Why Dual Diagnosis Treatment is Vital for Young Adults

The Hidden Crisis: When Mental Health and Substance Use Collide
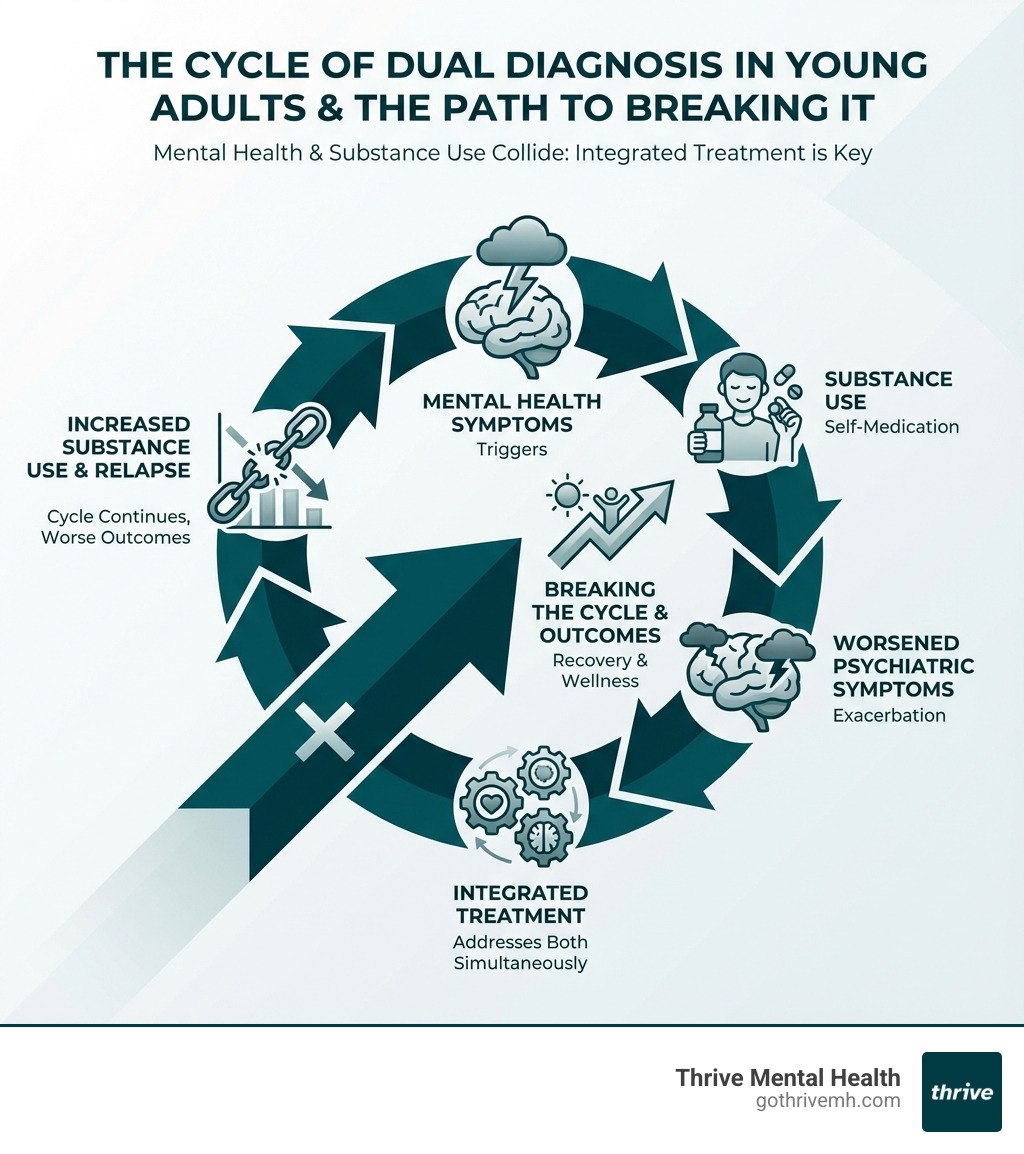
Dual diagnosis young adults face a unique and often misunderstood challenge: experiencing both a mental health disorder and a substance use disorder at the same time. This isn’t just two separate problems—it’s a dangerous cycle where each condition makes the other worse.
Quick Facts About Dual Diagnosis in Young Adults:
- Over 50% of young adults (ages 18-25) with substance use disorders have at least one co-occurring psychiatric disorder
- When present together, these conditions lead to more severe symptoms, higher relapse rates, and increased suicide risk
- Most psychiatric disorders begin by young adulthood, increasing the risk of developing substance use problems
- Young adults with dual diagnosis experience worse treatment outcomes when only one condition is addressed
Common Co-Occurring Conditions Include:
- Depression + Alcohol or Opioid Use
- Anxiety + Marijuana or Alcohol Use
- PTSD + Any Substance Use Disorder
- Bipolar Disorder + Alcohol or Cannabis Use
- ADHD + Misuse of Prescription Stimulants
The problem is urgent. Traditional treatment often fails because it addresses mental health or substance use—but not both at once. Young adults get caught in a revolving door: they stabilize one condition only to relapse because the other was never treated. They’re told to get sober before addressing trauma, or to fix their depression before dealing with addiction. This approach doesn’t work.
The good news? Integrated treatment that addresses both conditions simultaneously can break this cycle. When young adults receive the right care—trauma-informed, developmentally appropriate, and flexible enough to fit their lives—recovery isn’t just possible. It’s probable.
I’m Nate Raine, CEO of Thrive Mental Health, and over the past decade I’ve led initiatives that bridge clinical care, data science, and real-world outcomes for individuals struggling with complex behavioral health needs, including dual diagnosis young adults. At Thrive, we’ve built programs in Florida specifically designed to treat co-occurring disorders with the intensity and flexibility this population needs.
What is Dual Diagnosis? [The Unseen Crisis Facing Young Adults]
A dual diagnosis, also known as co-occurring disorders, refers to the simultaneous presence of a mental health condition and a substance use disorder (SUD). For dual diagnosis young adults, this isn’t just a coincidence; it’s a complex interplay where each condition fuels and complicates the other. Think of it like a tangled knot: pulling one thread tighter only makes the other harder to untangle.
Why is this such a growing concern, especially for young adults aged 18-25 in Florida and across the nation? The statistics paint a stark picture: over 50% of young adults with SUDs also struggle with at least one co-occurring psychiatric disorder. This isn’t a minor issue; it’s a widespread challenge with devastating consequences. When mental health disorders and SUDs occur together, they exacerbate one another, creating a vicious cycle. Symptoms become more severe, engagement in treatment drops, and the risk of relapse for both conditions skyrockets. The prognosis worsens significantly, including a dangerously higher risk of suicide. Critical scientific research on co-occurring disorders underscores the urgency of addressing co-occurring disorders in this age group.
Common co-occurring conditions we see in dual diagnosis young adults include:
- Anxiety Disorders & Alcohol/Marijuana Use: Young adults often use substances like alcohol or marijuana to self-medicate feelings of anxiety, leading to a cycle of temporary relief followed by worsened anxiety and increased substance dependence.
- Depression & Stimulant/Opioid Use: Depression can drive individuals to seek the temporary euphoria or escape offered by stimulants or opioids, which ultimately deepens depressive states and creates a physical and psychological addiction.
- PTSD & Substance Use Disorders (SUDs): Trauma survivors frequently turn to substances to numb painful memories or manage hyperarousal symptoms, making it incredibly difficult to process their trauma and achieve lasting sobriety.
- Bipolar Disorder & Alcohol/Cannabis Use: The extreme mood swings of bipolar disorder can lead young adults to use substances to stabilize their mood—alcohol to calm manic episodes or cannabis to alleviate depressive lows—resulting in a worsening of both conditions.
- ADHD & Misuse of Prescription Stimulants: Young adults with ADHD may misuse prescribed stimulants, or seek illicit ones, to improve focus or manage impulsivity. This can lead to addiction and exacerbate underlying ADHD symptoms.
Why Young Adulthood is a Critical Period for Intervention
Young adulthood (ages 18-25) is a period of immense change and vulnerability. The brain is still undergoing significant development, particularly the prefrontal cortex responsible for decision-making, impulse control, and emotional regulation. This ongoing neurodevelopment makes young adults biologically susceptible to the impacts of substance use, which can disrupt critical brain processes and predispose them to neuropsychiatric complications.
This stage is also marked by identity formation, a time when individuals are figuring out who they are and their place in the world. It’s a period of transition, often involving moving away from home, starting college or a career, and navigating new social dynamics. These pressures, combined with a developing brain, can lead to increased risk-taking behavior, including substance experimentation.
Alarmingly, most psychiatric disorders begin by young adulthood. Depression, anxiety, and other mental health conditions often manifest for the first time during these years, significantly increasing the risk of subsequent SUD development. When these conditions emerge, they can be particularly challenging to steer amidst the push for independence. Without proper intervention, dual diagnosis young adults can find themselves trapped in a cycle that jeopardizes their entire future. Early intervention is crucial to prevent a long-term chronic course of illness.
The Alarming Link Between Dual Diagnosis and Suicide Risk
When mental health disorders and substance use disorders co-exist, they don’t just worsen symptoms; they tragically lift the risk of suicide. This is a critical concern for dual diagnosis young adults. The presence of both conditions leads to more profound functional impairment and worse prognoses, including a higher risk of suicide.
The combination of severe mental health symptoms like deep depression or extreme anxiety, coupled with the disinhibiting and mood-altering effects of substances, can create a dangerous cocktail. Substances can intensify feelings of hopelessness, increase impulsivity, and impair judgment, making it harder for young adults to cope with distress and more likely to act on suicidal thoughts.
If you or someone you know is in crisis or considering suicide, call or text 988 immediately to connect with the 988 Suicide & Crisis Lifeline. You are not alone.
For dual diagnosis young adults, integrated care that addresses both conditions simultaneously is not just about recovery—it’s about survival. By stabilizing mental health symptoms and supporting sobriety, we can significantly reduce this alarming risk and offer a path toward safety and well-being.
The Trauma Connection: Why Past Pain Fuels Present Struggles

It’s impossible to discuss dual diagnosis in young adults without addressing the profound impact of trauma. For many, past pain isn’t just a memory; it’s a living force that fuels present struggles, often manifesting as a dual diagnosis. We know that an estimated 75% of adults in substance use treatment report interpersonal abuse and trauma histories. Even more striking, 84% of individuals with SUDs report exposure to four or more Adverse Childhood Experiences (ACEs), compared to just 13% of the general adult population.
ACEs are traumatic events that occur in childhood, such as abuse (physical, emotional, sexual), neglect, or household dysfunction (e.g., parental mental illness, substance abuse, divorce, incarceration). These experiences leave deep scars, altering brain development and increasing vulnerability to both mental health disorders and substance use later in life. Young adults who’ve experienced ACEs are often caught in a self-medication cycle, using substances to numb emotional pain, escape difficult memories, or regulate overwhelming feelings that they never learned to manage in a healthy way.
This connection isn’t just theoretical; it has a tangible impact on treatment outcomes. ACEs and childhood trauma are associated with worse outcomes in substance use treatment, including higher severity of and shorter time to relapse. The neurobiology of trauma shows how chronic stress and adverse experiences can rewire the brain, affecting areas related to stress response, emotion regulation, and reward processing. This makes it incredibly challenging for dual diagnosis young adults to engage in traditional treatment approaches that don’t acknowledge or address their underlying trauma.
At Thrive Mental Health, we understand that effective recovery for young adults with co-occurring disorders means addressing the deep-seated impact of trauma. Our integrated treatment programs are designed to provide comprehensive support, including trauma-focused therapy. You can find more information about our approach to trauma-focused therapy on our IOP program page.
How Trauma-Informed Care Changes Everything for Dual Diagnosis Young Adults
Recognizing the pervasive impact of trauma, we believe that trauma-informed care is not just an add-on; it’s a foundational principle for treating dual diagnosis young adults. Trauma-informed care operates on the assumption that trauma exposure is common and that many individuals seeking treatment have experienced it. It shifts the focus from “What’s wrong with you?” to “What happened to you?”.
This approach fundamentally changes the treatment environment and interaction. Key principles include:
- Safety and Trust: Creating a physically and psychologically safe environment where young adults feel secure enough to share their experiences without fear of judgment or re-traumatization. This includes clear boundaries, predictability, and transparency.
- Collaboration and Empowerment: Ensuring that young adults are active participants in their treatment planning and decision-making. This fosters a sense of control and self-efficacy, which is often undermined by trauma.
- Peer Support: Recognizing the healing power of shared experiences. Connecting young adults with peers who have similar histories can reduce isolation and build a sense of community.
- Cultural Responsiveness: Understanding how cultural background can influence the experience and expression of trauma, and tailoring care to be respectful and effective across the diverse populations in Florida.
By adopting a trauma-informed lens, we can better understand the root causes of substance use and mental health struggles, rather than just addressing the surface-level symptoms. This approach helps dual diagnosis young adults develop healthier coping mechanisms, rebuild trust, and begin the profound process of healing.
What is Trauma-Specific Treatment for Dual Diagnosis Young Adults?
While trauma-informed care creates a supportive environment, trauma-specific treatment directly addresses the symptoms and impact of trauma. For dual diagnosis young adults, these evidence-based therapies are crucial for resolving past experiences and preventing relapse.
Several modalities have proven effective in treating Post-Traumatic Stress Disorder (PTSD) and co-occurring SUDs:
- Eye Movement Desensitization and Reprocessing (EMDR): This therapy helps individuals process traumatic memories and reduce their emotional impact through guided eye movements or other bilateral stimulation. EMDR has shown promise in reducing craving and improving PTSD symptoms in individuals with co-occurring SUDs.
- Cognitive Processing Therapy (CPT): CPT focuses on helping individuals identify and challenge unhelpful thoughts and beliefs related to their trauma. By re-evaluating these thoughts, young adults can gain a new understanding of their traumatic experiences and reduce their emotional distress. This can be particularly effective for adolescents and young adults who have experienced childhood sexual and physical abuse.
- Seeking Safety: This is a present-focused therapy specifically designed for individuals with co-occurring PTSD and SUD. It helps clients develop coping skills to manage their symptoms without re-traumatizing them by extensively revisiting past events. It focuses on safety skills, healthy relationships, and self-care.
It is crucial that PTSD and SUD are treated simultaneously. Historically, individuals were often told they needed to achieve sobriety before addressing their trauma, or vice versa. However, this sequential approach is often ineffective because the two conditions are so intertwined. Treating both at once, within an integrated framework, offers the best chance for lasting recovery for dual diagnosis young adults. For more detailed guidance on trauma-informed behavioral health services, we recommend this comprehensive guide.
How Integrated Treatment Breaks the Cycle [5 Pillars of Success]

The heart of effective care for dual diagnosis young adults lies in integrated treatment. This isn’t merely offering mental health therapy and substance use counseling under the same roof; it’s about a seamless, coordinated approach where both conditions are treated as interconnected aspects of a single disorder. Unlike sequential treatment, which attempts to address one issue before the other, integrated care acknowledges that true healing can only happen when both are tackled simultaneously.
Integrated care for young adults can manifest in various settings, including patient-centered medical homes (PCMH) and collaborative care models. These models emphasize communication and coordination among all providers involved in a young adult’s care, ensuring a holistic and unified treatment plan. At Thrive Mental Health, we understand that a structured environment is paramount. Our programs provide the necessary support and boundaries that help young adults focus on their recovery journey, free from the daily stressors and triggers that often exacerbate their conditions.
Pillar 1: Integrated & Adaptive Assessment
For dual diagnosis young adults, assessment is not a one-time event but an ongoing process. We believe in continuous evaluation, regularly assessing and adapting to the evolving mental health needs, motivations, and treatment goals of our clients. Young adults are in a dynamic developmental stage, and their needs can change rapidly. Our clinicians are trained to use evidence-based strategies like motivational interviewing (MI) and motivational improvement therapy (MET) to engage young adults, explore their ambivalence about change, and foster intrinsic motivation.
Shared decision-making is another cornerstone of our approach. We empower young adults to be active participants in their treatment planning, ensuring that their preferences, values, and goals are at the center of their care. This collaborative process builds a strong therapeutic alliance, which is a critical factor in supporting recovery, improving symptoms, and enhancing treatment engagement and satisfaction. Our PHP programs offer an excellent example of this comprehensive, adaptive assessment in action.
Pillar 2: Developmentally-Custom Therapies
Effective treatment for dual diagnosis young adults requires therapies custom to their unique developmental stage. We use a range of evidence-based therapeutic modalities that are proven to be effective for this population:
- Cognitive Behavioral Therapy (CBT): This therapy helps young adults identify and change negative thought patterns and behaviors that contribute to both their mental health symptoms and substance use. It equips them with practical coping skills and problem-solving strategies.
- Dialectical Behavior Therapy (DBT): Particularly helpful for young adults struggling with intense emotions, impulsivity, and relational difficulties, DBT teaches skills in mindfulness, emotion regulation, distress tolerance, and interpersonal effectiveness.
- Group Therapy: Group settings provide a powerful sense of community and validation. Young adults can connect with peers facing similar challenges, share experiences, practice new skills, and receive mutual support. This fosters a sense of belonging and reduces isolation.
- Life Skills Training: Beyond clinical therapy, we focus on practical life skills essential for independent young adulthood. This includes stress management, financial literacy, healthy communication, time management, and problem-solving—all crucial for sustaining recovery.
- Vocational Support: Helping young adults explore educational or career paths provides purpose and structure. We offer support in identifying interests, setting goals, and developing the skills needed to pursue meaningful work or education, contributing to overall well-being and stability.
These therapies, delivered by our expert clinical teams in Florida, are designed to address the complex needs of dual diagnosis young adults, promoting not just symptom reduction but holistic personal growth.
Pillar 3: Flexible & Accessible Treatment Settings
We understand that dual diagnosis young adults need treatment that fits into their lives, not the other way around. Traditional inpatient care can be disruptive, and once-a-week therapy may not be enough. That’s why we offer flexible and accessible treatment settings through our Intensive Outpatient Programs (IOP) and Partial Hospitalization Programs (PHP). These programs provide the clinical intensity required for significant change, while still allowing young adults to maintain their responsibilities, such as school or work.
Here’s a comparison of our in-person and virtual IOP/PHP options:
| Feature | In-Person IOP/PHP | Virtual IOP/PHP |
|---|---|---|
| Structure | Structured clinical environment, daily/multiple weekly sessions | Structured clinical environment, daily/multiple weekly sessions |
| Location | Thrive Mental Health centers in Florida | Access from anywhere in Florida with internet access |
| Community | In-person peer support and group activities | Virtual group sessions, online community support |
| Flexibility | Fixed schedules, may require travel | Highly flexible scheduling, evening options available |
| Accessibility | Limited by geographical proximity | Overcomes geographical barriers, ideal for rural areas or mobility issues |
| Privacy | Discreet office visits | Improved privacy from home |
| Cost/Insurance | Generally covered by insurance | Generally covered by insurance (Cigna, Optum, Florida Blue, etc.) |
| Engagement | Direct personal interaction | High engagement through interactive virtual platforms |
The benefits of virtual care, in particular, are transformative for dual diagnosis young adults. It removes geographical barriers, allowing access to high-quality care whether they are in a busy city like Miami or Orlando, or a more rural community in the Panhandle. Flexible scheduling, including evening options, means they can continue their education or employment while receiving intensive treatment, reducing disruption to their lives. Our virtual IOP programs allow young adults to receive evidence-based care from the comfort and privacy of their own homes.
Pillar 4: Strategic Family Involvement
The family unit plays a pivotal role in the recovery journey of dual diagnosis young adults. We recognize that a dual diagnosis doesn’t just affect the individual; it impacts the entire family system—emotionally, socially, and sometimes financially. Strategic family involvement is therefore a critical pillar of our integrated treatment approach.
Through family systems therapy, we work with parents, siblings, and other key family members to address underlying dynamics, improve communication patterns, and heal strained relationships. Education for parents and siblings is essential, helping them understand the complexities of dual diagnosis, identify triggers, and learn effective ways to support their loved one without enabling unhealthy behaviors.
We help families establish healthy boundaries, which are crucial for both the young adult’s recovery and the well-being of the family as a whole. By fostering open, honest communication and providing support for caregivers, we aim to transform the home environment into a place of healing and sustained recovery. When families are equipped with the right tools and understanding, they become powerful allies in their young adult’s journey to wellness.
Pillar 5: Overcoming Barriers to Care
Despite the clear need, dual diagnosis young adults often face significant barriers to accessing adequate treatment. We are committed to dismantling these obstacles to ensure that every young adult can receive the care they deserve.
- Financial Barriers: Young adults often have the highest uninsured and unemployment rates of any age group, leading to substantial financial problems for treatment. We work with major insurance providers like Cigna, Optum, and Florida Blue, as well as many others, to make our programs accessible.
- Stigma and Shame: The stigma associated with both mental health disorders and substance use can prevent young adults from seeking help. They may fear judgment from peers, family, or potential employers. Our programs foster a non-judgmental, supportive environment where vulnerability is encouraged.
- Lack of Awareness: Many young adults and their families may not recognize the signs of a dual diagnosis or understand that integrated treatment is necessary. We strive to educate and empower families in Florida about the benefits of specialized care.
- Navigating the Healthcare System: The behavioral healthcare system can be complex and fragmented, especially for co-occurring conditions. We simplify this process by guiding families through admissions, insurance verification, and treatment planning.
We understand these challenges intimately, which is why we’ve built our programs to be as accessible and supportive as possible. You can quickly verify your insurance coverage now → Start benefits check to understand your benefits and how we can help.
Frequently Asked Questions about Dual Diagnosis in Young Adults
What’s the first step if I suspect my child has a dual diagnosis?
Start with a comprehensive assessment from a qualified mental health provider specializing in co-occurring disorders. Open, non-judgmental communication is key. Your family doctor can be a good starting point for a referral.
Can you treat a dual diagnosis with just therapy?
Effective treatment almost always involves a combination of therapies. This includes individual and group therapy, and often includes medication management to stabilize mental health symptoms, which makes therapy for substance use more effective.
How long does dual diagnosis treatment take for a young adult?
There’s no set timeline. It depends on the severity of the disorders, the individual’s motivation, and the presence of a strong support system. Programs like IOP and PHP typically last several weeks to months, followed by ongoing outpatient care.
Your Path to Recovery Starts Here
The journey for dual diagnosis young adults is undeniably challenging, marked by the severe and intertwined struggles of mental health and substance use disorders. But as we’ve explored, this crisis is not without a solution. Integrated, trauma-informed care is not just a hopeful ideal; it is the evidence-based path to healing and long-term recovery.
At Thrive Mental Health, we are dedicated to providing this specialized approach. Our programs are designed to address the unique needs of young adults, offering comprehensive support that fosters improved health outcomes, stable relationships, and the foundation for career success. We offer flexible virtual and in-person IOP/PHP programs across Florida, bringing expert-led care directly to you.
Ready for support? Thrive offers virtual and hybrid IOP/PHP programs with evening options. Verify your insurance in 2 minutes (no obligation) → Start benefits check or call 561-203-6085. If you’re in crisis, call/text 988.