Mentalization-Based Therapy for BPD: When Mindfulness Meets Mentalizing

Mentalization Based Therapy for BPD: 1 Powerful Hope
Mentalization-Based Therapy for BPD [2025]: 86% No Longer Meet Criteria—Cut Self-Harm and Hospital Stays
If you’re in crisis or thinking about self-harm, call or text 988 (24/7).
[If you’re in crisis, call/text 988 right now. You are not alone.]
Summary: Mentalization based therapy for bpd helps you understand thoughts, feelings, and intentions—reducing self-harm, hospitalizations, and relationship chaos with lasting results.
Mentalization based therapy for bpd offers hope for those caught in the exhausting cycle of intense emotions, unstable relationships, and identity confusion that defines borderline personality disorder. This evidence-based approach focuses on one crucial skill: understanding the mental states behind your own and others’ behaviors.
Quick Answer for Mentalization-Based Therapy for BPD:
- What it is: A therapy that improves your ability to understand thoughts, feelings, and intentions
- How it works: Through weekly individual and group sessions over 12-18 months
- Success rate: 86% of patients no longer met BPD criteria after 8 years
- Key benefit: Reduces self-harm, hospitalizations, and improves relationships
- Best for: People with BPD who struggle with emotional regulation and relationships
If you have BPD, you know the pain of feeling misunderstood. You might idealize someone one moment, then fear abandonment the next. With overwhelming emotions and unstable relationships, you may wonder if things can ever get better.
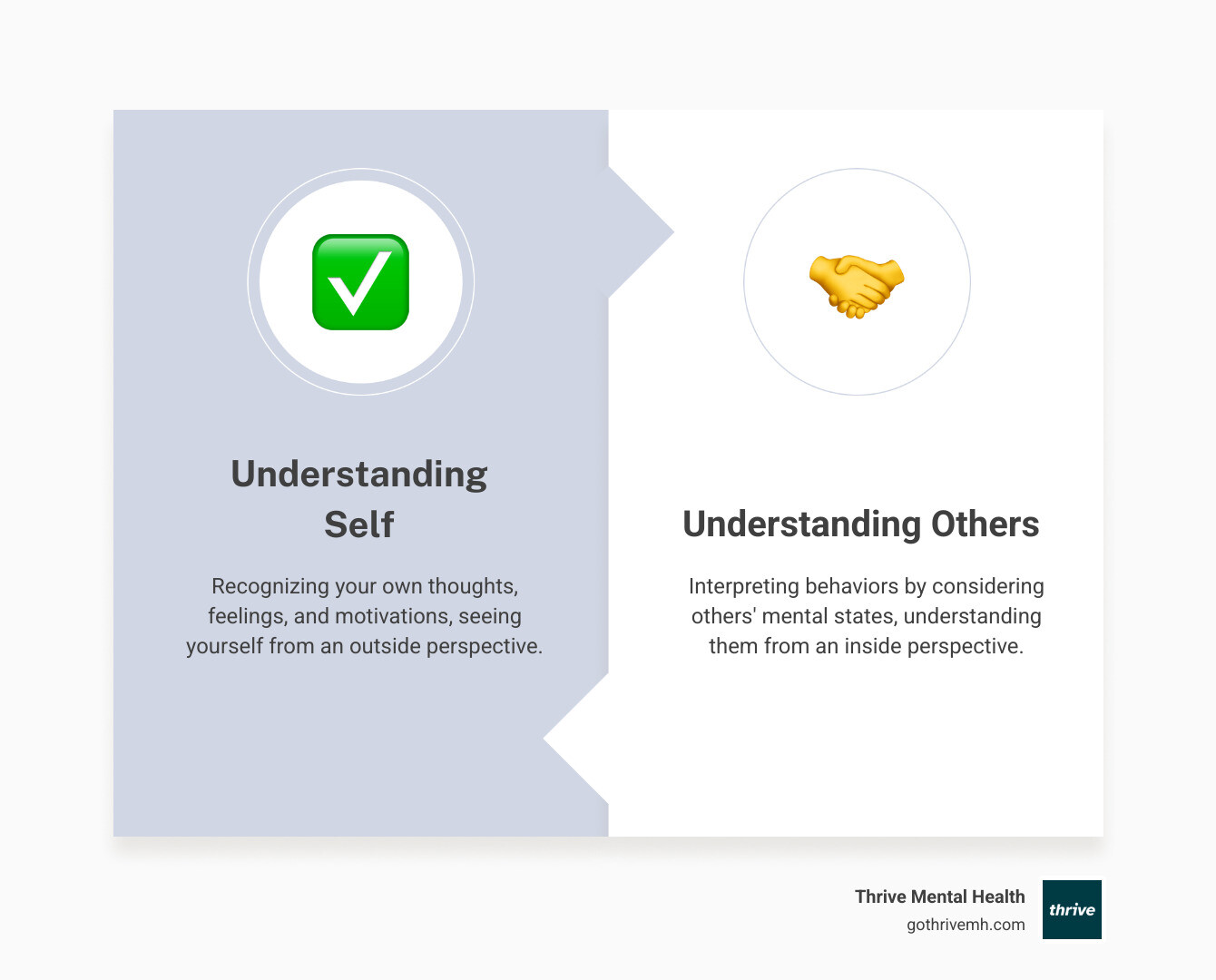
The answer is yes. MBT helps you develop what researchers call “mentalization” – the ability to see yourself from the outside and understand others from the inside. It’s like having a pause button for your emotions and a translator for your relationships.
I’m Anna Green, LMHC, LPC, Chief Clinical Officer at Thrive Mental Health, with specialized training in Mentalization-Based Therapy alongside my work in complex trauma and personality disorders. Through years of clinical practice, I’ve seen how mentalization based therapy for bpd transforms lives by addressing the core challenges of emotional dysregulation and relationship instability.
Quick mentalization based therapy for bpd definitions:
What Is BPD and Why Does Mentalizing Matter?
If you or someone you know is in crisis or struggling with thoughts of self-harm, please call or text the 988 Suicide & Crisis Lifeline. Help is available 24/7, and you are not alone.
Borderline Personality Disorder affects 0.2-1.8% of people worldwide, rising to 11% of adolescent outpatients and 49% of inpatients. If this is your struggle, you are not alone.
BPD makes daily life overwhelming. Emotional instability causes rapid mood shifts from intense joy to despair. Unstable relationships swing between idealization and devaluation. Impulsivity can lead to regrettable decisions like reckless spending or risky behaviors.
Identity disturbance leaves you unsure of who you are, often with chronic feelings of emptiness. Intense anger can be surprising, and a deep fear of abandonment can make every relationship feel precarious.
Perhaps most concerning, research shows that 69-80% of people with BPD engage in self-harm or suicidal behavior, with suicide rates reaching up to 10%. These aren’t just statistics – they represent real people struggling with real pain.
Here’s where mentalization based therapy for bpd comes in as a game-changer. At the heart of BPD lies a challenge with something called mentalization – your ability to understand the thoughts, feelings, and intentions behind both your own behavior and others’ actions.
Think of mentalization as your emotional GPS. When it’s working well, you can steer relationships and understand why you feel the way you do. But when it breaks down – especially under stress – you’re left trying to read a map in the dark.
Peter Fonagy and Anthony Bateman, the pioneers who developed MBT, finded that BPD is essentially what happens when our mentalization system gets overwhelmed. This usually starts in childhood when attachment relationships with caregivers are disrupted through trauma, neglect, or inconsistent care. Without those secure early bonds, our ability to “keep mind in mind” never fully develops.
The Breakdown of Mentalizing in BPD
When your mentalizing capacity shuts down under stress, the world becomes a much scarier and more confusing place. That fear of abandonment kicks in because you can’t accurately read what’s happening in relationships. Your friend seems quiet, and instead of thinking “maybe they’re tired,” your brain jumps to “they hate me and they’re leaving.”
Black-and-white thinking takes over because nuanced understanding requires mentalization. People become all good or all bad, with no middle ground. Yesterday’s perfect partner becomes today’s worst enemy over a minor disagreement.
Misinterpreting others becomes the norm. A neutral facial expression looks angry. A delayed text response means rejection. Your boss’s feedback feels like a personal attack. Without mentalization, you’re constantly misreading social cues and responding to threats that aren’t really there.
The intense emotional reactions that define BPD make perfect sense when you understand that your emotional pause button is broken. Small triggers create massive responses because you can’t step back and mentalize what’s really happening.
This creates a vicious cycle where you feel misunderstood by everyone around you. How can you explain your feelings to others when you don’t understand them yourself? How can others understand you when you’re misreading their intentions?
Under stress, people with BPD often swing between extremes. Sometimes you might hyperactivate – becoming overly trusting, idealizing someone new, or crossing boundaries in your desperation for connection. Other times you might deactivate – shutting down emotionally, appearing calm while drowning inside, or isolating yourself completely. Many people experience both patterns, creating the relationship chaos that makes BPD so exhausting.
The good news? Mentalization based therapy for bpd specifically targets these core issues. Instead of just managing symptoms, MBT helps rebuild your capacity to understand minds – starting with your own.
Your Complete Guide to Mentalization-Based Therapy for BPD
If you’re considering mentalization based therapy for bpd, you’re taking a brave step toward understanding yourself in a whole new way. Think of MBT as learning a new language – the language of minds. Instead of just reacting to what people do, you’ll start understanding why they do it. And more importantly, you’ll understand your own “why” too.
This isn’t about changing who you are. It’s about helping you become the expert on your own mind while building bridges to others’ hearts and thoughts.
The Core Principles: What Makes MBT Work?
Mentalization based therapy for bpd emerged in the 1990s when Anthony Bateman and Peter Fonagy noticed something important: traditional therapy approaches weren’t quite hitting the mark for people with BPD. They realized that the real breakthrough came from focusing on one core skill – mentalization.
From psychoanalytic roots and attachment theory, MBT recognizes that your early relationships shaped how you understand minds (including your own). If those early experiences were chaotic or traumatic, your “mind-reading” abilities might go haywire when emotions run high.
The primary goal isn’t just symptom relief – though that often follows. It’s about strengthening your capacity to mentalize, which then naturally improves everything else: your relationships, emotional stability, and sense of self.
What makes MBT different is the therapist’s “not knowing” stance. Your therapist won’t pretend to be a mind reader or tell you what you’re “really” feeling. Instead, they’ll ask genuine questions like “What was going through your mind when that happened?” or “What do you think they might have been feeling?”
This curiosity and collaboration creates a safe space where you can explore without judgment. You and your therapist become partners in detective work, investigating the mental states behind behaviors. The focus stays on the present moment – what’s happening right now in your relationships, in the therapy room, and in your daily interactions.
What to Expect in an MBT Session
Walking into your first MBT session, you might wonder what makes it different from other therapies. The atmosphere feels collaborative rather than clinical – like having a conversation with someone who’s genuinely curious about how your mind works.
One powerful technique you’ll experience is “stop and rewind.” When emotions spike or conflicts emerge, your therapist might pause the conversation and say, “Let’s rewind for a moment. What was happening in your mind right before things got intense?” This isn’t about criticism – it’s about understanding.
You’ll spend time exploring alternative views of situations. If you’re convinced someone was being hostile, your therapist might gently ask, “What else could have been going on for them?” This expands your perspective without invalidating your experience.
Clarifying misunderstandings becomes a regular practice. Those moments when you’re sure someone meant to hurt you? You’ll learn to pause and consider other possibilities. Maybe they were distracted, tired, or dealing with their own struggles.
The therapeutic relationship itself becomes your practice ground. How you perceive your therapist, how you react to their comments, how you handle scheduling changes – all of this offers rich material for understanding your patterns with others.
Most MBT programs combine individual therapy sessions with group therapy. Individual sessions give you private space to explore personal triggers and receive custom guidance. Group sessions let you practice with multiple people, learning from others’ experiences while getting feedback on your own patterns.
A typical MBT journey lasts 12-18 months – long enough to build real, lasting changes in how you understand minds. This isn’t a quick fix, but rather a deep reconstruction of fundamental skills.
More info about our virtual IOP/PHP programs
Finding a Qualified MBT Program
Finding the right MBT program can feel overwhelming, especially when you’re already struggling. The key is looking for certified therapists who’ve completed specialized MBT training – not just general therapy training.
At Thrive Mental Health, we integrate MBT into our Intensive Outpatient Programs (IOP) and Partial Hospitalization Programs (PHP). These structured programs provide the consistent support needed for real change while allowing you to maintain your daily responsibilities.
Insurance coverage is often a major concern, and we work with major providers including Cigna, Optum, and Florida Blue. Our goal is removing financial barriers to quality care.
We understand that location matters too. Our programs serve communities across Florida, with flexible care options including virtual sessions and evening programs. Whether you’re in Miami, Orlando, or anywhere in between, you can access expert-led treatment that fits your schedule.
The beauty of our virtual options means you can receive mentalization based therapy for bpd from the comfort of your own space, which can actually improve the therapeutic process by reducing anxiety about new environments.
Verify your insurance in 2 minutes
Does MBT Actually Work? [The Research]
When you’re struggling with BPD, hope can feel hard to come by. You might wonder if anything will truly help, or if the research behind mentalization based therapy for bpd is just another set of empty promises. The good news? The evidence is not only solid – it’s remarkable.
MBT stands as a rigorously tested, evidence-based treatment for BPD. This means scientists have put it through the gold standard of research: randomized controlled trials where some people receive MBT while others receive different treatments or standard care. The results consistently show that MBT works – and works well.
The journey began with groundbreaking research in 1999. Patients receiving MBT in a partial hospitalization program showed significant improvements compared to those getting standard treatment. We’re talking about real changes: reduced suicidal acts, fewer self-harm episodes, less time in the hospital, and better relationships with family and friends. These weren’t just small improvements – they were life-changing differences.
But perhaps what’s most encouraging is what happened when researchers checked back years later. An 8-year follow-up study revealed something extraordinary: only 14% of patients treated with MBT still met BPD criteria, compared to 87% of those who received standard treatment. Think about that – after eight years, most people who received MBT had moved beyond their BPD diagnosis entirely.
8-year followup study on MBT effectiveness
The research shows MBT doesn’t just mask symptoms temporarily. It creates lasting change by improving your actual ability to mentalize – to understand your own thoughts and feelings and those of others. Studies measured this directly and found significant improvements in how people process emotions and steer social situations.
What does this mean for you? It means that the emotional chaos, relationship instability, and identity confusion that feel so overwhelming right now can genuinely improve. The research shows that MBT helps people build healthier relationships, develop better emotional regulation, and create a more stable sense of self that lasts long after therapy ends.
These aren’t just statistics – they represent real people who once felt hopeless and now live fulfilling lives. The evidence gives us confidence that mentalization based therapy for bpd offers a clear path from where you are now to where you want to be.
How MBT Compares to Other BPD Therapies
When you’re facing a BPD diagnosis, the number of treatment options can feel overwhelming. You might hear about Dialectical Behavior Therapy (DBT), Schema Therapy, or Transference-Focused Psychotherapy, and wonder which one is “right” for you. The truth is, there’s no one-size-fits-all answer – and that’s actually good news.
Understanding treatment options is the first step toward healing. All effective BPD therapies share some important qualities: they’re well-structured, focus on specific issues, have solid theoretical foundations, and encourage a strong therapeutic relationship. But each approach has its own personality, if you will.
At Thrive Mental Health, we believe in finding the right fit for your unique situation. Sometimes that means mentalization based therapy for bpd, sometimes it means integrating elements from different approaches. Our goal is creating individualized care plans that actually work for your life, your schedule, and your specific challenges.
Learn about other evidence-based therapies we use
MBT vs. DBT: What’s the Difference?
Think of MBT and DBT as two different paths up the same mountain. Both want to help you live a fuller, more stable life – they just take different routes to get there. While both can be incredibly powerful, they have different focuses and techniques.
Dialectical Behavior Therapy (DBT)
- Focus: Behavioral and skills-based. It teaches concrete techniques for managing intense emotions, tolerating distress, and communicating effectively.
- Goal: Building what founder Marsha Linehan calls “a life worth living” through practical skill-building.
- Techniques: Diary cards, distress tolerance skills (like STOP and PLEASE), and chain analysis to break down problem behaviors.
- Therapist Stance: Validating yet challenging, balancing acceptance with the push for change.
Mentalization-Based Therapy (MBT)
- Focus: Relational and process-oriented. It helps you understand the why behind your reactions by exploring the thoughts and feelings driving them.
- Goal: Understanding minds in relationships—both your own mind and others’.
- Techniques: “Stop and rewind” moments, exploring alternative perspectives, and clarifying misunderstandings in the moment.
- Therapist Stance: Curious and collaborative, asking “what” questions to help you explore your internal world without judgment.
At Thrive, we often integrate elements from both approaches into your treatment plan to provide the most effective, individualized care.
Is mentalization based therapy for bpd the only use?
While mentalization based therapy for bpd was originally developed specifically for borderline personality disorder, its core principle – improving your ability to understand mental states – turns out to be incredibly versatile. Think about it: most mental health struggles involve some difficulty understanding our own thoughts and feelings, or misreading others’ intentions.
Other applications where MBT shows promise include antisocial personality disorder, where individuals often struggle to mentalize others’ suffering. For narcissistic personality disorder, MBT helps people move from a “me-focused” to a “we-focused” perspective, building genuine empathy.
The approach has also been adapted for eating disorders, particularly anorexia, where people often lose touch with their body’s signals and emotional needs. In depression, MBT helps break the cycle of rumination by helping you understand what’s really driving those dark thoughts.
Adolescent self-harm is another area where MBT shines, helping young people understand the mental states that lead to hurting themselves. Research suggests it may be effective for other personality disorders too, including Avoidant Personality Disorder.
Challenges and limitations do exist. MBT requires significant commitment – typically 12-18 months – and finding a qualified therapist can be challenging, though training is becoming more accessible. It also requires emotional energy and willingness to explore difficult feelings, which isn’t always easy when you’re already struggling.
Future research directions include refining MBT for specific combinations of conditions, exploring its effectiveness across different cultural backgrounds, and continuing to understand exactly how it creates lasting change. The field is growing, and we’re excited about the potential for helping even more people find their way to emotional stability and healthier relationships.
FAQs: Mentalization-Based Therapy for BPD
-
What is Mentalization-Based Therapy (MBT) for BPD?
MBT helps you understand your own and others’ thoughts, feelings, and intentions so you react less impulsively and relate more clearly. It targets the core BPD problem: breakdowns in mentalizing under stress. -
How effective is MBT for BPD?
Strong evidence: in an 8-year follow-up, 86% of MBT patients no longer met BPD criteria, with fewer self-harm episodes and hospitalizations. -
How long does MBT take, and what happens in sessions?
Typically 12–18 months. You’ll attend weekly individual and group sessions, use “stop and rewind” to examine trigger moments, and practice seeing multiple perspectives. -
MBT vs. DBT: which is right for me?
DBT is skills-focused (distress tolerance, emotion regulation). MBT is relationship- and process-focused (understanding the “why” behind reactions). Many people benefit from a blend—ask your clinician which fits your goals and history. -
Does insurance cover MBT in Florida (Cigna, Optum, Florida Blue)?
Often yes. Thrive works with major plans including Cigna, Optum, and Florida Blue for care in Florida. Coverage varies—check your benefits in minutes: https://gothrivemh.com/verify-insurance/ -
Can I do MBT online?
Yes. MBT works well via secure virtual sessions, including IOP/PHP formats for added structure and support.
Suggested JSON-LD FAQ schema (add to page as a script tag):
{
“@context”: “https://schema.org”,
“@type”: “FAQPage”,
“mainEntity”: [
{
“@type”: “Question”,
“name”: “What is Mentalization-Based Therapy (MBT) for BPD?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “MBT helps you understand your own and others’ thoughts, feelings, and intentions so you react less impulsively and relate more clearly. It targets BPD’s core issue: mentalizing breakdowns under stress.”
}
},
{
“@type”: “Question”,
“name”: “How effective is MBT for BPD?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “In an 8-year follow-up, 86% of MBT patients no longer met BPD criteria, with fewer self-harm episodes and hospitalizations.”
}
},
{
“@type”: “Question”,
“name”: “How long does MBT take, and what happens in sessions?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Most courses last 12–18 months with weekly individual and group sessions using ‘stop and rewind,’ perspective-taking, and in-the-moment clarification.”
}
},
{
“@type”: “Question”,
“name”: “MBT vs. DBT: which is right for me?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “DBT is skills-based; MBT focuses on understanding the ‘why’ behind reactions. Many benefit from a blended approach based on goals and history.”
}
},
{
“@type”: “Question”,
“name”: “Does insurance cover MBT in Florida?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Often yes. Thrive works with Cigna, Optum, and Florida Blue for care in Florida. Verify coverage here: https://gothrivemh.com/verify-insurance/.”
}
}
]
}
Ready for Support?
Thrive offers virtual and hybrid IOP/PHP with evening options so treatment fits your life in Florida. We work with major insurance plans, including Cigna, Optum, and Florida Blue.
Ready for support? Thrive offers virtual and hybrid IOP/PHP with evening options. Verify your insurance in 2 minutes (no obligation) → Start benefits check or call 561-203-6085.
- Explore programs: IOP → https://gothrivemh.com/virtual-iop/ | PHP → https://gothrivemh.com/partial-hospitalization-program-php/
- Prefer telehealth? See Virtual Therapy → https://gothrivemh.com/virtual-therapy/
If you’re in crisis, call or text 988. You are not alone.

