Is It CPTSD? A Checklist of 17 Key Symptoms

Introduction: More Than Just Trauma—When the Past Won’t Stay in the Past
What are the 17 symptoms of complex PTSD? If you’re asking this question, you might already recognize that something feels profoundly different about your trauma response. Complex PTSD (C-PTSD) goes beyond the flashbacks and hypervigilance of standard PTSD—it affects how you see yourself, relate to others, and experience emotion itself.
The 17 Core Symptoms of Complex PTSD
- Emotional flashbacks (reliving past feelings without visual memories)
- Difficulty regulating emotions (intense mood swings, uncontrollable anger)
- Persistent feelings of guilt and shame (toxic shame, self-blame)
- Negative self-concept (feeling broken, worthless, or fundamentally damaged)
- Difficulty with relationships (trust issues, fear of abandonment, repeating unhealthy patterns)
- Feeling different or detached from others (persistent loneliness, feeling like an outsider)
- Hypervigilance (always on “high alert,” constantly scanning for danger)
- Exaggerated startle response (jumping at loud noises, extreme reactions to surprises)
- Avoidance of triggers (avoiding people, places, or activities related to trauma)
- Dissociation (feeling detached from reality, depersonalization, memory gaps)
- Chronic sleep disturbances (insomnia, frequent nightmares)
- Self-destructive behaviors (substance abuse, risky behaviors, self-harm)
- Loss of a system of meanings (losing faith, feeling hopeless about the future)
- Somatic symptoms (chronic pain, headaches, digestive issues with no clear medical cause)
- Cognitive difficulties (“brain fog,” problems with concentration and memory)
- Suicidal thoughts (thoughts of ending your life, wishing you were dead)
- Inability to experience positive emotions (emotional numbness, difficulty feeling joy or love)
Complex PTSD develops after prolonged or repeated trauma—not from a single event. Childhood abuse, ongoing domestic violence, captivity, or any situation where escape felt impossible can create this pattern. Studies estimate that C-PTSD affects 1 to 8 percent of the general population, with rates reaching up to 50 percent among individuals seeking mental health care.
Unlike standard PTSD, which typically follows a single traumatic incident like a car accident or natural disaster, C-PTSD emerges from trauma that was repeated, interpersonal, and often began in childhood. The World Health Organization recognized C-PTSD as a distinct diagnosis in the ICD-11, acknowledging that prolonged trauma creates unique disturbances in emotional regulation, self-identity, and relationships.
I’m Nate Raine, CEO of Thrive Mental Health, and over the past decade I’ve worked at the intersection of mental health innovation and evidence-based care, helping thousands of individuals understand what are the 17 symptoms of complex PTSD and find pathways to recovery. At Thrive, we’ve built programs specifically designed to address the full spectrum of C-PTSD symptoms through integrated, trauma-informed care.
Simple what are the 17 symptoms of complex PTSD glossary:
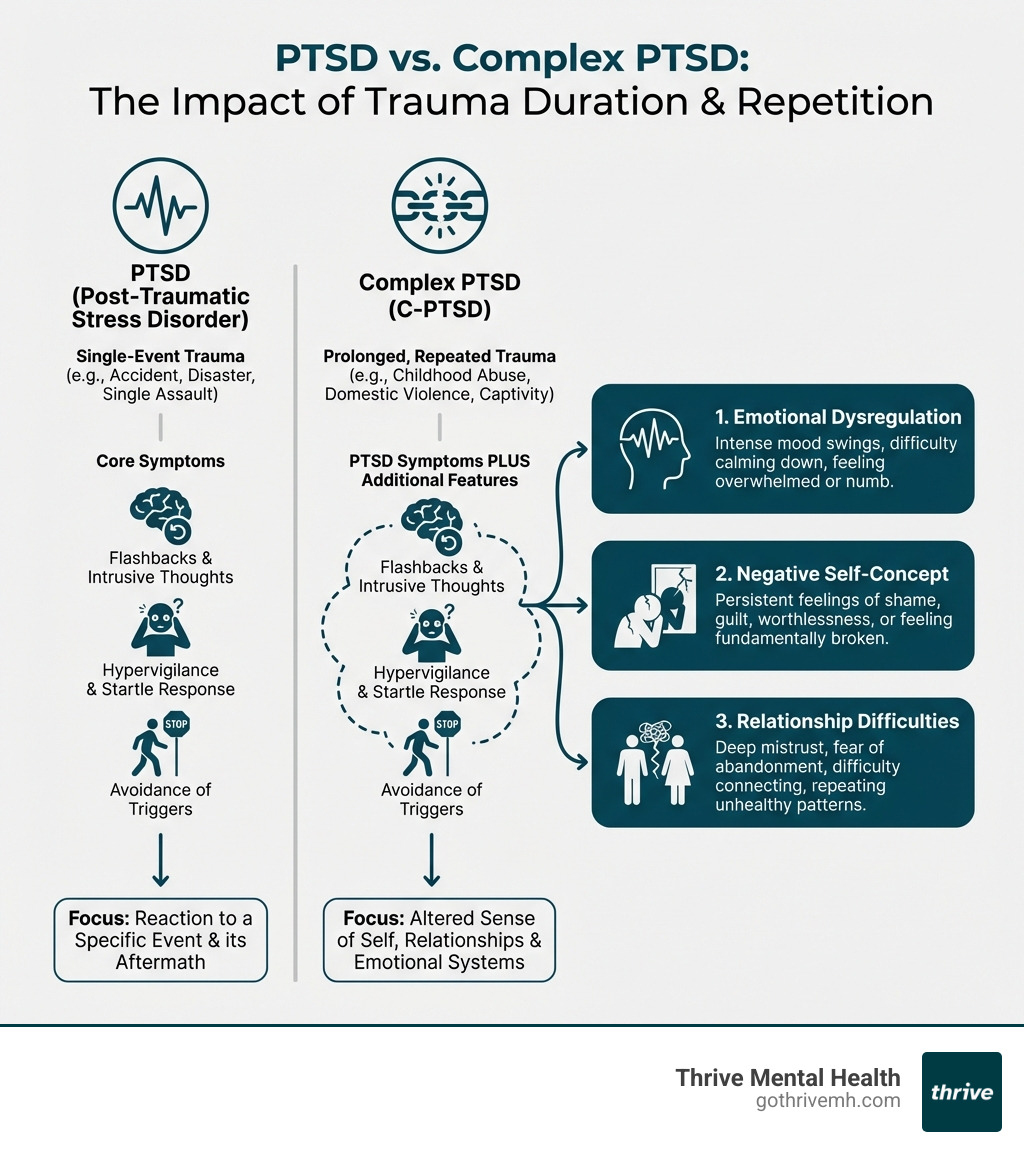
C-PTSD vs. PTSD: Why It’s Not “Just” PTSD
Many people are familiar with Post-Traumatic Stress Disorder (PTSD), often associated with a single, acute event like a car accident, a natural disaster, or a violent attack. However, trauma comes in many forms, and when it’s prolonged, repeated, or occurs in a context where escape feels impossible, it can lead to a different, more complex condition: Complex PTSD (C-PTSD).
The core distinction lies in the nature of the trauma. PTSD typically arises from a single, time-limited traumatic event. C-PTSD, on the other hand, develops from continuous, long-term trauma, such as prolonged childhood abuse or neglect, ongoing domestic violence, human trafficking, or living in a war zone. These experiences, especially when they occur during critical developmental periods like childhood, profoundly impact an individual’s sense of self, their ability to regulate emotions, and their capacity to form healthy relationships.
For example, a child who experiences chronic abuse from a caregiver, or an adult trapped in a domestically violent relationship, faces a different psychological challenge than someone who experiences a one-time traumatic incident. In these prolonged situations, the trauma isn’t just an event; it’s an environment, a way of life that shapes the developing brain and personality. This leads to what clinicians call “disturbances in self-organization”—a cluster of symptoms related to emotional regulation, negative self-perception, and difficulties in relationships, which go beyond the traditional PTSD symptom clusters of re-experiencing, avoidance, and hyperarousal.
The World Health Organization recognized C-PTSD as a distinct diagnosis in 2018 through the ICD-11, acknowledging its unique symptom profile. While it’s not yet formally included as a separate diagnosis in the DSM-5 in the U.S., its unique symptoms are widely accepted by mental health professionals.
Here’s a quick comparison of the key differences:
| Feature | PTSD | C-PTSD |
|---|---|---|
| Type of Trauma | Single, acute event (e.g., car crash, natural disaster) | Prolonged, repeated, interpersonal trauma (e.g., childhood abuse, domestic violence, captivity) |
| Core Symptoms | Re-experiencing, avoidance, hyperarousal, negative thoughts/mood | Core PTSD symptoms PLUS disturbances in self-organization: emotional dysregulation, negative self-perception, and relationship difficulties |
| Impact on Self-Concept | Less direct impact on identity, often related to the event | Deeply ingrained negative self-concept (worthlessness, shame, feeling damaged) |
| Relational Impact | May affect relationships, but not a defining feature | Significant, pervasive difficulties in forming and maintaining relationships, trust issues, fear of abandonment |
What Are the 17 Symptoms of Complex PTSD? A Detailed Checklist
Understanding what are the 17 symptoms of complex PTSD is the first crucial step toward healing. These symptoms are not just isolated reactions; they’re deeply intertwined and impact nearly every aspect of an individual’s life. We’ve categorized them below to help you better recognize their emotional, relational, behavioral, cognitive, and physical manifestations.
1. Emotional Flashbacks
Unlike traditional flashbacks that might involve vivid visual memories, emotional flashbacks in C-PTSD are about reliving the intense feelings associated with past trauma without clear visual cues. This means you might suddenly be flooded with overwhelming fear, shame, helplessness, or terror, feeling as if you are a child again, trapped in the original traumatic moment, even if you can’t pinpoint why.
2. Difficulty Regulating Emotions
This is a hallmark of C-PTSD. Individuals often struggle with intense and rapid mood swings, from uncontrollable anger and irritability to persistent sadness or profound anxiety. It can feel impossible to calm down once upset, leading to a constant sense of being overwhelmed by your own emotional landscape.
3. Persistent Feelings of Guilt and Shame
Trauma, especially prolonged interpersonal trauma, often leaves individuals with a deep, toxic shame. You might feel inherently flawed, damaged, or responsible for the abuse you endured. This self-blame can be incredibly debilitating, leading to a pervasive sense of worthlessness.
4. Negative Self-Concept
C-PTSD can shatter an individual’s sense of self. You might struggle with extremely low self-esteem, feel helpless, or see yourself as fundamentally broken. This can lead to a profound loss of identity, feeling disconnected from who you were before the trauma, and struggling to imagine a positive future self.
5. Difficulty with Relationships
Chronic trauma, particularly when inflicted by trusted figures, severely impacts the ability to form healthy attachments. This can manifest as profound difficulty trusting others, an intense fear of abandonment, avoidance of intimacy, or a tendency to repeat unhealthy relationship patterns. Connecting with others can feel like navigating a minefield.
6. Feeling Different or Detached from Others
A persistent sense of loneliness and feeling like an outsider is common. You might feel that no one truly understands your experience, creating a barrier to genuine connection. This detachment can make it difficult to relate to those who haven’t experienced similar depths of trauma.
7. Hypervigilance (Always on “High Alert”)
Living in a state of constant threat means your nervous system is perpetually activated. You might find yourself constantly scanning your environment for danger, feeling perpetually on edge, and unable to relax. This state of hyper-alertness can be exhausting and make everyday situations feel threatening.
8. Exaggerated Startle Response
Because your nervous system is primed for danger, even minor surprises can trigger an extreme physical reaction. Loud noises, sudden movements, or unexpected touches can cause you to jump, tense up, or experience a rapid increase in heart rate, reflecting a heightened fight-or-flight response.
9. Avoidance of Triggers
To cope with overwhelming emotions and memories, individuals with C-PTSD often develop avoidance behaviors. This includes actively avoiding people, places, activities, or conversations that might remind them of the trauma. Emotional numbness can also be a form of avoidance, where you try to shut down all feelings to escape the pain.
10. Dissociation (Feeling Detached from Reality)

Dissociation is a common coping mechanism for unbearable pain. It can manifest as depersonalization (feeling detached from your own body or thoughts) or derealization (feeling that the world around you isn’t real). You might describe feeling “spaced out,” like you’re watching a movie of your own life, or experience memory gaps related to traumatic events.
11. Chronic Sleep Disturbances
The constant state of hyperarousal and anxiety makes restful sleep incredibly difficult. Insomnia, difficulty falling or staying asleep, and frequent, distressing nightmares are common. Research from the U.S. Department of Veterans Affairs (the VA) has indicated that 71% to 96% of those with PTSD may have nightmares, and this is often even more pronounced in C-PTSD.
12. Self-Destructive Behaviors
To manage overwhelming emotional pain, individuals may engage in self-destructive behaviors. This can include substance abuse (alcohol, drugs) to numb feelings, risky behaviors that put them in danger, self-harm, or disordered eating. These behaviors often start as maladaptive coping mechanisms, providing temporary relief but causing more harm in the long run.
13. Loss of a System of Meanings
Prolonged trauma can shatter an individual’s worldview. You might experience a profound loss of faith (spiritual or in humanity), feel a pervasive sense of hopelessness about the future, or question core beliefs about the goodness of the world or people. This existential crisis can leave you feeling adrift and without purpose.
14. Somatic (Physical) Symptoms
The body “keeps the score” of trauma, as Bessel van der Kolk famously noted. Many individuals with C-PTSD experience chronic physical symptoms that have no clear medical cause, such as persistent pain, tension headaches, dizziness, chest pains, digestive issues (like irritable bowel syndrome), and chronic fatigue. These are often manifestations of a dysregulated nervous system.
15. Cognitive Difficulties
Trauma can impact cognitive function, leading to what’s often described as “brain fog.” You might struggle with problems concentrating, experience memory issues (beyond dissociative gaps), and find it difficult to make even simple decisions. This can affect work, studies, and daily functioning.
16. Suicidal Thoughts
Callout Box: If you’re in crisis, call or text 988 right now. You are not alone.
The overwhelming pain, shame, hopelessness, and negative self-concept associated with C-PTSD can tragically lead to suicidal thoughts. This might manifest as actively planning to end your life, wishing you were dead, or feeling like a burden to others. It’s a severe symptom that requires immediate attention and support.
17. Inability to Experience Positive Emotions
A pervasive emotional numbness can make it difficult to experience joy, love, excitement, or other positive feelings. You might feel empty or flat, even during moments that should be happy. Research suggests that C-PTSD can dampen a person’s ability to regulate positive emotions, leaving a feeling of hollowness.
You Are Not Broken: Evidence-Based Treatment Can Reclaim Your Life
Recognizing what are the 17 symptoms of complex PTSD is a powerful first step, but the journey doesn’t end there. We understand that living with these symptoms can feel like an ongoing battle, but we want you to know: you are not broken, and healing is absolutely possible. Recovery is a process, not a destination, and it often requires professional support and evidence-based therapies.
At Thrive Mental Health, we specialize in providing trauma-informed care designed to help adults and young professionals steer the complexities of C-PTSD. Our approach integrates various therapeutic modalities proven effective for complex trauma, including:
- Trauma-Focused Cognitive Behavioral Therapy (TF-CBT): Helps you process traumatic memories and develop healthier coping mechanisms.
- Dialectical Behavior Therapy (DBT): Focuses on building skills in emotional regulation, distress tolerance, interpersonal effectiveness, and mindfulness, which are crucial for C-PTSD.
- Eye Movement Desensitization and Reprocessing (EMDR): A powerful therapy that helps process traumatic memories and reduce their emotional impact.
- Somatic Experiencing (SE): Addresses the physical manifestations of trauma, helping to release stored tension and regulate the nervous system.
- Internal Family Systems (IFS): A “parts work” approach that helps integrate fragmented parts of the self resulting from trauma.
Medication can also be a supportive element, especially for managing co-occurring conditions like depression, anxiety, or sleep problems that often accompany C-PTSD. However, it’s typically most effective when used as part of a comprehensive treatment plan that includes therapy.
In addition to professional treatment, self-help strategies and lifestyle changes play a vital role in supporting recovery:
- Grounding Techniques: Practices like deep breathing, focusing on your five senses, or progressive muscle relaxation can help you stay present and manage overwhelming emotions.
- Establishing Safety: Creating a physically and emotionally safe environment is paramount. This might involve setting boundaries, building a trusted support system, or seeking safe housing.
- Building a Support Network: Connecting with understanding friends, family, or C-PTSD support groups can combat feelings of isolation and foster a sense of belonging.
- Self-Compassion: Learning to treat yourself with kindness and understanding, recognizing that your symptoms are adaptive responses to extreme stress, not personal failings.
- Mindfulness and Body-Based Practices: Gentle yoga, tai chi, meditation, or spending time in nature can help regulate your nervous system and promote a sense of calm.
- Healthy Lifestyle: Prioritizing regular sleep, nutritious food, and consistent physical activity can significantly improve mood and resilience.
We offer trauma-focused virtual IOP programs that provide intensive, structured care from the comfort of your home, or in-person programs at our locations across Florida. Our programs combine clinical expertise, flexible scheduling, and measurable results—designed for people who need more than once-a-week therapy but less than inpatient care.
Frequently Asked Questions about Complex PTSD
How is C-PTSD diagnosed?
C-PTSD is diagnosed by a qualified mental health professional through a comprehensive clinical assessment. This involves a detailed evaluation of your trauma history, current symptoms, and how they impact your daily life. They will look for the core PTSD symptoms alongside the “disturbances in self-organization” (emotional dysregulation, negative self-perception, and relationship difficulties). Tools like the International Trauma Questionnaire (ITQ) may be used to align with ICD-11 criteria. It’s crucial to seek a trauma-informed professional who understands the nuances of complex trauma, as C-PTSD can sometimes overlap with other conditions.
Is C-PTSD a permanent disability?
While C-PTSD is a serious condition that can have profound and lasting effects, it is not considered a permanent disability in the sense that it cannot be treated. With effective, trauma-informed treatment, individuals can learn to manage their symptoms, process their trauma, build resilience, and lead fulfilling lives. Recovery is a journey that looks different for everyone, but significant improvement and a higher quality of life are absolutely achievable.
What should I NOT say to someone with C-PTSD?
When interacting with someone struggling with C-PTSD, certain phrases can be incredibly invalidating and harmful. Avoid saying things like “just get over it,” “it wasn’t that bad,” “everyone goes through tough times,” or offering unsolicited advice like “you just need to move on.” These statements minimize their pain and can reinforce feelings of shame and isolation. Instead, practice active listening, offer validation (“That sounds incredibly difficult,” “I hear you,” “I believe you”), express your support, and ask how you can best help them.
Your First Step to Healing Starts Now

Recognizing what are the 17 symptoms of complex PTSD is a critical first step on your healing journey. It takes immense courage to confront the lasting impact of prolonged trauma, and we want you to know that you don’t have to manage this alone. Specialized, trauma-informed care can provide the tools and support you need to process your experiences, regulate your emotions, rebuild your self-concept, and foster healthier relationships.
At Thrive Mental Health, we are dedicated to helping adults and young professionals find lasting recovery from C-PTSD. Our virtual and in-person Intensive Outpatient (IOP) and Partial Hospitalization (PHP) programs are designed with clinical expertise and flexible scheduling to meet you where you are. We serve individuals across Florida, and we work with major insurance providers like Cigna, Aetna, and Florida Blue to make evidence-based treatment accessible.
Ready for support? Thrive offers virtual and hybrid IOP/PHP programs with evening options. Verify your insurance in 2 minutes (no obligation) → Start benefits check or call 561-203-6085. If you’re in crisis, call/text 988.