Chronic Pain Relief: Deciding Between EMDR and CBT

emdr vs cbt for chronic pain: Ultimate Relief 2025
Your Pain is Real. Your Relief Can Be, Too.
Choosing between EMDR vs CBT for chronic pain is a critical decision when you’re living with pain that won’t quit. Both therapies are evidence-based, but they work differently. Here’s the quick breakdown:
| Therapy | Best For | How It Works | Primary Benefit |
|---|---|---|---|
| EMDR | Pain linked to trauma or unprocessed memories | Reprocesses traumatic memories using bilateral stimulation (eye movements, tapping) | Directly reduces pain intensity, especially with 6-8 sessions |
| CBT | Pain worsened by negative thoughts and avoidance behaviors | Changes thought patterns and behaviors through structured talk therapy | Improves mood and function, reduces catastrophizing |
Key takeaway: If you have a trauma history, EMDR often reduces pain faster. If you struggle with fear and avoidance, CBT teaches coping skills to break the pain-fear cycle.
Chronic pain is more than physical. It steals your sleep, relationships, and sense of control. If you’ve tried medications and physical therapy without lasting relief, it’s likely because your brain is involved. Pain is created in the brain, and your nervous system can get stuck in a high-alert state called central sensitization, amplifying pain signals long after an injury has healed. This is why traditional treatments often fail.
Psychological therapies like EMDR and CBT can retrain your brain’s alarm system to reduce or even eliminate pain.
- EMDR (Eye Movement Desensitization and Reprocessing) helps your brain reprocess stuck memories—including the physical sensations of pain—that keep the alarm bells ringing. It’s especially effective for people with trauma histories.
- CBT (Cognitive Behavioral Therapy) focuses on changing the thoughts and behaviors that make pain worse, like catastrophic thinking and fear-avoidance.
Understanding which therapy fits your pain is the key to getting relief. At Thrive Mental Health, we specialize in evidence-based care for complex conditions like chronic pain, offering virtual and in-person programs in Florida designed for real-world recovery.
Emdr vs cbt for chronic pain helpful reading:
Why Your Brain is the Command Center for Chronic Pain
Pain doesn’t always match the injury. You can have severe pain with minimal tissue damage, or vice versa. That’s because pain isn’t created in your body—it’s created in your brain. Your brain acts as a command center, interpreting danger signals from the body (nociception) through a filter of past experiences, emotions, and beliefs. If it perceives a threat, it creates the sensation of pain.
This is where the EMDR vs CBT for chronic pain debate becomes critical. Both therapies target the brain’s alarm system, but in different ways.
In chronic pain, this alarm system gets stuck on high alert. This is called central sensitization—your nervous system becomes so hypersensitive that it generates pain even without a physical threat. Your brain’s ability to rewire itself, known as neuroplasticity, works against you, strengthening pain pathways until your brain “learns” to be in pain. The good news is that your brain can also unlearn this pattern. EMDR and CBT are designed to do just that: retrain the alarm system and build healthier neural pathways.
Trauma is a major factor. Research shows a staggering overlap between chronic pain and psychological trauma, with up to 80% of chronic pain patients having a history of trauma or PTSD. Trauma primes your nervous system for danger, making you more susceptible to central sensitization. Your brain links physical sensations with unprocessed emotional memories, trapping you in a pain loop. Research on psychological trauma and functional somatic syndromes confirms this connection.
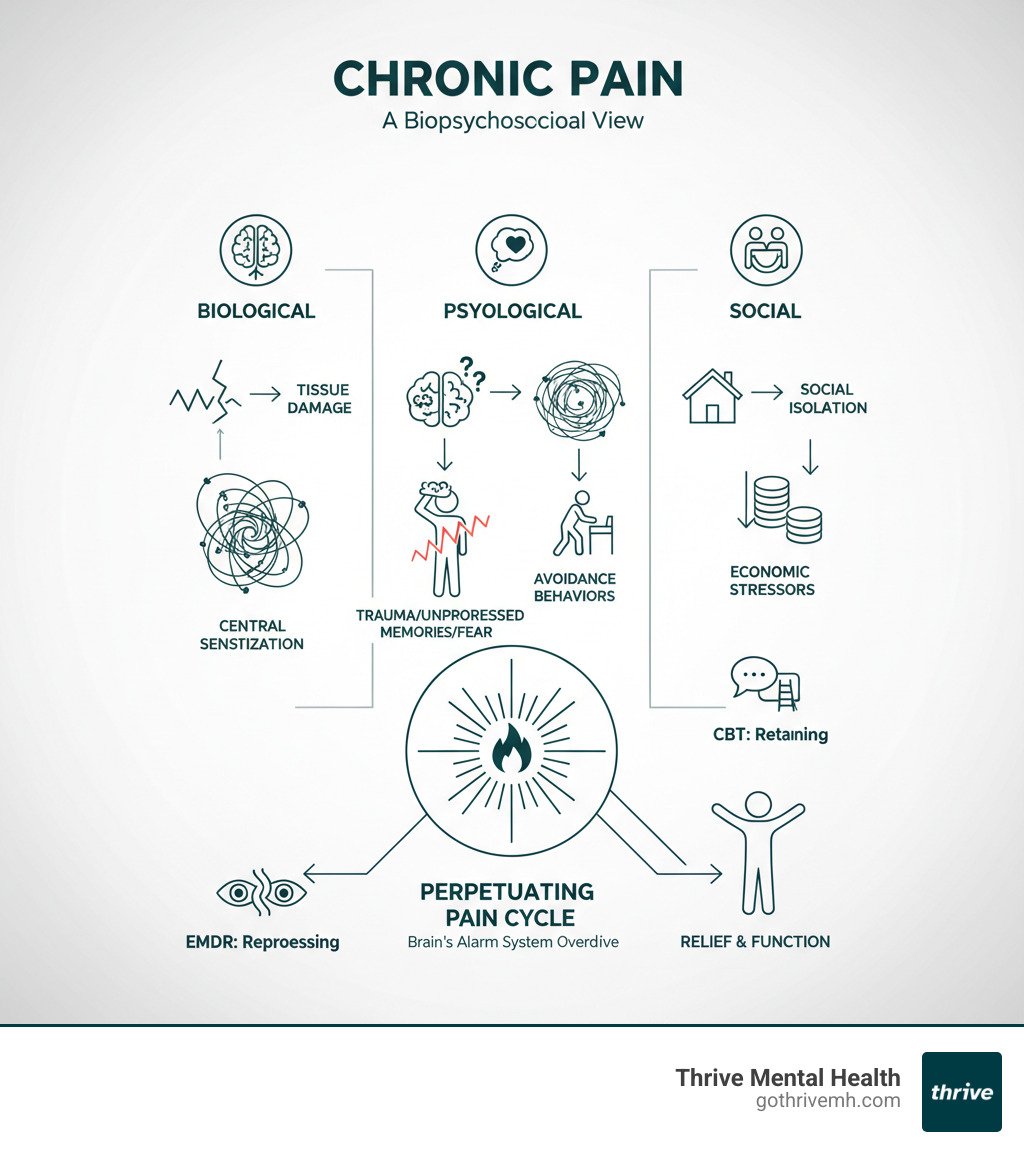
This is why the biopsychosocial model is essential. It acknowledges that pain is biological, psychological, and social. To treat it effectively, you must address the brain. Both EMDR and CBT use neuroplasticity to turn down the overactive alarm, helping your brain relearn safety and disengage the pain mechanism.
CBT for Chronic Pain: Retrain Your Brain, Reclaim Your Life
Cognitive Behavioral Therapy (CBT) is the most studied psychological treatment for chronic pain. It works by interrupting the vicious cycle where negative thoughts about pain (“This will never end”) lead to distressing feelings (hopelessness, anxiety) and unhelpful behaviors (avoiding movement, isolation), which in turn makes the pain worse.
CBT teaches you to challenge thoughts that amplify suffering, such as pain catastrophizing and the fear-avoidance model. It’s not about pretending the pain isn’t real; it’s about building practical coping skills to regain control.
CBT Techniques You’ll Actually Use
CBT is structured and hands-on. You’ll learn practical tools to use daily:
- Cognitive Restructuring: Catching, challenging, and reframing distorted thoughts about pain to reduce their emotional weight.
- Behavioral Activation: Gradually re-engaging with meaningful activities to break the fear-avoidance cycle and rebuild your life.
- Activity Pacing: Balancing activity and rest to stay active without triggering flare-ups.
- Relaxation Training: Using deep breathing, guided imagery, and other techniques to calm the nervous system and reduce muscle tension.
- Problem-Solving: Developing a systematic approach to tackle pain-related challenges instead of feeling overwhelmed.
CBT requires practice. You’ll apply these skills between sessions through “homework,” which is essential for making lasting changes.
The Evidence: What to Expect from CBT
Research confirms CBT works. It has small to medium, but meaningful, effects on pain, disability, and mood. Its greatest strengths are in reducing psychological distress (anxiety, depression) and improving daily function. You learn to cope better and feel less controlled by your pain. The American Psychiatric Association (APA) recognizes its effectiveness for co-occurring conditions.
However, CBT’s direct effects on pain intensity can be more limited long-term. It excels at helping you manage your life around pain, but may not reduce the physical sensation as much as other approaches. Research on CBT for functional somatic syndromes supports its value in reducing disability even when pain persists.
When considering EMDR vs CBT for chronic pain, this is a key difference: CBT teaches you to respond differently to pain, while EMDR often targets the pain signal itself. At Thrive Mental Health, we integrate CBT into our virtual IOP and PHP programs available to all residents of Florida.
EMDR for Chronic Pain: Heal Past Trauma to End Present Pain
Eye Movement Desensitization and Reprocessing (EMDR) is a powerful therapy for chronic pain, especially when it’s linked to trauma. It’s based on the idea that your brain can hold onto painful experiences—including the physical sensations—long after your body has healed. This is the Adaptive Information Processing (AIP) model.
When a distressing event occurs, the memory can get “stuck” with all its original emotions and somatic sensations (physical feelings). For chronic pain, this means your brain might still be holding the “memory” of an injury, constantly triggering your nervous system’s danger alarm and generating real pain. EMDR helps your brain properly process and file away these stuck memories, breaking the neurological loop.
How EMDR Directly Targets Pain Signals

EMDR goes straight to the source using bilateral stimulation (BLS)—guided eye movements, tapping, or tones. While engaging in BLS, you’ll focus on a specific pain-related memory (e.g., the initial injury, a traumatic event). This activates your brain’s natural processing system, similar to REM sleep, allowing it to reprocess the memory.
Through EMDR’s 8-phase protocol, your therapist helps you target these memories. During the desensitization phase, you focus on the memory and the associated physical pain. As you process with BLS, the intensity of both the memory and the pain itself often decreases. You are effectively desensitizing the pain sensations by changing how your brain stores the experience. For more on the process, visit the EMDRIA website.
The Evidence: Does EMDR Work for Chronic Pain?
This is where the EMDR vs CBT for chronic pain comparison is stark. While CBT improves coping, EMDR often leads to direct improvement in pain intensity. Clinical trials show EMDR can reduce and sometimes eliminate pain, especially with co-morbid trauma.
Effective treatment typically requires six to eight sessions to give the brain time to reprocess memories and recalibrate the danger alarm. Research on EMDR’s efficacy in pain treatment supports this. A key advantage is less homework; the main work happens in-session, which is a relief for those overwhelmed by chronic pain. If your pain is linked to a specific trauma, EMDR may offer faster relief. At Thrive Mental Health, our Florida-based virtual IOP and PHP programs leverage EMDR to help clients achieve breakthroughs.
The Ultimate Showdown: EMDR vs CBT for Chronic Pain
When weighing EMDR vs CBT for chronic pain, you’re choosing a path. Both are backed by research, but they work in fundamentally different ways. Understanding these differences helps you find relief faster.
| Feature | EMDR for Chronic Pain | CBT for Chronic Pain |
|---|---|---|
| Core Theory | Adaptive Information Processing (AIP): Unprocessed traumatic memories (including pain sensations) get “stuck” and need reprocessing. | Cognitive Model: Thoughts, feelings, and behaviors are interconnected; changing negative patterns reduces distress and improves function. |
| Best For | Pain with a trauma history; unexplained pain; pain sensations tied to past events; those who prefer less verbal processing. | Pain worsened by negative thoughts (catastrophizing); fear-avoidance behaviors; poor coping skills; those who prefer structured problem-solving. |
| Session Focus | Processing specific distressing memories and sensations using bilateral stimulation (BLS) to facilitate resolution. | Identifying and challenging negative thoughts; developing coping strategies; setting behavioral goals; learning relaxation techniques. |
| Homework | Minimal formal homework; focus is on in-session processing. | Specific assignments: thought records, behavioral experiments, activity scheduling. |
| Primary Outcome | Direct reduction in pain intensity and emotional distress; shifts in the somatic experience of pain. | Improved function, reduced psychological distress (anxiety, depression), better coping skills, less pain catastrophizing. |
Core Approach: How do EMDR and CBT differ in treating chronic pain?
- Reprocessing vs. Restructuring: EMDR helps your brain reprocess stuck memories and sensations. CBT teaches you to consciously restructure the thoughts and behaviors that worsen pain.
- Bottom-Up vs. Top-Down: EMDR works from the “bottom-up,” starting with the raw physical and emotional experience stored in the brain. CBT works “top-down,” using your rational mind to change beliefs and behaviors.
- Somatic vs. Cognitive Focus: EMDR directly targets the physical sensation of pain during reprocessing. CBT’s primary target is your thoughts about the pain and your behavioral responses.
Who is a Better Candidate?
You might be a great fit for EMDR if:
- You have a trauma history (accident, medical trauma, childhood adversity).
- Your pain is unexplained by physical findings or feels disproportionate.
- You find talking about trauma overwhelming but feel its impact in your body.
- Your primary goal is direct reduction of pain intensity.
You are likely a better fit for CBT if:
- You notice your thoughts (e.g., catastrophizing) make your pain worse.
- You avoid activities out of fear of triggering pain.
- You prefer a structured, talk-based approach with clear, actionable skills.
- Your main goal is to improve daily function and reduce anxiety or depression.
Good news: these therapies aren’t mutually exclusive. Many people benefit from a combined approach. At Thrive Mental Health, our clinicians can help determine the best path for you.
Practical Factors: Cost, Duration, and Finding a Therapist
- Therapist Training: Both require specialized certification. At Thrive Mental Health, our clinicians are extensively trained in these evidence-based treatments.
- Duration: CBT sessions are typically 45-60 minutes over 8-20 weeks. EMDR sessions can be longer (60-90 minutes), with significant results often seen in 6-8 sessions for trauma-related pain.
- Cost & Insurance: Most major insurance plans, including Cigna, Optum, and Florida Blue, cover both therapies. You can verify your insurance coverage with us in just 2 minutes.
- Virtual Therapy: Both EMDR and CBT are highly effective online. This is a major benefit for chronic pain patients who find travel difficult. Our virtual IOP and PHP programs at Thrive offer intensive care to residents throughout Florida, with flexible evening options.
Frequently Asked Questions about Pain Therapy
Which is better in the debate of EMDR vs CBT for chronic pain?
Neither therapy is universally “better.” The best choice depends on the root of your pain.
- Choose EMDR if your pain is linked to trauma (an accident, medical procedure, PTSD). It often provides direct pain reduction by targeting the root memory.
- Choose CBT if your pain is worsened by negative thoughts (catastrophizing) and avoidance behaviors. It excels at improving function and mood by teaching practical coping skills.
Many people benefit from a combination of both.
Do I have to talk about my trauma in detail for EMDR?
No. This is a common misconception. EMDR does not require you to describe traumatic events in detail. The focus is on the internal processing of the memory while using bilateral stimulation (eye movements, tapping). Your brain does the reprocessing work without the need for extensive verbal recounting, which many find less overwhelming than traditional talk therapy.
Can I get EMDR or CBT for chronic pain online?
Yes, and it’s highly effective. Both EMDR and CBT are delivered successfully online, which is a game-changer for people with chronic pain who face mobility challenges. Virtual IOP (Intensive Outpatient) and PHP (Partial Hospitalization) programs offer structured, intensive treatment from home. At Thrive Mental Health, our virtual programs provide expert care to residents across Florida without the commute. We accept major insurance like Cigna, Optum, and Florida Blue. You can verify your insurance coverage in minutes.
Your Path to Relief: Choosing the Right Therapy for You

You’ve seen the evidence. Now it’s time to choose what’s right for you. The truth about EMDR vs CBT for chronic pain is that there’s no single winner—only what’s best for your unique history.
- If you carry trauma in your body, EMDR often works faster to reduce pain intensity by reprocessing the root memories your nervous system is holding.
- If your pain is amplified by fear, negative thinking, or avoidance, CBT gives you practical tools to break the cycle, improve function, and feel less distressed.
Sometimes, the best path is a combination of both. What matters is that you don’t have to figure it out alone.
At Thrive Mental Health, we specialize in helping people in Florida make this exact decision. Our virtual and in-person IOP and PHP programs are for those who need more than weekly therapy. We offer structured, evidence-based treatment across Florida, with evening options to fit your life.
We accept most major insurance plans, including Cigna, Optum, and Florida Blue. Chronic pain has taken enough. It’s time to take your life back.
Ready for support? Thrive offers virtual and hybrid IOP/PHP programs with evening options. Verify your insurance in 2 minutes (no obligation) → Start benefits check. If you’re in crisis, call/text 988.