Cheat Sheet to United Health Intensive Mental Health Options

UHC Intensive Mental Health Care: 5 Steps to Hope
Your UHC Plan Covers Intensive Mental Health Care—Here’s How to Use It
If weekly therapy isn’t enough, your UnitedHealthcare (UHC) plan provides a lifeline to more intensive mental health support. You have options beyond once-a-week sessions, especially when you need structured care to manage severe symptoms or transition from a hospital stay.
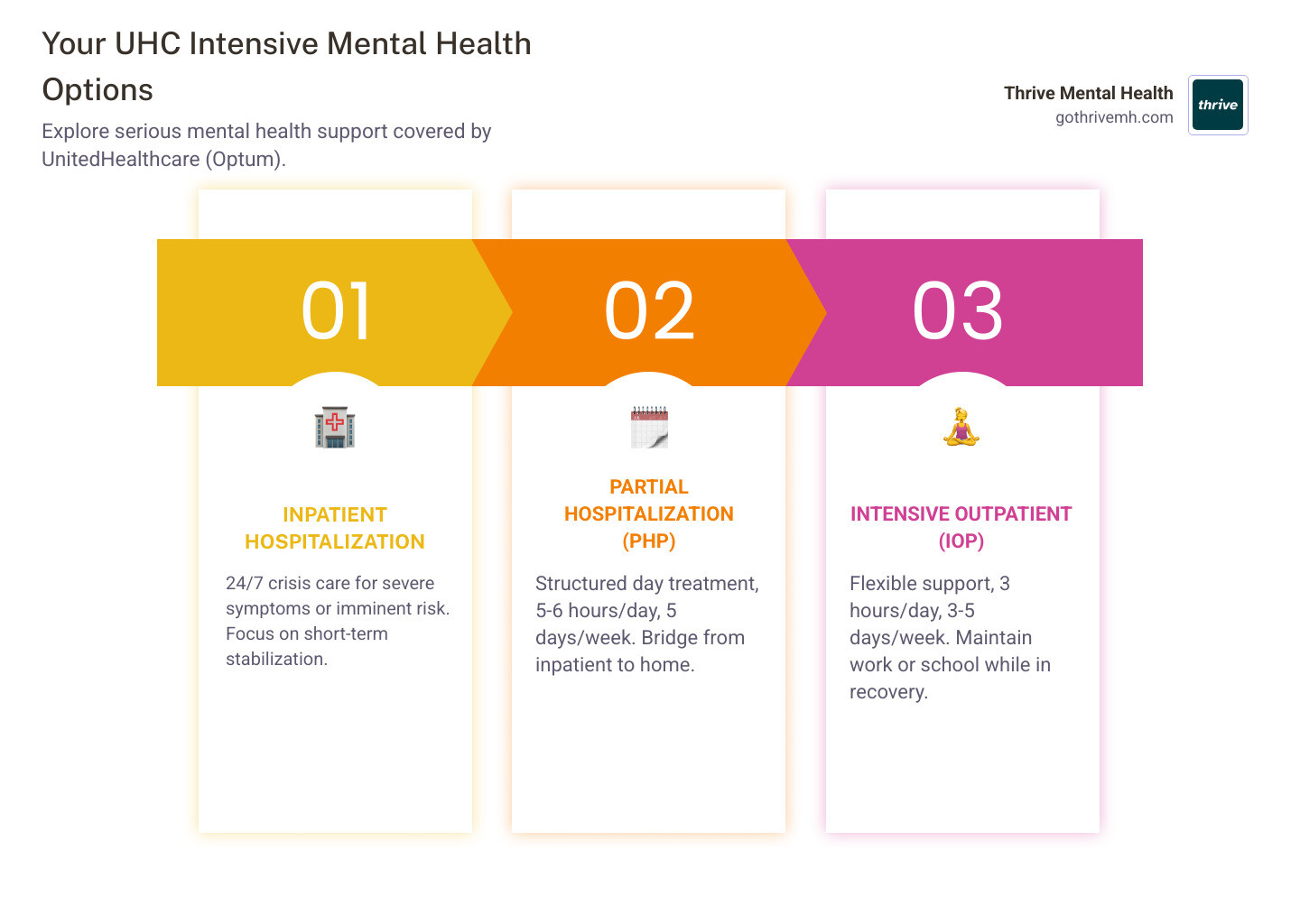
Your UnitedHealthcare plan covers several intensive mental health options:
- Inpatient Hospitalization – 24/7 crisis care for severe symptoms or imminent risk.
- Partial Hospitalization Program (PHP) – 5-6 hours/day, 5 days/week; structured day treatment.
- Intensive Outpatient Program (IOP) – 3 hours/day, 3-5 days/week; fits around work or school.
- Outpatient Therapy & Psychiatric Services – Weekly sessions and medication management for ongoing support.
All of these services are managed through Optum (also called United Behavioral Health), UHC’s behavioral health subsidiary. Your coverage depends on your specific plan, medical necessity, and finding an in-network provider.
The key is knowing how to steer your benefits and get care approved—and this guide will show you how.
I’m Nate Raine, CEO of Thrive Mental Health. We help people with UHC plans understand their options for intensive care. Then, we deliver flexible, outcomes-driven IOP and PHP programs that get results.
Is Weekly Therapy Not Enough? Signs You Need a Higher Level of Care
Call or text 988 for the Suicide & Crisis Lifeline if you are experiencing emotional distress or suicidal thoughts. You are not alone.
Sometimes, once-a-week therapy just isn’t enough. That’s not a failure—it’s a signal that you need more intensive support. Think of it like this: you wouldn’t treat a broken leg with a weekly ice pack. When mental health symptoms become severe, you need a higher level of care.
How do you know you’ve reached that point? Here are the clearest signs:
- Daily life is unmanageable: You’re struggling to get to work, keep up with basic hygiene, or manage responsibilities that used to be easy. This isn’t laziness; it’s a clinical indicator.
- Symptoms aren’t improving: Despite months of therapy, the depression, anxiety, or mood swings aren’t letting up. It’s time to increase the intensity of treatment, not blame yourself.
- You feel yourself sliding downhill: You might not be in crisis today, but you can feel yourself heading there. An intensive program can provide support before you need hospitalization.
- You’re leaving inpatient care: Going from 24/7 support to one weekly session is a recipe for relapse. A PHP or IOP program bridges this critical gap.
- Your environment is harmful: If your home or social life is chaotic or unsupportive, an intensive program offers a structured, safe alternative.
- You’re having thoughts of self-harm: Even without a plan, persistent thoughts of harming yourself mean your current level of care isn’t enough.
If you recognize yourself in these signs, you’re already doing the right thing by seeking information. The next step is to verify your UHC benefits and find a program that fits your life. For a deeper look at behavioral health signs, check out mentalhealth.gov’s guide on what to look for.
If you are in severe distress or having suicidal thoughts right now, please stop reading and call or text 988 for the Suicide & Crisis Lifeline. Immediate, 24/7 support is available.
What Intensive Mental Health Care Does UnitedHealthcare Actually Cover?
Your UnitedHealthcare plan is required by law (thanks to the Mental Health Parity and Addiction Equity Act) to cover mental health care just as it does physical health. All behavioral health benefits are managed by Optum (also called United Behavioral Health), UHC’s subsidiary. This means your coverage for intensive programs is based on medical necessity—proof that you need this level of care to stabilize and recover.
Your plan also covers co-occurring disorders, providing integrated treatment for both mental health and substance use challenges. Let’s break down the levels of care.
Inpatient Hospitalization: 24/7 Crisis Stabilization

This is the highest level of care, designed for acute crises where you are at imminent risk of harm to yourself or others. It provides 24/7 medical supervision in a secure facility for rapid stabilization. Treatment is short-term (typically a few days to a week), with the goal of transitioning you to a lower level of care once the immediate crisis has passed.
Partial Hospitalization Programs (PHP): The Bridge from Inpatient to Home
PHP is a structured day program that acts as a bridge from inpatient care or an alternative to it. You attend treatment for 5-6 hours a day, 5 days a week, while living at home. It combines intensive individual and group therapy, skill-building, and psychiatric oversight to prevent relapse and build a foundation for long-term recovery. At Thrive Mental Health, our virtual PHP programs for adults offer this rigorous support with the flexibility of attending from home.
Intensive Outpatient Programs (IOP): Real-World Recovery with Robust Support

IOP provides structured, evidence-based treatment without taking over your life. It typically involves 3 hours of treatment per day, 3-5 days a week, allowing you to maintain work, school, or family commitments. The focus is on building real-world coping skills through a combination of individual and group therapy. Thrive Mental Health offers virtual IOPs for Florida residents, with evening options available.
| Level of Care | Intensity | Hours/Week (Approx.) | Best For | UHC Coverage Goal |
|---|---|---|---|---|
| Inpatient | Highest: 24/7 supervision, medical monitoring | 168 | Acute psychiatric crises, imminent risk of harm, severe functional impairment. | Short-term stabilization of acute symptoms and ensuring safety. |
| PHP | High: Structured day treatment | 25-30 | Stepping down from inpatient, severe symptoms not manageable by outpatient care. | Providing intensive daily support to prevent relapse and build coping skills. |
| IOP | Moderate-High: Flexible, structured | 9-15 | Needing more than weekly therapy, maintaining work/school, developing coping skills. | Offering structured treatment that integrates into daily life to prevent escalation. |
| Outpatient Therapy | Low: Weekly or bi-weekly sessions | 1-2 | Mild to moderate symptoms, ongoing support, and maintenance. | Supporting long-term mental health management for stable individuals. |
The key to getting any of these programs covered is proving medical necessity. Your provider will document why you need this specific level of care to get better.
How to Get Your UHC Plan to Approve Intensive Care: A 4-Step Guide
Getting intensive mental health care approved by UnitedHealthcare requires a clear process. While a good provider like Thrive Mental Health will handle the administrative work for you, understanding these steps puts you in control.
Step 1: Verify Your Specific UHC Mental Health Benefits

First, know your exact coverage. Call the behavioral health number on your Member ID card (this connects you to Optum) or log into your member account on myUHC.com. Ask these key questions:
- Does my plan cover Partial Hospitalization (PHP) and Intensive Outpatient (IOP) programs?
- Is pre-authorization required for these services?
- What are my in-network providers in Florida?
You can also download the UnitedHealthcare app for quick access to your plan details.
Step 2: Understand Your Costs: Deductibles, Copays, and Coinsurance
Even with great insurance, you’ll have some out-of-pocket costs. Understanding them upfront prevents surprises.
- Deductible: The amount you pay for covered services before your insurance starts paying.
- Copay: A fixed amount you pay for a service (e.g., $40 per session).
- Coinsurance: A percentage of the cost you pay after your deductible is met (e.g., you pay 20%, insurance pays 80%).
- Out-of-Pocket Maximum: The absolute most you’ll pay in a plan year.
Staying in-network is critical. In-network providers have contracts with UHC/Optum, which means significantly lower costs for you. Going out-of-network can cost double or triple, and HMO plans often won’t cover it at all outside of an emergency.
Step 3: Find a Provider That Offers IOP or PHP
Now, find a clinically excellent provider that accepts your insurance. Start with the UHC provider search tool, filtering specifically for “Intensive Outpatient Program” or “Partial Hospitalization Program.” Since Optum manages these benefits, their directory is also a key resource.
Call providers directly to confirm they accept your specific UHC plan and have openings. If you can’t find a suitable in-network option, ask UHC for a “network gap exception.” This allows you to see an out-of-network provider at in-network rates if their network is inadequate.
Step 4: The Pre-Authorization (Prior Auth) Process Explained
For intensive care like IOP and PHP, UHC requires pre-authorization to confirm the treatment is medically necessary. Your chosen provider handles this for you. They submit clinical documentation—your diagnosis, symptoms, and functional impairment—to UHC/Optum to justify the need for a higher level of care.
This is where working with an experienced provider makes a difference. They know what insurers need for approval. If a request is denied, don’t panic. Your provider can help you appeal the decision.
Your UHC Intensive Care Roadmap: 5 Steps to Take Today

Navigating your UnitedHealthcare benefits for intensive care can feel complex, but you now have the knowledge to get the support you need. Here is your simple action plan.
- Assess Your Need: Be honest. Is weekly therapy not working? If your daily functioning is impaired or symptoms are persistent, it’s time for a higher level of care like IOP or PHP.
- Verify Your Benefits: Call the behavioral health number on your UHC card. Ask directly about your specific coverage for Intensive Outpatient and Partial Hospitalization programs.
- Find an In-Network Provider: Use the UHC provider search tool to find an in-network IOP or PHP program. Thrive Mental Health offers virtual programs across Florida and is in-network with most UHC/Optum plans.
- Let Them Handle Pre-Authorization: A quality provider’s admissions team will manage the pre-authorization paperwork with UHC/Optum on your behalf.
- Confirm Your Costs: Before starting, ask the provider for a clear estimate of your out-of-pocket costs, including your deductible and any copays or coinsurance.
We built Thrive Mental Health to simplify this process. Our team verifies your benefits, handles pre-authorization, and gets you into an evidence-based program that fits your life. You’ve already taken the hardest step by seeking answers. Now, it’s time to act.
Frequently Asked Questions about UHC and Intensive Mental Health Care
Here are clear, simple answers to the most common questions about using your UnitedHealthcare plan for intensive mental health treatment.
Does UnitedHealthcare use a different company for mental health?
Yes. UHC manages all behavioral health benefits, including IOP and PHP, through its subsidiary, Optum (also known as United Behavioral Health). When searching for care, you must find providers who are in the Optum network.
How many therapy sessions does UnitedHealthcare cover?
Most modern UHC plans do not use arbitrary session limits. Instead, continued coverage for intensive programs like IOP or PHP is based on “medical necessity.” As long as your provider documents that you are benefiting from treatment and still require that level of care, your treatment will be covered.
What if I can’t find an in-network IOP or PHP provider near me?
This is a common problem in some areas. If the Optum network is inadequate near you, you can request a “network gap exception” or a “single-case agreement” from UHC. If approved, this allows you to see an out-of-network provider at your in-network cost. This is especially useful for accessing high-quality virtual programs when local options are limited.
Ready for Real Support? Here’s Your Next Step.
At Thrive Mental Health, we’ve built our virtual and hybrid IOP/PHP programs for adults who need more than once-a-week therapy. We offer evening options so you can get care without derailing your life, and our programs are led by expert clinicians focused on measurable results.
We serve clients across Florida, and we’re in-network with most major insurance plans, including UnitedHealthcare/Optum. Our team handles the insurance process so you can focus on getting better.
Ready for support? Thrive offers virtual and hybrid IOP/PHP programs with evening options. Verify your insurance in 2 minutes (no obligation) or call 561-203-6085. If you’re in crisis, call/text 988.