How to Find United Health Covered PHP Programs

Navigating Your Path to PHP Treatment with UnitedHealthcare
Find a partial hospitalization program that is covered by United Health Company insurance by following these key steps:
- Call the member services number on your UnitedHealthcare ID card and ask specifically about “behavioral health benefits” for “partial hospitalization”
- Log in to myuhc.com and use the provider search tool to find in-network PHP facilities in your area
- Contact potential providers who accept UHC and ask them to verify your benefits and handle prior authorization
- Confirm your costs including deductible, copay, and coinsurance before starting treatment
- Get prior authorization through your chosen provider, who will submit clinical documentation to UHC on your behalf
You need intensive mental health support, but the thought of navigating your UnitedHealthcare plan feels overwhelming. Here’s the reality: finding a partial hospitalization program that is covered by United Health Company insurance doesn’t have to be complicated—you just need to know the right questions to ask and where to look.
Most UHC plans do cover PHPs for medically necessary conditions like depression, anxiety, PTSD, bipolar disorder, and substance use disorders. In fact, federal mental health parity laws require UHC to cover mental health treatment at levels comparable to physical health care. The challenge isn’t whether you’re covered—it’s understanding how to access those benefits and find quality providers who accept your plan.
The stakes are real. In 2022, 32% of U.S. adults reported symptoms of anxiety or depression, yet 60% of behavioral health providers can’t accept new patients. Meanwhile, nearly 7,710 mental health facilities accept private insurance, but not all are in your UHC network or offer the intensive PHP structure you might need.
This matters because the right PHP can be life-changing. Research shows that a six-week PHP significantly reduced symptom severity and improved relational health for participants with mental health issues. But only if you can actually access it through your insurance.
I’m Nate Raine, CEO of Thrive Mental Health, and over the past decade I’ve helped build systems that bridge the gap between clinical care and insurance coverage, making it easier to find a partial hospitalization program that is covered by United Health Company insurance across Florida. Below, I’ll walk you through exactly how to verify your benefits, locate in-network providers, steer prior authorization, and understand your costs—so you can focus on recovery, not paperwork.
What is a PHP and Does UnitedHealthcare (UHC) Cover It?
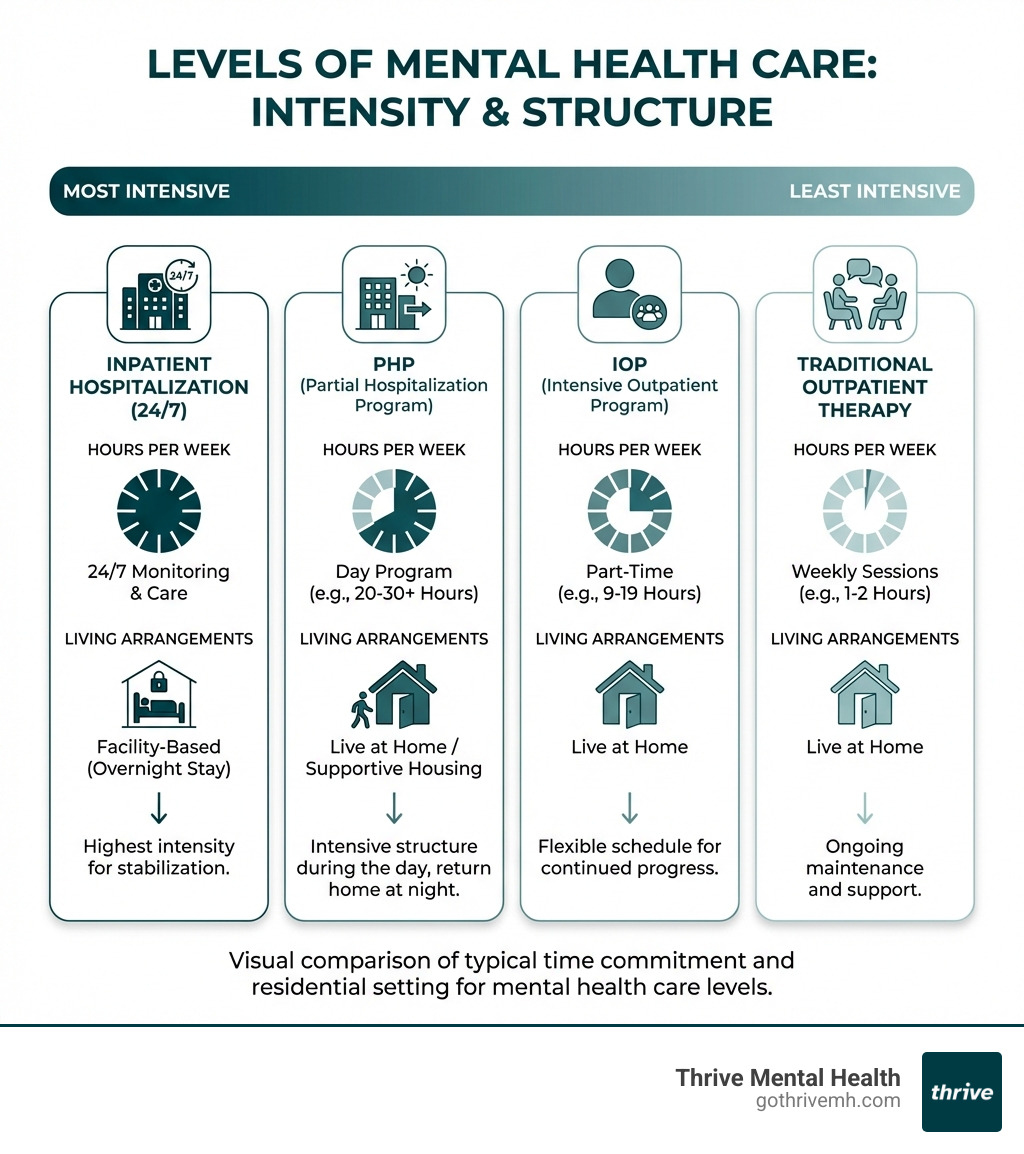
A Partial Hospitalization Program (PHP) is the most intensive form of outpatient care, providing structured therapy for several hours a day, five days a week, while you continue to live at home. Think of it as a powerful middle ground: it offers more support than traditional outpatient therapy but doesn’t require the overnight stay of inpatient care. Understanding the key differences between IOP and PHP is crucial for choosing the right level of care. PHPs are ideal for individuals who need a “step-down” from inpatient care to continue their recovery, or a “step-up” from less intensive outpatient programs when symptoms worsen or become harder to manage. The goal is to provide comprehensive support, clinical expertise, and measurable results, designed for people who need more than once-a-week therapy but less than inpatient care. You can find More info about PHP Mental Health Services on our website.
Yes, UnitedHealthcare (UHC), one of America’s largest health insurance providers, through its subsidiary UnitedHealth Group, typically covers PHPs for medically necessary conditions. This coverage is mandated by federal mental health parity laws, which require mental health benefits to be comparable to physical health benefits. This means if a PHP is deemed medically necessary for your condition, UHC is obligated to cover it, similar to how they would cover a physical health procedure.
What Mental Health Conditions Does UHC Cover for PHP?
UHC plans generally cover PHP for a wide range of mental health conditions and substance use disorders when a higher level of care is deemed necessary. This determination is made based on clinical assessments, which indicate that your symptoms are severe enough to warrant intensive, structured support without requiring 24/7 inpatient supervision.
Here is a list of common diagnoses for which UHC often provides PHP coverage:
- Major Depressive Disorder (MDD): For individuals experiencing severe depressive episodes that impair daily functioning.
- Post-Traumatic Stress Disorder (PTSD): When trauma-related symptoms are significantly impacting a person’s life and require intensive therapeutic intervention.
- Obsessive-Compulsive Disorder (OCD): For severe OCD symptoms that are resistant to less intensive treatments.
- Bipolar Disorder: To stabilize mood episodes and provide comprehensive support during acute phases or for relapse prevention.
- Anxiety Disorders: Including generalized anxiety disorder, panic disorder, and social anxiety disorder, when symptoms are debilitating.
- Substance Use Disorders (SUD): For individuals needing intensive support to overcome addiction, often as a step-down from detox or inpatient rehab. UHC generally provides coverage for substance use disorder PHPs, including for alcohol use disorder (AUD) and opioid use disorder (OUD).
- Dual Diagnosis (Co-occurring Substance Use and Mental Health Disorders): When a person experiences both a mental health condition and a substance use disorder simultaneously, PHPs can offer integrated treatment.
UHC’s coverage extends to specialized services within PHPs, such as dual diagnosis care and medication management, which are crucial for many individuals seeking intensive treatment.
What Therapies Are Covered in a UHC-Approved PHP?
UHC focuses on covering treatments with proven effectiveness, meaning your covered PHP will likely incorporate evidence-based therapies delivered by a multidisciplinary team. These therapies are designed to help you manage symptoms, develop coping skills, and improve overall functioning.
Your UHC-approved PHP will likely include a mix of the following therapeutic components:
- Individual Therapy: One-on-one sessions with a licensed therapist to address personal challenges, trauma, and develop individualized coping strategies.
- Group Therapy: A cornerstone of PHP, providing a supportive environment where you can connect with peers, share experiences, and learn from others facing similar challenges. Group therapy helps assure patients they are not alone in their thoughts, feelings, and circumstances.
- Cognitive Behavioral Therapy (CBT): A highly effective approach that helps you identify and change negative thought patterns and behaviors that contribute to mental health issues.
- Dialectical Behavior Therapy (DBT): Often used for individuals with intense emotional dysregulation, DBT teaches skills in mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness. You can learn more about Understanding Insurance Coverage for Dialectical Behavior Therapy: Blue Cross Blue Shield vs. UnitedHealthcare.
- Medication Management: Psychiatric consultations with a psychiatrist or psychiatric nurse practitioner to assess the need for medications, manage existing prescriptions, and monitor their effectiveness.
- Family Therapy: Sessions involving family members to improve communication, resolve conflicts, and build a stronger support system, especially encouraged in adolescent programs.
- Experiential Therapies: Depending on the program, this might include movement therapy, music therapy, art therapy, or mindfulness training to help you express emotions and develop self-awareness.
- Educational Workshops: Sessions focused on understanding mental health conditions, relapse prevention, stress management, and healthy lifestyle choices.
These comprehensive approaches ensure that you receive holistic care addressing your mind, body, and spirit, leading to more sustainable recovery.
Your 5-Step Guide to Find a Partial Hospitalization Program That Is Covered by United Health Company Insurance
When you’re ready to take the courageous step of seeking PHP treatment, navigating insurance can feel like another hurdle. But with a clear strategy, you can confidently find a partial hospitalization program that is covered by United Health Company insurance. Choosing a UHC-accepting PHP facility means you’ll likely benefit from lower out-of-pocket costs and a smoother billing process, as the provider is already familiar with UHC’s specific procedures and requirements.
Step 1: Verify Your Specific UHC Benefits & Coverage
This is your crucial first move. Don’t assume anything; verify everything. While UHC generally covers PHPs, the specifics of your plan—like deductibles, copayments, and coinsurance—can vary significantly.
To verify your benefits:
- Log in to your myuhc.com account or use the UnitedHealthcare mobile app. Your member portal is a goldmine of information, including your plan documents and summary of benefits.
- Call the member services number located on the back of your UnitedHealthcare ID card. This is often the most direct way to get personalized information. When you call, ask specifically about your “behavioral health benefits” for “partial hospitalization programs.” Inquire about:
- Your remaining deductible.
- Your copayment amount for PHP services.
- Your coinsurance percentage for PHP.
- Whether prior authorization is required (it almost always is for PHP).
- Your in-network and out-of-network benefits for PHP.
- Understand your benefits: If you have a United Healthcare Mental Wellness plan, it’s designed to make mental health care accessible.
For more general information on UHC’s mental health services, refer to their official page: UHC Mental Health Services.
Step 2: Understand the Prior Authorization Process
Prior authorization is a critical step for intensive treatments like PHP. It’s UHC’s way of confirming that the treatment is medically necessary and appropriate for your condition. Without it, even if your plan covers PHP, you could be responsible for the full cost.
Here’s how it generally works:
- Medical Necessity: Your potential PHP provider will conduct an assessment to determine if a PHP is the most appropriate level of care for your needs. This assessment forms the basis of the “medical necessity” argument.
- Provider Submission: Once you choose a PHP provider, their admissions team will typically handle the prior authorization request. They will submit comprehensive clinical documentation to UHC on your behalf, outlining your diagnosis, symptoms, treatment history, and why a PHP is medically necessary.
- Approval Process: UHC reviews this documentation. This process determines if your treatment will be covered. Providers experienced with UHC, like Thrive Mental Health, understand the nuances of this process and can effectively advocate for your coverage.
You can find more information about UHC’s prior authorization requirements on their provider portal: UHC Prior Authorization Requirements.
Step 3: How to find a partial hospitalization program that is covered by United Health Company insurance near you.
Now that you understand your benefits and the authorization process, it’s time to locate a suitable PHP. This step is about finding facilities that are not only clinically excellent but also in-network with your UHC plan and conveniently located in Florida.
- Use the UHC Provider Directory: The most reliable way to find a partial hospitalization program that is covered by United Health Company insurance is through the provider search tool on myuhc.com. Filter your search by “behavioral health” and “partial hospitalization program.” Crucially, ensure you select facilities that are “in-network” to maximize your benefits and minimize out-of-pocket costs.
- Localize your search: Filter your search to Florida, focusing on our service areas like Tampa Bay, Miami, Orlando, and Jacksonville.
- Consider Virtual PHP Options: For many, virtual PHP offers flexibility and accessibility, especially if in-person options are limited. Many UHC plans now cover virtual PHP programs. Thrive Mental Health offers Virtual Partial Hospitalization Programs designed for people who need intensive support but benefit from receiving care from the comfort of their own home.
- Use National Resources: While not specific to UHC, the SAMHSA National Helpline (Substance Abuse and Mental Health Services Administration) offers a confidential treatment locator that can help you find partial hospitalization services near you. Once you have a list, cross-reference them with your UHC provider directory.
- Contact the Facilities Directly: Once you have a list of potential PHPs, contact their admissions or intake department. They can confirm their in-network status with your specific UHC plan and often offer to verify your benefits on your behalf, streamlining the process.
Step 4: Estimate Your Potential Out-of-Pocket Costs
Understanding your potential financial responsibility upfront can prevent surprises. Your out-of-pocket costs will depend on your specific UHC plan’s structure.
Key terms to remember:
- Deductible: The amount you must pay out-of-pocket for covered services before your insurance plan starts to pay.
- Copayment (Copay): A fixed amount you pay for a covered health service after you’ve paid your deductible.
- Coinsurance: Your share of the costs of a covered health care service, calculated as a percentage (e.g., 20%) of the allowed amount for the service, after you’ve paid your deductible.
- Out-of-Pocket Maximum: The most you have to pay for covered services in a plan year. After you reach this amount, your health plan pays 100% of the costs of covered benefits.
The national average cost for PHP without insurance can be upwards of $12,000, but with UHC, your portion will be significantly less, especially once you’ve met your deductible. An in-network provider’s admissions team can give you a detailed estimate based on your verified benefits and discuss any potential payment plans for your portion.
What to Do if Your UHC Claim for PHP Is Denied

A claim denial can be disheartening, but it’s crucial to remember that a denial is not the final word. Many initial denials can be overturned with persistence and the right information.
Here’s what to do if your UHC claim for PHP is denied:
- Understand the Denial Reason: UHC is required to send you an Explanation of Benefits (EOB) and a denial letter outlining the specific reason for the denial. This might be due to a lack of medical necessity, missing information, or an administrative error. Read this letter carefully.
- Gather Supporting Documentation: Work closely with your PHP provider. They will have access to your clinical records, which are vital for an appeal. Ensure all documentation supporting the medical necessity of PHP is comprehensive and clearly outlines why this level of care is essential for your condition.
- Initiate an Internal Appeal: You have the right to an internal appeal, which means UHC will review its own decision. Your provider can often submit this appeal on your behalf, often including a “peer-to-peer review” where your treating clinician can speak directly with a UHC medical reviewer to explain the clinical rationale. This is a powerful tool, as it allows for direct communication between medical professionals.
- Request an External Review: If your internal appeal is denied, you have the right to request an external review. This involves an independent third party, not affiliated with UHC, reviewing your case and making a decision. This level of appeal is often successful if the medical necessity is clear.
- Seek Advocacy: Organizations specializing in mental health advocacy or legal aid can provide assistance with navigating complex insurance appeals.
Persistence is key. Your health and well-being are worth fighting for.
Frequently Asked Questions about UHC and PHP Coverage
How long will UnitedHealthcare cover a Partial Hospitalization Program?
The duration of UHC coverage for a Partial Hospitalization Program is based on medical necessity. While the typical length of a PHP can vary, UHC generally authorizes treatment in weekly increments. This means your clinical team will provide regular updates to UHC to justify your continued stay. The total length of treatment often lasts for several weeks, depending on your individual progress and clinical needs. Our programs at Thrive Mental Health are designed to be short-term and intensive, aiming for effective stabilization and skill-building within a focused timeframe.
Does UnitedHealthcare cover virtual PHP programs?
Yes, many UnitedHealthcare plans now cover virtual PHP programs. Telehealth has become a standard and accessible option for mental health care, significantly expanding access to intensive treatment. This is especially important given that 3 million providers offer behavioral health services, but 60% of them cannot accept new patients. Virtual PHPs offer the same structured, evidence-based therapies as in-person programs but with the convenience of receiving care from home. It’s always best to verify with your specific UHC plan to confirm your telehealth benefits, as coverage can vary.
How do I find a partial hospitalization program that is covered by United Health Company insurance for a teenager?
The process for finding a partial hospitalization program that is covered by United Health Company insurance for a teenager is similar to that for an adult. You’ll start by verifying the teen’s specific UHC benefits and checking for prior authorization requirements. When using the UHC provider directory, filter your search by “adolescent” or “teen” programs. Many facilities specialize in treating adolescents, offering age-appropriate therapies and support for issues like depression, anxiety, trauma, and co-occurring disorders. Studies on partial hospitalization programs for adolescents have shown significant benefits, including reduced symptom severity and improved relational health over time.
Get the UHC-Covered Care You Deserve
You’ve learned what a PHP is, how UHC covers it, and the exact steps to find a partial hospitalization program that is covered by United Health Company insurance. Don’t let insurance confusion be a barrier to getting the intensive support you need. The right PHP can be a transformative experience, offering the structure and clinical care necessary to steer significant mental health challenges.
At Thrive Mental Health, we understand the complexities of insurance and are committed to making evidence-based treatment accessible. Our admissions teams are dedicated to navigating the insurance process for you, ensuring you can focus on your recovery. We are in-network with UHC in Florida, offering both virtual and in-person PHP options customized to your needs in locations like Tampa Bay, Miami, Orlando, and Jacksonville.
Ready for support? Thrive offers virtual and hybrid IOP/PHP programs with evening options. Verify your insurance in 2 minutes (no obligation) → Start your benefits check now or call 561-203-6085. If you’re in crisis, call/text 988.