Blue Cross Michigan: Your Path to Intensive Outpatient Support

Why Finding IOP Programs In-Network with Blue Cross and Blue Shield of Michigan Changes Everything
IOP programs in-network with Blue Cross and Blue Shield of Michigan offer a lifeline when weekly therapy isn’t enough, but you’re not ready for a hospital stay. You need more structure and support, but you can’t afford surprise medical bills or take a month off work.
Here’s the good news: Blue Cross Blue Shield of Michigan covers Intensive Outpatient Programs (IOPs). This means you can get 9–15 hours of therapy per week while living at home, keeping your job, and paying predictable in-network rates. No hospital stay, no financial ruin.
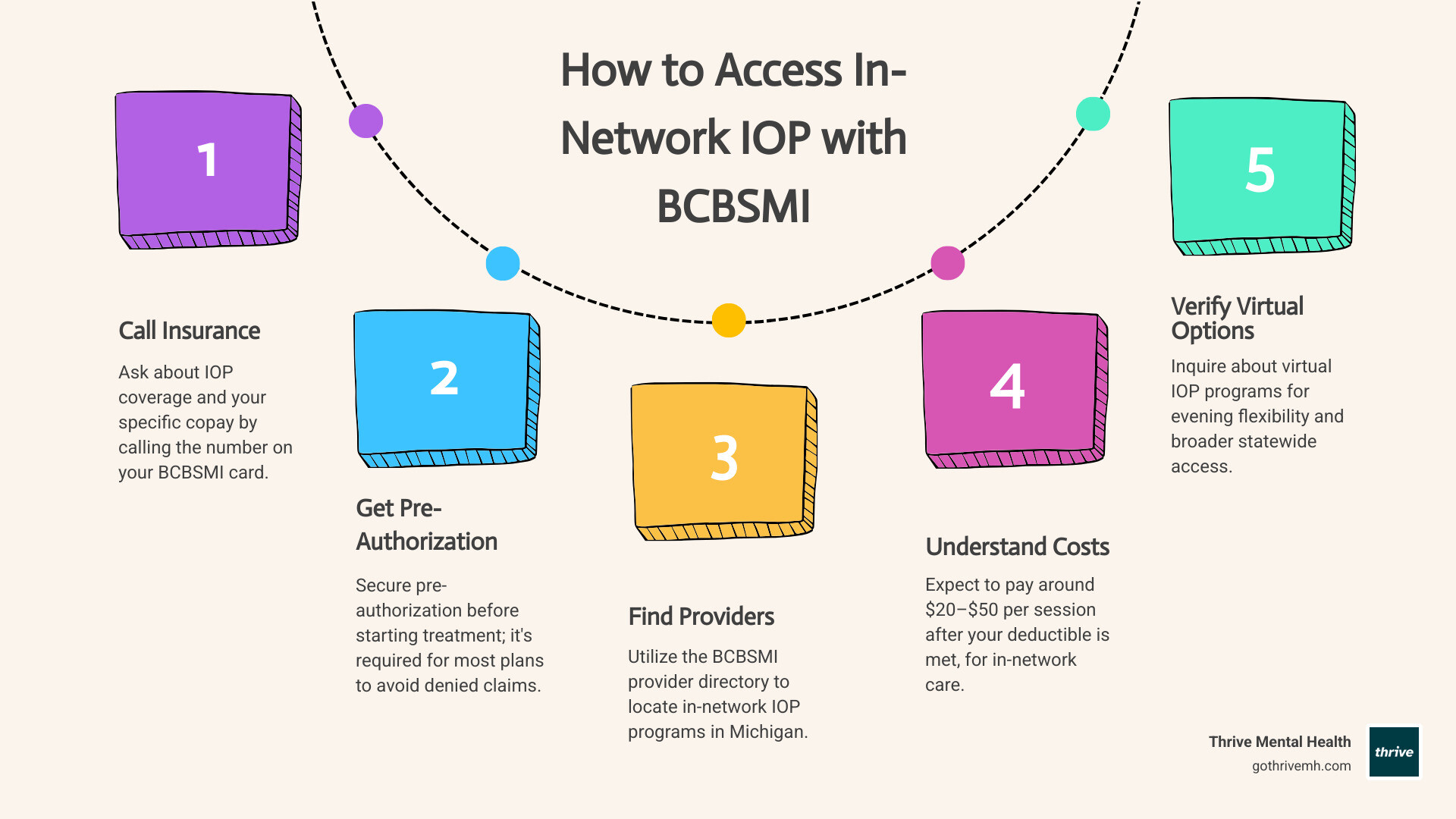
Quick Answer: How to Access In-Network IOP with BCBSMI
- Call your insurance card’s member services number to confirm IOP coverage and copay.
- Get pre-authorization before starting treatment (this is required for most plans).
- Use the BCBSMI provider directory to find in-network programs in Michigan.
- Expect to pay a $20–$50 copay per session after your deductible, compared to $100–$250 out-of-network.
- Verify virtual IOP options for flexible evening schedules and statewide access.
But here’s the catch: choosing the wrong program or skipping pre-authorization can lead to denied claims and thousands in out-of-pocket costs. This guide walks you through the process step-by-step to get the help you need without the surprise bills.
I’m Nate Raine, CEO of Thrive Mental Health. We’ve helped thousands of Michigan residents access evidence-based IOP care—primarily through virtual programs that make treatment accessible from anywhere in the state. We know how to steer BCBSMI coverage to connect you with effective, affordable care.
Stuck? How Michigan Residents Can Get Intensive Help—Without Breaking the Bank
You know you need a higher level of care to make real progress with your mental health or substance use, but the thought of inpatient treatment is overwhelming. Worse, the fear of huge, uncovered medical bills is paralyzing.
This is a common dilemma. You need structured help that fits into your life, not disrupts it. This guide is your roadmap to accessing IOP programs in-network with Blue Cross and Blue Shield of Michigan. We’ll show you how to get intensive support with predictable costs and peace of mind—no more guessing games or unexpected bills.
What Is an IOP? [Intensive Outpatient Program Explained]
An Intensive Outpatient Program (IOP) is a structured treatment program for mental health and substance use. It’s designed for individuals who need more support than weekly therapy but do not require 24/7 supervision in a hospital.
An IOP typically involves 9–15 hours of structured therapy per week, spread across 3-5 days. This model allows you to live at home, keep your job or school commitments, and practice recovery skills in your daily life. It’s an effective step-up from weekly therapy when symptoms worsen or a step-down from inpatient care to transition back to daily life with continued support.
IOPs are effective for a wide range of conditions, including:
- Depression & Anxiety Disorders
- Trauma and PTSD
- Substance Use Disorders
- Bipolar Disorder
- Co-occurring Disorders (mental health and substance use)
- Eating Disorders
![Diverse group therapy session. Alt: “In-network IOP group session in Michigan”]
IOP vs. Other Care: What’s the Difference?
Understanding the levels of care helps you find the right fit. IOP strikes a balance between intensity and flexibility.
Here’s a quick comparison:
| Feature | Standard Outpatient Therapy | Intensive Outpatient Program (IOP) | Partial Hospitalization Program (PHP) |
|---|---|---|---|
| Time Commitment | 1-2 hours/week | 9–15 hours/week (e.g., 3-5 days, 3 hours/day) | 20–30+ hours/week (e.g., 5 days, 6+ hours/day) |
| Living Situation | Lives at home | Lives at home | Lives at home |
| Focus | Ongoing support, individual therapy | Skill-building, group therapy, managing daily life | Stabilization, intensive therapy, structured environment |
| Intensity | Lowest | Medium | High |
Conditions Treated in a Blue Cross Blue Shield of Michigan IOP
Thanks to the Mental Health Parity and Addiction Equity Act (MHPAEA) and the Affordable Care Act (ACA), most BCBSMI plans must cover mental health and substance use disorders at the same level as physical health conditions. This ensures you have coverage for medically necessary treatment.
IOP programs in-network with Blue Cross and Blue Shield of Michigan commonly treat depression, anxiety, trauma, substance use disorders (SUDs), bipolar disorder, and co-occurring disorders. With over 50% of people with a SUD also having a mental illness, integrated treatment that addresses both is critical for better outcomes. You can learn more about your behavioral health rights from the Substance Abuse and Mental Health Services Administration (SAMHSA) here.
Blue Cross Blue Shield of Michigan: What’s Covered, What’s Not
Blue Cross Blue Shield of Michigan (BCBSMI) plans are generally comprehensive for behavioral health. Due to federal laws like the Mental Health Parity Act, if your plan covers medical care, it must also cover medically necessary mental health treatment like IOP.
The biggest factor for your wallet is the difference between in-network and out-of-network care.
- In-Network: The provider has a contract with BCBSMI, agreeing to their rates. You pay only your deductible, copay, or coinsurance. This means lower, predictable costs and no surprise bills.
- Out-of-Network: The provider has no contract. You may have to pay the full fee upfront and seek partial reimbursement. You could also be “balance billed” for the difference between the provider’s fee and what BCBSMI pays, leading to thousands in unexpected costs.
Choosing IOP programs in-network with Blue Cross and Blue Shield of Michigan is the smartest financial decision.
![Blue Cross Blue Shield of Michigan insurance card. Alt: “BCBSMI card for in-network IOP coverage”]
What Will You Pay? [Real Numbers]
With an in-network IOP, your costs are transparent. They typically include:
- Deductible: The amount you pay before insurance coverage begins.
- Copay: A fixed fee per session after your deductible is met. For in-network BCBSMI plans, this is often around $20–$50 per session.
- Coinsurance: A percentage of the cost you pay after meeting your deductible.
- Out-of-Pocket Maximum: The most you will pay for covered services in a plan year. Once you hit this limit, your plan pays 100%.
Example: If your plan has a $1,000 deductible and a $20 copay, you’d pay the full session cost until the $1,000 is met, then just $20 per session thereafter. This is far more affordable than paying $150+ per session out-of-network.
Note: Pre-authorization from BCBSMI is almost always required before starting IOP services. Without it, claims will be denied. If you’re unsure about your coverage, we can help. Verify your insurance in 2 minutes with Thrive Mental Health.
PPO vs. HMO: How Your Plan Changes Your Options
Your BCBSMI plan type affects how you access care. Here are the common types:
- PPO (Preferred Provider Organization): Offers the most flexibility. You can see in-network or out-of-network providers without a referral, but your costs will be lowest with in-network providers.
- HMO (Health Maintenance Organization): Generally only covers care within its network. You will likely need a referral from your primary care physician (PCP) to see specialists, including for IOP.
- EPO (Exclusive Provider Organization): A hybrid plan that only covers in-network care (like an HMO) but usually doesn’t require a referral to see specialists (like a PPO).
Always call the number on your insurance card to verify your specific plan’s rules for IOP coverage, copays, and referrals.
How to Find In-Network IOP Programs with Blue Cross Blue Shield of Michigan [4 Steps]
Follow these four steps to find the right IOP programs in-network with Blue Cross and Blue Shield of Michigan and avoid financial surprises.
![Person calling insurance provider. Alt: “Michigan resident verifying IOP coverage with Blue Cross Blue Shield”]
Step 1: Call the Number on Your BCBSMI Card
This is your most important first step. Call the member services number on the back of your insurance card to get accurate information about your specific plan. Ask these key questions:
- “Does my plan cover Intensive Outpatient Programs (IOP)?”
- “What is my copay or coinsurance for in-network IOP?”
- “What is my remaining deductible?”
- “Is pre-authorization required for IOP?”
Step 2: Get Pre-Authorization Before Starting
This step is non-negotiable. Pre-authorization is required for most BCBSMI plans for behavioral health services. Skipping it will result in denied claims, even if the program is in-network.
Once you choose an IOP, their intake team will usually handle the pre-authorization request. However, it is your responsibility to confirm with both the provider and BCBSMI that approval has been granted before you begin treatment. Keep a record of your authorization number.
Step 3: Use the BCBSMI Provider Finder Tool
BCBSMI offers an online “Find a Doctor” or “Provider Finder” tool on its website. Use it to search for contracted providers in your area.
- Log in to your member account for the most accurate results.
- Filter your search for “Intensive Outpatient Program” or “Behavioral Health.”
- Enter your Michigan zip code to find local options.
This tool will generate a list of facilities that are genuinely in-network with your plan.
Step 4: Ask About Virtual IOP for Maximum Flexibility
Virtual care has made mental health treatment more accessible than ever. Many IOP programs in-network with Blue Cross and Blue Shield of Michigan now offer virtual options, which is a game-changer for Michigan residents.
- Statewide Access: Virtual IOP removes geographic barriers, allowing you to access top-tier care from anywhere in Michigan.
- Flexible Scheduling: Programs often offer evening sessions, so you don’t have to miss work, school, or family commitments.
- Insurance Coverage: BCBSMI generally covers telehealth services, including virtual IOP, as long as pre-authorization is obtained.
Thrive Mental Health offers expert-led virtual IOP programs that are in-network with BCBSMI, making our evidence-based care accessible to all Michigan residents. Learn more about Thrive’s virtual IOP.
What Makes a Quality In-Network IOP? [Don’t Settle]
Finding a program that accepts your insurance is just the first step. To get real results, you need a quality program. Don’t settle for less.
A quality IOP should offer:
- Evidence-Based Care: Uses proven therapies like Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT).
- Licensed Clinicians: Staffed by experienced, licensed therapists, psychologists, and psychiatrists.
- Comprehensive Treatment: A mix of individual therapy, group therapy, psychoeducation, and medication management.
- Structured Curriculum: A clear program with defined goals and ways to measure your progress.
- Aftercare Planning: A solid plan to help you maintain progress after you complete the program, with referrals to ongoing support.
- Accreditation: Look for programs accredited by respected bodies like The Joint Commission or designated as a “Blue Distinction® Center” by BCBSMI.
At Thrive Mental Health, our programs are built on these standards to deliver measurable results. See Thrive’s IOP services to learn about our approach.
Why In-Network IOP with Blue Cross Blue Shield of Michigan Is a Game-Changer
Choosing an in-network IOP is a strategic move for a stress-free recovery. Here’s why:
- Lower, Predictable Costs: You pay negotiated rates (copays/coinsurance) and avoid surprise balance billing.
- Vetted Providers: In-network providers meet BCBSMI’s credentialing standards, ensuring a baseline of quality.
- Less Hassle: The provider handles billing and claims directly with the insurer, reducing your paperwork.
- Coordinated Care: In-network providers often work within a system that allows for better communication with your other doctors.
Warning Signs: Avoid These Red Flags
Be vigilant and avoid programs that could compromise your recovery or finances. Watch out for:
- Vague Promises: No clear schedule or unrealistic claims of an “instant cure.”
- Lack of Licensing: The program cannot provide proof of state licensing or accreditation.
- High-Pressure Sales Tactics: Pushing you to commit immediately without time for questions.
- No Aftercare Plan: No discussion of what happens after you complete the IOP.
- Refusal to Discuss Costs: Evasive about pricing or unwilling to help verify your insurance benefits.
FAQs: Blue Cross Blue Shield of Michigan & IOP Programs
Here are some common questions Michigan residents have about accessing IOP programs in-network with Blue Cross and Blue Shield of Michigan.
How much does IOP cost with Blue Cross Blue Shield of Michigan?
For IOP programs in-network with Blue Cross and Blue Shield of Michigan, most members can expect to pay a copay of around $20–$50 per session once their annual deductible has been met. Your total out-of-pocket spending for covered services is capped by your plan’s out-of-pocket maximum, providing financial protection.
Do I need a referral for IOP with my BCBSMI plan?
This depends on your specific BCBSMI plan type. If you have an HMO plan, you will typically need a referral from your primary care physician (PCP) to access IOP services. For PPO or EPO plans, a referral is generally not required, but pre-authorization from BCBSMI is almost always necessary before starting IOP, regardless of the plan type. Always call the number on your insurance card to confirm.
Does Blue Cross Blue Shield of Michigan cover virtual IOP?
Yes, in most cases. Blue Cross Blue Shield of Michigan generally covers virtual IOP services, including phone and video visits, provided that the services are medically necessary and pre-authorized. This allows Michigan residents to access IOP programs in-network with Blue Cross and Blue Shield of Michigan from anywhere in the state, offering incredible flexibility. See Thrive’s virtual options for more information.
Can I use my insurance from other states (Cigna, Optum, Florida Blue, etc.)?
Yes, Thrive Mental Health accepts most major insurance plans, including Cigna, Optum, and various Blue Cross Blue Shield plans from across the country. While this article focuses on Michigan, our virtual and in-person programs are accessible to residents in Florida, California, Indiana, Arizona, and South Carolina, and we work with many different insurance providers to make our evidence-based care accessible. Verify your insurance with us to understand your specific benefits.
How fast can I start IOP after approval?
Once your IOP services have received pre-authorization from Blue Cross Blue Shield of Michigan, you can typically begin treatment very quickly. Most quality programs, including Thrive Mental Health, aim to start clients within 1–5 days after insurance approval, understanding the urgency of getting you the support you need.
Take the First Step—Don’t Wait for a Crisis
If you’re seeking more support than weekly therapy, you’re not alone. For Michigan residents, accessing IOP programs in-network with Blue Cross and Blue Shield of Michigan means you can get fast, affordable, and proven care—whether through a local facility or an expert-led virtual program.
By understanding your BCBSMI benefits, securing pre-authorization, and choosing a quality in-network provider, you can focus on healing. Don’t risk out-of-network bills or low-quality programs. Take control of your mental health journey today.
Explore Thrive’s IOP and PHP programs | Virtual Therapy | Verify Insurance
Related: “How Virtual IOPs Cut Recovery Time by 50%”
Ready for support? Thrive offers virtual and hybrid IOP/PHP programs with evening options. Verify your insurance in 2 minutes (no obligation) → Start benefits check. If you’re in crisis, call/text 988.