Insurance & PHP: What You Need to Know About Your Benefits

Why Understanding Your PHP Coverage Matters More Than You Think
Does your insurance cover a partial hospitalization program? Here’s what you need to know right now:
Quick Answer:
- Yes, most plans do — thanks to the Affordable Care Act (ACA) and Mental Health Parity laws
- Medical necessity is required — your doctor must certify you need this level of care
- Pre-authorization is common — most insurers require approval before you start
- Medicare Part B covers 80% after deductible (when criteria are met)
- Medicaid coverage varies by state — Florida offers coverage
- Private insurance (Cigna, Optum, Florida Blue, etc.) typically covers PHP when medically necessary
- Cost without insurance: $300–$1,500 per day — potentially $10,000–$30,000+ for a full program
If you’ve been told you need a Partial Hospitalization Program (PHP), your first thought is probably: “Can I afford this?” It’s a valid concern. PHP treatment is intensive—20+ hours per week of structured therapy, psychiatric care, and support. But here’s the good news: most insurance plans are required by law to cover mental health and substance use treatment at the same level as medical care.
The problem? Figuring out exactly what your plan covers, how much you’ll pay, and what hoops you need to jump through can feel like a full-time job. Insurance companies use terms like “medical necessity,” “pre-authorization,” and “out-of-network penalties” that leave most people confused and stressed.
You shouldn’t have to choose between getting help and avoiding financial disaster.
This guide will walk you through exactly how to verify your PHP coverage, what questions to ask your insurer, and what to do if you hit a roadblock. Whether you have private insurance, Medicare, Medicaid, or TRICARE—or even if you’re uninsured—we’ll show you the path forward.
I’m Nate Raine, CEO of Thrive Mental Health, and I’ve spent over a decade helping people steer the intersection of mental health care and insurance systems. Understanding does your insurance cover a partial hospitalization program is critical to accessing the right level of care without surprise bills, and I’ve built Thrive to make that process transparent and stress-free.
Related content about does your insurance cover a partial hospitalization program:
- Find a partial hospitalization program that is covered by United Health Company insurance.
- partial hospitalization program
What is a PHP and Is It Right for You?
When we talk about mental health or addiction treatment, there’s a spectrum of care available. On one end, you have traditional outpatient therapy, like weekly individual sessions. On the other, you have inpatient or residential treatment, which involves living at a facility 24/7. A Partial Hospitalization Program (PHP) sits right in the middle, offering a crucial bridge for individuals who need more intensive support than outpatient care but don’t require round-the-clock supervision.
A PHP is a highly structured, intensive outpatient treatment program. It typically involves attending therapy and treatment sessions for at least 20 hours per week, often five days a week, for several hours each day. Unlike inpatient care, clients return home or to a supportive living environment each evening. This model allows individuals to maintain some connection to their daily lives and responsibilities, which can be incredibly beneficial for long-term recovery and integration back into the community. We often refer to PHPs as a “step-down” from inpatient care, helping individuals transition back to daily life, or a “step-up” from traditional outpatient therapy when symptoms become more acute or persistent.
PHPs are recognized by the American Society of Addiction Medicine (ASAM) as a Level 2.5 on their continuum of care, indicating a high level of intensity and structure. They are designed for individuals struggling with severe mental health conditions such as major depression, anxiety disorders, PTSD, bipolar disorder, or eating disorders, as well as substance use disorders. The goal is to stabilize acute symptoms, prevent hospitalization, or reduce the risk of relapse after inpatient treatment.
If you’re wondering if a PHP is right for you, consider if you need a comprehensive, multidisciplinary approach to managing your symptoms, but you also have a relatively stable home environment and don’t pose an imminent danger to yourself or others. For more in-depth information on what a PHP entails and how it supports recovery, you can explore our More info about PHP services. You might also find this scientific research on partial hospitalization insightful for understanding its efficacy.
Services Typically Included in a PHP
PHPs are comprehensive by design, meaning they integrate various therapeutic approaches to address the complex needs of clients. While specific offerings may vary between programs, you can generally expect a robust suite of services, including:
- Individual Therapy: One-on-one sessions with a licensed therapist to dig into personal challenges, develop coping mechanisms, and process emotions.
- Group Therapy: A cornerstone of PHP, these sessions provide a supportive environment for sharing experiences, practicing social skills, and receiving feedback from peers and clinicians.
- Family Counseling: Crucial for building a strong support system, these sessions involve family members to address relational dynamics and educate them on how to best support their loved one’s recovery.
- Medication Management: Oversight by a psychiatrist or other medical professional to prescribe, monitor, and adjust medications as needed, ensuring optimal symptom management.
- Psychiatric Evaluations: Initial and ongoing assessments to diagnose conditions accurately and tailor treatment plans.
- Skills-Building Groups: Focused sessions to teach practical coping strategies, such as dialectical behavior therapy (DBT) skills for emotional regulation and distress tolerance, cognitive behavioral therapy (CBT) techniques for challenging negative thought patterns, or relapse prevention strategies for substance use disorders.
- Case Management: Support with coordinating care, navigating resources, and addressing practical needs like housing, employment, or legal issues.
In our Florida-based programs, we integrate these services with evidence-based practices to ensure a holistic and effective treatment experience.
Does Your Insurance Cover a Partial Hospitalization Program? [The Short Answer]
The good news is that for most people seeking mental health or addiction treatment in a Partial Hospitalization Program, the answer is a resounding yes, most plans do offer some level of coverage. This isn’t just luck; it’s largely due to significant legislative efforts designed to ensure equitable access to mental healthcare.
Under the Affordable Care Act (ACA), all rehab insurance coverage (except grandfathered plans) must offer mental health and substance use disorder services as one of the ten essential health benefits. This means that plans offered through the HealthCare.gov Marketplace, for example, cannot cap the amount of substance use or mental health treatment covered.
Even more impactful is the Mental Health Parity and Addiction Equity Act (MHPAEA). This law mandates that if an insurance plan offers mental health and substance use disorder benefits, they must be comparable to the medical and surgical benefits offered. This means your copay, deductible, and out-of-pocket maximum for a PHP should be similar to what you’d pay for a medical hospitalization or specialist visit, for example. The MHPAEA ensures that insurance companies can’t impose more restrictive limits on mental health care than they do on physical health care.
However, “coverage” doesn’t always mean 100% free. The primary hurdle you’ll encounter is medical necessity. Your insurance company will require a licensed medical professional (typically a psychiatrist or physician) to certify that a PHP is the appropriate level of care for your condition. This involves a formal diagnosis and documentation that your symptoms are severe enough to warrant intensive treatment, and that less intensive options would be insufficient or that you require this level of care to prevent inpatient hospitalization or relapse. This is especially true for co-occurring disorders, where both a mental health condition and a substance use disorder are present.
Additionally, pre-authorization is common. Many insurers require approval before you even begin a PHP. This step is critical and often where delays or denials can occur if not handled correctly. We’ll dive into how to manage this crucial step shortly.
Finally, whether a program is in-network versus out-of-network will significantly impact your out-of-pocket costs. In-network providers have agreements with your insurance company, leading to lower costs for you. Out-of-network providers may still be covered, but usually at a lower percentage, leaving you with a larger bill. Major private insurers like Florida Blue, Cigna, and Optum typically have networks of PHP providers across Florida.
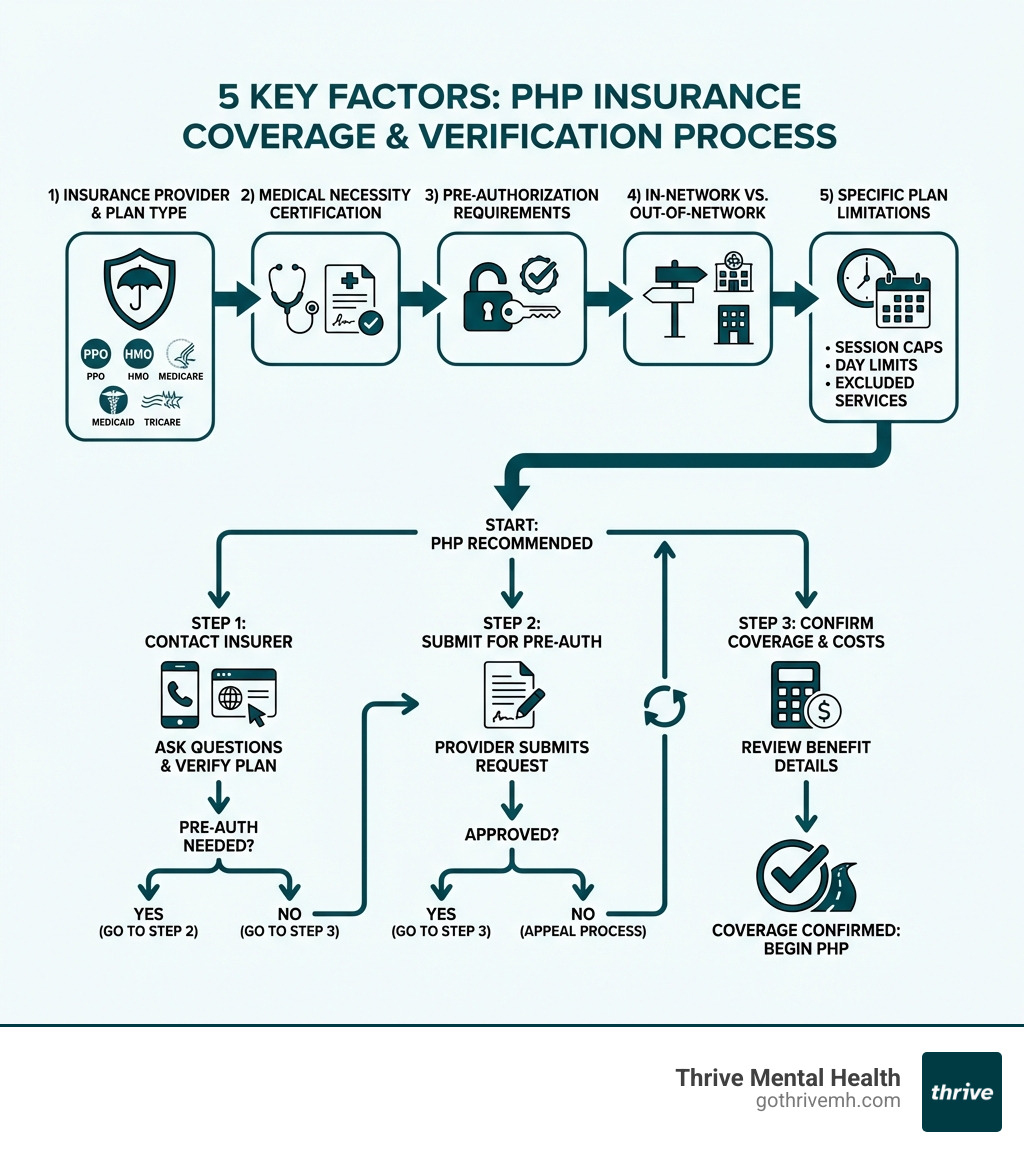
Your 5-Step Guide to Verifying PHP Benefits & Avoiding Surprise Bills
Navigating the complexities of insurance coverage for mental health treatment can feel like trying to solve a Rubik’s Cube blindfolded. But trust us, it’s not impossible! This is the most critical part of the process. By following these steps, you can get a clear answer to does your insurance cover a partial hospitalization program and avoid those dreaded surprise bills.

Step 1: Find Your Plan’s “Behavioral Health” Benefits
Your first mission is to locate your Summary of Benefits and Coverage (SBC). This document, often available through your insurance company’s online portal or mailed to you, provides a high-level overview of your plan’s coverage. Look specifically for sections related to “Mental Health Services” or “Behavioral Health.” You’ll want to see if “Partial Hospitalization” is explicitly listed. If not, don’t despair—it might be covered under a broader category.
Step 2: Call Your Insurer and Ask These 5 Questions
This is where you become an insurance detective. Call the member services number on the back of your insurance card. Be prepared with your member ID, group number, and the name of the PHP program you’re considering. We recommend asking these specific questions, taking detailed notes of the representative’s name, call reference number, and date/time of the call:
- Is pre-authorization required for PHP (CPT Code H0035)? This is a critical question. PHP services are typically billed using CPT Code H0035. Knowing if pre-authorization is required and what the process entails is essential.
- What is my remaining deductible and out-of-pocket maximum? Your deductible is the amount you pay before your insurance starts contributing. Your out-of-pocket maximum is the most you’ll pay in a policy year for covered services. Knowing these numbers helps you budget.
- What is my copay or coinsurance for in-network PHP? A copay is a fixed amount, while coinsurance is a percentage of the cost after your deductible is met. Ask for both for in-network providers.
- Are there limits on the number of days or sessions covered? Some plans have annual limits, such as 30 days per year for PHP, or may cap sessions per week or month. It’s better to know this upfront.
- Can you confirm [Provider Name] is in-network? Even if a provider claims to be in-network, always double-check with your insurer to prevent discrepancies.
Step 3: Understand Coverage Differences: Private vs. Government Plans
The specifics of does your insurance cover a partial hospitalization program can vary significantly depending on whether you have private insurance, Medicare, or Medicaid.
- Private Insurance (e.g., Florida Blue, Cigna, Optum): These plans, common in Florida, generally cover PHPs when medically necessary.
- PPO vs. HMO plans: PPO (Preferred Provider Organization) plans offer more flexibility, allowing you to see out-of-network providers at a higher cost. HMO (Health Maintenance Organization) plans usually require you to stay within their network, often needing a referral from a primary care physician. Always verify the specific rules of your plan.
- Medicare Part B: Yes, Medicare Part B covers partial hospitalization programs for mental health treatment. However, it comes with specific requirements:
- A doctor must certify that you need PHP, either to avoid inpatient treatment or to prevent relapse after discharge.
- You must receive services from a Medicare-approved facility.
- Medicare requires a plan showing you need at least 20 hours per week of services.
- Medicare Part B covers 80% of approved costs after the deductible, meaning you’ll be responsible for the remaining 20% coinsurance. Your State Health Insurance Assistance Program (SHIP) can provide more information on Medicare coverage.
- Medicaid: Medicaid coverage depends on your state. However, most states, including Florida, offer PHP for mental health or addiction. Coverage criteria and the extent of services can vary, so it’s crucial to check with your state’s Medicaid office or your specific plan for details. Pre-approval and session limits may apply.
- TRICARE: TRICARE covers PHP for both mental health and substance use disorders. You must use an authorized provider, but pre-authorization is generally not required for PHP services. TRICARE outlines specific medical necessity criteria, similar to other insurers, to ensure the PHP is appropriate for your condition.
Step 4: Get Pre-Authorization If Required
If your insurer requires pre-authorization (and many do), this step is non-negotiable. It’s your official “permission slip” from the insurance company. Here’s what it typically involves:
- Medical Necessity Letter: Your doctor or the PHP facility will submit a letter outlining your diagnosis, symptoms, and why a PHP is medically necessary for your recovery. This letter should explain why less intensive treatment isn’t sufficient.
- Clinical Assessment: Detailed assessment results that support the need for PHP.
- Treatment Plan Submission: The PHP will provide a comprehensive treatment plan, detailing the services you’ll receive, the expected duration, and treatment goals.
Always get an authorization number in writing before starting the program. This number is your proof that your services are approved. Without it, you risk significant out-of-pocket costs.
Step 5: Know the Common Exclusions and Limitations
Even with coverage, there can be fine print. Being aware of common exclusions and limitations can save you from unexpected bills.

- Session Limits / Day Limits: Your plan might have annual limits, such as 30 days per year for PHP, or limits on the number of sessions per week or month. Once these limits are reached, you’ll be responsible for the full cost.
- Non-Covered Services: While PHPs are comprehensive, certain services are typically not covered by insurance. These often include:
- Meals provided during the program.
- Transportation to and from the facility.
- General support groups that are not led by licensed therapists or considered group psychotherapy.
- Non-mental health related job skills training or vocational rehabilitation.
- Out-of-Network Penalties: If you choose an out-of-network PHP, your plan may cover a much smaller percentage, or not at all, leading to significantly higher out-of-pocket expenses.
What to Do If Your PHP Claim is Denied (Or You’re Uninsured)
It can feel incredibly frustrating, even devastating, if your insurance denies coverage for a PHP. But don’t panic! A denial isn’t always the final word. Many denials are due to clerical errors or insufficient documentation.
Common Denial Reasons:
- Clerical Error: Incorrect billing codes, missing information, or a simple oversight.
- Not Medically Necessary: The insurer believes your condition doesn’t meet their specific criteria for PHP, or that a less intensive treatment would suffice.
- Lack of Pre-Authorization: You started the program without getting prior approval.
- Exceeded Limits: You’ve used up your plan’s annual or session limits.
The Appeals Process:
If your claim is denied, you have the right to appeal. The denial letter should explain why your claim was denied and how to appeal.
- Internal Appeal: Start by filing an internal appeal with your insurance company. This involves submitting a written request, often with additional documentation from your doctor or the PHP facility, explaining why the PHP is medically necessary. Provide any new information or clarify existing details.
- External Review: If your internal appeal is denied, you can often request an external review. This means an independent third party, not affiliated with your insurance company, will review your case. This step is particularly powerful, as the external reviewer’s decision is usually binding.
- Know Your Rights: The ACA and MHPAEA protect your right to mental health coverage. Referencing these laws in your appeal can strengthen your case. SAMHSA provides valuable information on your rights to coverage (PDF | 2.2 MB).
Options for Uninsured Individuals:
If you don’t have insurance or your plan simply won’t cover a PHP, hope is not lost. Many programs and organizations offer financial assistance:
- Sliding-Scale Fees: Some PHP facilities offer fees based on your income, making treatment more affordable.
- Payment Plans: Many centers will work with you to set up a manageable payment schedule.
- Grants and Scholarships: Non-profit organizations and some treatment centers offer grants or scholarships to help cover treatment costs.
- Community Mental Health Centers: These centers often provide services at a reduced cost or can connect you with resources for financial aid.
Don’t let financial barriers prevent you from getting the help you need. There are resources and options available.
Frequently Asked Questions about PHP Insurance Coverage
How do I prove a PHP is “medically necessary” to my insurance?
Medical necessity is proven with a formal diagnosis from a licensed clinician, documentation that less intensive care (like weekly therapy) is insufficient, and a treatment plan showing how PHP will address acute symptoms to prevent hospitalization or relapse. This documentation typically comes from your referring physician or the PHP’s clinical team. They’ll outline your symptoms, functional impairments, and how the structured, intensive nature of PHP is uniquely suited to your needs.
Will my insurance cover a virtual PHP?
Coverage for virtual PHPs has expanded significantly. Most major insurers, including Cigna, Optum, and Florida Blue, now cover virtual programs, but you must confirm this with your specific plan as policies can vary. Given the success of online therapy and treatment programs, especially for substance use disorders, many insurance companies have adapted their policies. Thrive Mental Health offers virtual PHPs across Florida, and we are in-network with most major insurance providers, making it easier to access care from the comfort of your home.
What’s the difference in coverage between a PHP and an IOP?
Both PHPs and Intensive Outpatient Programs (IOPs) are typically covered under “behavioral health benefits,” but the reimbursement rates and pre-authorization requirements may differ. PHPs are more intensive (20+ hours/week) and may have higher daily reimbursement rates but stricter medical necessity criteria than IOPs (9-15 hours/week). Essentially, a PHP is a higher level of care than an IOP, and insurance coverage reflects this difference in intensity and cost. Always verify coverage for both if you’re considering either option.
What are the typical out-of-pocket costs for a PHP with insurance?
Even with insurance coverage, you will likely have some out-of-pocket costs. These typically include:
- Deductible: The amount you must pay out-of-pocket before your insurance plan starts to pay.
- Copay: A fixed amount you pay for each PHP session or day after your deductible is met.
- Coinsurance: A percentage of the cost you pay for services after your deductible is met (e.g., if your plan covers 80%, you pay 20%).
- Out-of-Pocket Maximum: The most you’ll have to pay for covered services in a plan year. Once you hit this limit, your insurance typically pays 100% of covered costs.
These costs vary greatly by plan, so it’s crucial to ask your insurer about them directly (see Step 2 above).
Get the Help You Need—Without the Financial Guesswork
Understanding does your insurance cover a partial hospitalization program requires a few strategic steps, but getting a clear answer is possible. By understanding your plan, asking the right questions, and knowing your rights, you can access high-quality care with confidence. Thrive Mental Health is in-network with most major insurance providers, and our team is here to make the process seamless.
Ready for support? Thrive offers virtual and hybrid IOP/PHP programs with evening options. Verify your insurance in 2 minutes (no obligation) → Start benefits check or call 561-203-6085. If you’re in crisis, call/text 988.