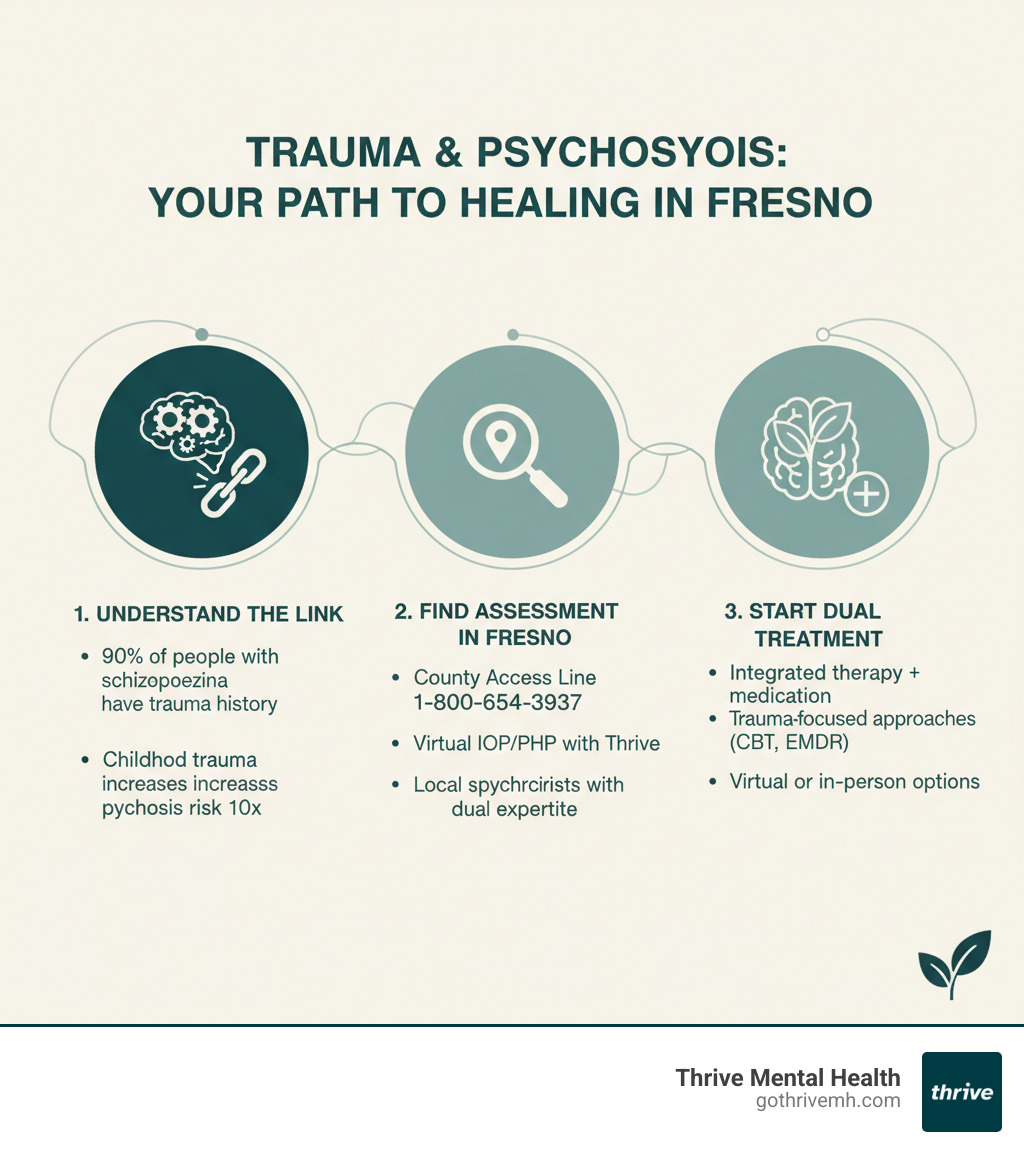
3 Critical Steps to Find Trauma & Schizophrenia Assessment in Fresno

Worried? 3 Critical Steps: Trauma & Schizophrenia Fresno
Why Trauma and Schizophrenia Are More Connected Than You Think
I’m worried about the link between trauma and schizophrenia. Where can I find an assessment program in Florida? Here’s what you need to know right now:
Quick Answer: 3 Places to Start Your Assessment in Florida
- Florida’s 2-1-1 Network – Dial 2-1-1 (24/7) for immediate screening and referrals to local assessment programs and crisis support.
- Thrive Mental Health – Virtual IOP/PHP programs for Florida residents with trauma-informed psychosis assessment (no waitlist, insurance accepted).
- Local Psychiatrists & Testing Centers – Search Psychology Today’s directory for Florida providers specializing in “trauma” + “schizophrenia/psychosis”.
You’re right to be worried. The research is clear and scary: up to 90% of people with schizophrenia have a history of trauma. Childhood trauma can increase your risk of developing psychosis by up to 10 times.
This isn’t just correlation. Trauma literally changes how your brain develops and responds to stress. It can trigger psychotic symptoms in people who are already vulnerable. And ignoring the trauma while treating the psychosis? That’s like putting a band-aid on a broken bone.
The good news: early assessment saves lives. When you catch the trauma-psychosis connection early and treat both together, recovery happens faster and symptoms improve more.
But here’s the problem most people face in Florida: finding a provider who actually understands both trauma and schizophrenia. Not just one or the other. You need someone who gets how they feed each other—and how to treat them as a team.
I’m Nate Raine, CEO of Thrive Mental Health, and I’ve spent over a decade building systems that connect people to evidence-based mental health care when they need it most. At Thrive, we’ve helped hundreds of Floridians steer the exact question I’m worried about the link between trauma and schizophrenia. Where can I find an assessment program in Florida?—and we know what works.
This guide walks you through 3 critical steps to get a real assessment, fast. No fluff. No waitlists. Just a clear path to help.
I’m worried about the link between trauma and schizophrenia. Where can I find an assessment program in Florida? terms to learn:
- Why Betrayal Trauma Feels Like PTSD (And What You Can Do About It)
- bilateral stimulation exercises for trauma
- mental health centers in miami that specialize in trauma therapy for adults
Step 1: Know the Real Risk—How Trauma Fuels Schizophrenia
Trauma isn’t just a past event; it actively rewires your brain and can set the stage for psychosis. When you’re thinking I’m worried about the link between trauma and schizophrenia. Where can I find an assessment program in Florida?, you’re connecting dots that could save your life.
Research shows individuals with severe trauma are up to 10 times more likely to develop schizophrenia. This isn’t a small statistical blip—it’s a massive red flag.
Childhood trauma disrupts brain development, altering the parts that handle emotional regulation and stress response. It’s like your brain’s wiring gets scrambled during its most critical construction phase. Studies show that between 50% and 90% of people with schizophrenia have a trauma history, making trauma-informed assessment essential.
This is often explained by the “diathesis-stress” model. Some people have a genetic vulnerability to schizophrenia (the diathesis), but it may not manifest without a trigger. Severe trauma can be that trigger, pushing a vulnerable person into psychosis.
Here’s the danger: ignoring trauma means missing the root cause. When doctors only treat psychotic symptoms without addressing the underlying trauma, you’re getting half the treatment. Many symptoms that look like “pure” schizophrenia—paranoia, dissociation, even some hallucinations—can be direct manifestations of past trauma. If your treatment team doesn’t understand that connection, you’ll struggle longer than you need to.
[Internal Link: Learn more about trauma’s impact on mental health → How to Overcome Trauma]
What symptoms should you watch for if you’ve had trauma?
If you have a history of trauma and are experiencing these symptoms, it’s time to get help. The lines between trauma response and psychosis blur, which is why a professional assessment is critical.
- Paranoia and hypervigilance: A constant feeling of being unsafe or watched. This is a classic trauma response but also a psychotic symptom.
- Hallucinations tied to past trauma: Hearing voices or seeing images related to a traumatic event. These vivid “flashbacks” can blur the line between PTSD and psychosis.
- Social withdrawal and isolation: Pulling away from everyone due to fear, distrust, or feeling overwhelmed. Both trauma and early schizophrenia can drive you into isolation.
- Disorganized thinking under stress: Thoughts become jumbled or illogical when pressure hits. Trauma impacts cognitive function, but this is also a hallmark sign of emerging psychosis.
- Emotional numbness or outbursts: Swinging between feeling completely detached and having sudden, intense emotional explosions. Trauma and schizophrenia both dysregulate emotions.
- Loss of motivation and joy (anhedonia): Nothing feels good anymore, and you can’t find the motivation to do anything. This is common in severe trauma and is also a debilitating negative symptom of schizophrenia.
Recognizing these signs early is your first line of defense. Early, trauma-informed intervention can change the trajectory of your life.
Step 2: Find a Florida Assessment Program That Gets Both Trauma & Psychosis
When you’re thinking “I’m worried about the link between trauma and schizophrenia. Where can I find an assessment program in Florida?”, you need a team that understands both conditions. Many providers specialize in trauma or schizophrenia, but not both. That gap can mean the difference between effective treatment and staying stuck.
Look for “trauma-informed” and “dual diagnosis” specialists. A trauma-informed approach means the provider understands how trauma impacts your brain and won’t accidentally re-traumatize you. Dual diagnosis specialists treat co-occurring conditions like schizophrenia and PTSD at the same time.
Outpatient psychiatric evaluations are a good first step. Psychiatrists in Florida can conduct diagnostic evaluations to create a treatment roadmap. For more support, consider Intensive Outpatient Programs (IOP) and Partial Hospitalization Programs (PHP). These programs offer structured, intensive treatment while you live at home. At Thrive Mental Health, our virtual IOP and PHP programs are designed for adults with complex needs like co-occurring trauma and psychosis.
Crucially, you’re not limited to physical locations in Florida. Virtual assessment and treatment mean you can access expert care from anywhere in Florida. This is a huge advantage if you struggle with paranoia or social anxiety. At Thrive, we offer virtual IOP and PHP with no waitlist, and we accept most major insurance. You can get a trauma-informed psychosis assessment from home, often starting in days.
How do you find the right provider in Florida?
- Use online directories like Psychology Today. Filter for psychiatrists in Florida who list both “Trauma and PTSD” and “Schizophrenia & psychosis” as specialties.
- Ask directly: “Do you offer trauma-informed care for psychosis?” A provider who can clearly explain their integrated approach is a good fit.
- Verify credentials. Look for licensed therapists and psychiatrists (MDs, PMHNPs, LCSWs, LMFTs) with dual-diagnosis experience.
- Contact Florida resources. Dialing 2-1-1 is a key access point for local services. You can also contact your regional managing entity for substance abuse and mental health services, or reach out to your local NAMI Florida chapter for guidance.
- Consider the Baker Act. For individuals who may be a danger to themselves or others due to mental illness, Florida’s Baker Act provides a civil court process for involuntary examination and stabilization.
[Internal Link: See Thrive’s IOP and PHP programs in Florida → Intensive Outpatient Programs | Partial Hospitalization Program (PHP)]
How to Pay: Insurance and Costs in Florida
Cost is a major concern, but you have options. Most PPO plans (Aetna, Cigna, Blue Cross Blue Shield, Optum) cover assessment and treatment for mental health. Florida Medicaid is also accepted at many programs. If you don’t have insurance, many providers offer private pay options or sliding scale fees.
Always verify your benefits before starting. Understand your deductible, copays, and session limits. We can help you check your coverage in about 2 minutes with no obligation.
[Internal Link: Check your insurance coverage now → Insurance Policy]
Step 3: Get Ready for Your Assessment—And What Happens Next
A real assessment is a roadmap to recovery. Knowing what to expect can ease some of the anxiety you’re feeling.
Your first appointment—whether in-person in Florida or virtual—will start with a clinical interview. A provider will ask about your symptoms, trauma history, and family mental health background to see the full picture. Many trauma-informed programs also use screening for Adverse Childhood Experiences (ACEs) to understand risk factors.
You’ll likely go through diagnostic tools for psychosis, which are standardized tests to confirm a diagnosis. Good clinicians will also rule out other causes, such as medical conditions or substance use that can mimic psychotic symptoms.
The best assessments involve both a psychiatrist and a therapist working together. The psychiatrist handles medication, while the therapist provides psychotherapy, ensuring both trauma and psychosis are addressed as a team.
What treatment options are available for trauma and schizophrenia in Florida?
After your assessment, you’ll get a personalized treatment plan. If you’re asking “I’m worried about the link between trauma and schizophrenia. Where can I find an assessment program in Florida?”, you also need to know what comes next.
- Integrated care—therapy plus medication—is the gold standard. Antipsychotic medication helps manage psychotic symptoms, while therapy addresses the underlying trauma and builds coping skills.
- Trauma-focused therapies are crucial. These include Cognitive Behavioral Therapy (CBT) to change negative thought patterns, Eye Movement Desensitization and Reprocessing (EMDR) to process distressing memories, and Somatic Experiencing (SE) to release trauma stored in the body.
- Medication management for psychosis is overseen by a psychiatrist who monitors your progress and minimizes side effects.
- Virtual IOP and PHP programs offer flexible, high-level care. At Thrive Mental Health, our programs provide more structure than weekly therapy without requiring you to leave your home in Florida. We offer evening options and accept most major insurance.
Local options in Florida include Assertive Community Treatment (ACT) programs, which provide comprehensive, community-based services for adults with serious mental illness. These are often accessed through your region’s managing entity.
[Internal Link: Learn about Thrive’s evidence-based trauma treatment → Evidence-Based Trauma Treatment]
Why you can’t wait: The cost of ignoring early signs
Every week you wait, the risk grows. Untreated trauma and psychosis lead to a higher risk of crisis, hospitalization, and disability. Symptoms worsen, and brain changes can become more entrenched, making recovery harder.
But the opposite is also true: early intervention means faster recovery, fewer symptoms, and a better life. The sooner you get help, the better your prognosis. Don’t let fear stop you from getting the assessment you need now.
How to Support a Loved One in Crisis in Florida

Watching a loved one struggle with trauma and potential psychosis is heartbreaking and scary. It’s normal to fear saying the wrong thing, which is why understanding how to be an effective supporter is so important.
- Listen without judgment. When your loved one shares experiences that sound paranoid or confusing, resist the urge to correct them. Their experiences are real to them. Acknowledge their pain without criticism to create a safe space.
- Encourage professional help—don’t try to “fix” it alone. Your role is to guide them toward people who can help. Dialing or texting 988 connects you to the national crisis line for immediate support. NAMI Florida also offers excellent family support groups across the state.
- Help with logistics. The mental health system is complex. Offer practical support by making phone calls, verifying insurance, or arranging transportation to appointments. These small acts can remove huge barriers.
- Set boundaries to protect your own mental health. Supporting someone with severe mental health challenges is exhausting. You can’t help if you’re drowning. Find your own therapist, join a support group, and take breaks. Self-care isn’t selfish; it’s essential for the long haul.
If you’re in crisis, call/text 988 right now. You are not alone. This applies to you, too. Caregiver burnout is real, and reaching out for support is a sign of strength.
FAQs: Trauma & Schizophrenia Assessment in Florida
You’re serious about getting answers. Here are straight answers to the questions people actually ask when they’re worried about trauma and schizophrenia.
Can trauma cause schizophrenia?
Trauma is a major risk factor, not a direct cause. It can trigger the onset of schizophrenia in people who are already genetically vulnerable. Think of it as genetics loading the gun and trauma pulling the trigger. Research shows that severe trauma increases the risk up to 10 times. This is why finding an assessment program in Florida is so critical for anyone worried about the link between trauma and schizophrenia.
What is trauma-informed care for psychosis?
It’s an approach that recognizes trauma is often central to psychosis. A trauma-informed provider creates safety, avoids triggering interventions, and treats both the trauma and psychotic symptoms together. It’s integrated care that sees the whole person, not just a diagnosis. This is the standard of care you should look for in an assessment program.
Are virtual assessments for trauma and schizophrenia effective?
Yes, and they are often more comfortable for those dealing with paranoia or social anxiety. Virtual Intensive Outpatient (IOP) and Partial Hospitalization (PHP) programs are proven effective for assessing and treating complex, co-occurring conditions. At Thrive Mental Health, our virtual programs offer privacy, flexibility, and expert care from your home in Florida.
Does insurance cover trauma and schizophrenia assessment in Florida?
Yes, most major PPO insurance plans (like Aetna, Cigna, Blue Cross Blue Shield, and Optum) cover assessment and treatment in Florida. Florida Medicaid also covers services through the state’s behavioral health system. Always verify your specific benefits before starting. At Thrive, you can verify your insurance coverage in about 2 minutes.
How fast can I start treatment?
With Thrive Mental Health, you can often start in days. We’ve eliminated waitlists for our virtual IOP and PHP programs because we know every day matters when you’re struggling. Local Florida programs may have longer wait times, but statewide resources like the 988 Crisis Line and 2-1-1 can provide immediate screening and referrals.
Summary: Don’t Wait—Get Trauma & Schizophrenia Assessment in Florida Now
If you’re asking, “I’m worried about the link between trauma and schizophrenia. Where can I find an assessment program in Florida?”, don’t wait. The connection is real and treatable, with up to 90% of people with schizophrenia having a trauma history. While Florida has local resources available through community mental health centers and regional managing entities, access to specialists who understand both conditions can be limited, with long wait times.
This is where virtual IOP and PHP programs make a real difference. At Thrive Mental Health, we offer immediate access to expert, trauma-informed psychosis care from your home in Florida. Our programs combine therapy and medication management with no waitlist. Getting the right assessment isn’t just about a diagnosis; it’s about a plan that treats both issues together. Don’t let another week go by—the risk grows with delay, but recovery starts with action.
[Internal Link: Learn more about Thrive’s virtual therapy options → Virtual IOP]
Ready for support? Thrive offers virtual and hybrid IOP/PHP programs with evening options. Verify your insurance in 2 minutes (no obligation) → Start benefits check. If you’re in crisis, call/text 988.