significantly reducing suicide attempts.
- Medication Management: For many, medications like antidepressants or mood stabilizers are crucial for treating underlying conditions like depression or bipolar disorder. These are carefully prescribed and monitored by a medical professional.
- Higher Levels of Care: For those in Florida needing more than weekly therapy, our Intensive Outpatient Program (IOP) provides structured group and individual therapy while allowing clients to live at home. Our Virtual IOP makes this care accessible to residents across the state. We work with major insurers common in Florida, including Aetna, Cigna, Florida Blue, and Optum.
How to Support a Loved One (and Yourself)
Your support can be a lifeline. Research shows strong social connections make a significant difference. You don’t have to be a therapist—just be present and willing to help.
- Listen Without Judgment: Create a safe space for them to talk without trying to fix their pain. Acknowledging their struggle is powerful.
- Ask Direct Questions: Asking “Are you thinking about suicide?” does not plant the idea. It opens the door for an honest conversation and shows you care.
- Encourage Professional Help: Gently but persistently offer to help them find a therapist or make an appointment.
- Remove Means & Create a Safety Plan: If they have a plan, work with them to remove access to lethal means. Help them collaborate with a professional to create a written safety plan.
- Take Care of Yourself: Supporting someone in crisis is exhausting. Seek your own support through therapy or trusted friends. Our Mental Health Tips – Ultimate Guide offers more strategies. For parents, teaching adolescents coping mechanisms is a key protective skill.
Frequently Asked Questions about Active vs. Passive Suicidal Ideation
What is the main difference between active and passive suicidal thoughts?
The main difference between active vs passive suicidal thoughts is intent and planning. Passive ideation involves wishing for death or for pain to end without a specific plan or intent to act (e.g., “I wish I wouldn’t wake up”). Active ideation includes a specific plan, access to means, and the intent to die (e.g., “I am going to take these pills tonight”). Active ideation is a psychiatric emergency.
Is passive suicidal ideation an emergency?
While not an immediate crisis like active ideation, passive suicidal ideation is a serious warning sign that requires professional mental health treatment. It signals profound distress and hopelessness. Left unaddressed, the underlying pain can worsen, and the thoughts can escalate into active planning, especially during times of increased stress. It should never be ignored.
Can passive thoughts turn into active ones?
Yes, and this is why early intervention is critical. Passive thoughts can escalate into active ideation. Triggers like a major loss, worsening depression, or increased isolation can erode a person’s coping abilities and protective factors, leading them to move from wishing for death to actively planning it. Evidence-based treatments like Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT) are designed to interrupt this progression. Our Intensive Outpatient Program (IOP) provides the structured support needed to address these thoughts before they escalate.
You Are Not Alone: Take the First Step Toward Healing
Understanding the difference between active vs passive suicidal thoughts is a critical first step, but the most important takeaway is this: recovery is possible.
You cannot always stop painful thoughts from appearing, but you can learn to manage them. Evidence-based treatment dramatically reduces their power and prevents them from turning into action. At Thrive Mental Health, our Evidence-Based Suicide Prevention programs are built to do exactly that—equip you with real tools to build a life that feels worth living.
We meet you where you are, whether in the fog of passive ideation or the crisis of an active plan. At Thrive Mental Health, we are deeply committed to serving the Florida community. Our flexible virtual and hybrid programs are designed to fit your life, making evidence-based care accessible to residents across the state. We accept major insurance, including Aetna, Cigna, Florida Blue, and Optum, to make care accessible. You don’t have to do this alone.
Ready for support? Thrive offers virtual and hybrid IOP/PHP programs with evening options. Verify your insurance in 2 minutes (no obligation) → Start benefits check or call 561-203-6085. If you’re in crisis, call/text 988.

