OCD Medications Explained – What Works and Why

Medication for OCD: 1st-Line Relief Guide
If You’re in Crisis, Help Is Here
If you’re in crisis, call or text 988 right now. You are not alone.
Why Finding the Right Medication for OCD Changes Everything
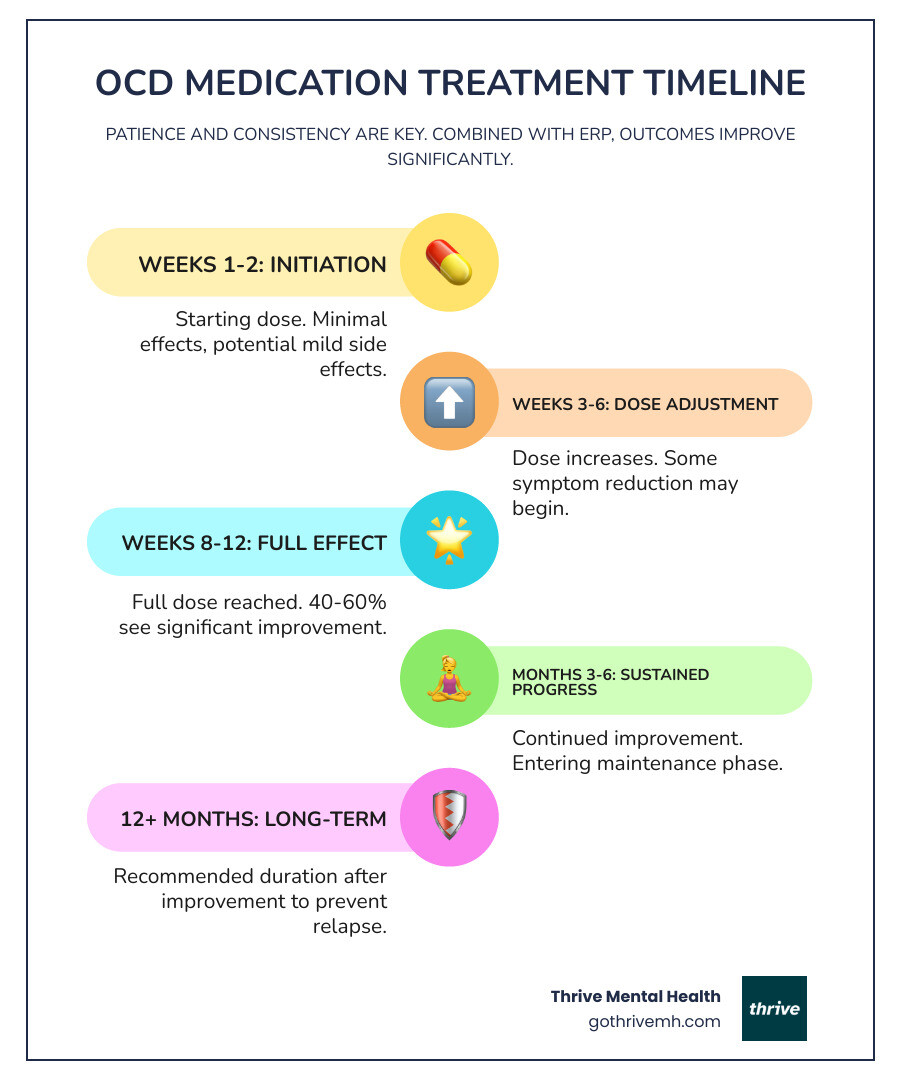
If you’re living with OCD, you know the exhaustion of intrusive thoughts and compulsions. Medication for OCD can significantly reduce these symptoms for most people, but it’s a process that requires patience and the right information.
The first-line treatment is a class of medications called SSRIs (like Prozac, Zoloft, Luvox, and Paxil). They take 8 to 12 weeks to show their full effects, and you’ll need to be at a higher dose for at least six of those weeks.
Research shows that 40 to 60% of people experience a 40 to 50% reduction in symptom severity. This isn’t a cure, but it can be life-changing, creating the space to live your life instead of being controlled by OCD.
Unlike depression treatment, OCD medication requires higher doses and longer trials. It works best when paired with therapy like Exposure and Response Prevention (ERP). Think of medication as turning down the volume on obsessions, while therapy teaches you new ways to respond.
If your first medication doesn’t work, don’t worry—that’s common. Options include switching SSRIs, adding a booster drug, or trying Clomipramine. Most people need to stay on medication for at least 12 months after their symptoms improve to prevent relapse.
This guide, written by Anna Green, LMHC, LPC, and founder of Thrive Mental Health, will walk you through your options to make this process clearer and less overwhelming. We offer virtual and hybrid IOP/PHP programs that combine medication support with evidence-based therapy.
Quick medication for ocd terms:
First-Line Treatment: Why SSRIs Are the Starting Point for OCD
When starting medication for OCD, your doctor will almost always begin with SSRIs (Selective Serotonin Reuptake Inhibitors). They are the gold standard due to decades of research showing their effectiveness and better safety profile compared to older drugs.
How Do SSRIs Work to Alleviate OCD Symptoms?
SSRIs work by increasing the amount of available serotonin, a chemical messenger in the brain that helps regulate mood, anxiety, and intrusive thoughts. By blocking serotonin’s reabsorption, SSRIs improve communication between brain cells, which over time reduces obsessive thoughts and compulsive urges.
What Are the Primary Types of Medications Used to Treat OCD?
The primary medications for OCD are Serotonin Reuptake Inhibitors (SRIs). This includes SSRIs and one older tricyclic antidepressant.
- FDA-approved SSRIs for OCD: Fluoxetine (Prozac), Sertraline (Zoloft), Fluvoxamine (Luvox), and Paroxetine (Paxil). Citalopram (Celexa) and Escitalopram (Lexapro) are also commonly used off-label.
- Second-line option: Clomipramine (Anafranil), a powerful but older medication with more side effects.
Effectiveness Rate of SSRIs for OCD
Research shows that about 40% to 60% of people with OCD see a significant 40–50% reduction in symptom severity with an SSRI. However, fewer than 20% achieve full remission with medication alone. That’s why combining medication with Exposure and Response Prevention (ERP) therapy offers the best chance for lasting improvement. You can learn more from the NHS guidance on SSRI antidepressants.

How OCD Medication Differs from Depression Treatment
Treating OCD with medication is different from treating depression, even when using the same drugs. The doses are higher, the timeline is longer, and the experience can feel entirely new.
| Condition | Typical Dose | Time to See Effects | Recommended Trial Length |
|---|---|---|---|
| OCD | Higher (often 2-3x higher than for depression) | 8–12 weeks | 12+ weeks |
| Depression | Lower | 2–4 weeks | 6–8 weeks |
Dosing and Duration for OCD Medication
OCD typically requires doses two to three times higher than those for depression. Treatment starts with a low dose that is gradually increased over several weeks (slow titration) to help your body adjust and minimize side effects. An adequate trial of medication for OCD takes 8 to 12 weeks, with at least six weeks at a high dose. This patience is necessary for the medication to work. Once symptoms improve, treatment should continue for at least 12 months to prevent relapse. For some, long-term medication is the most effective strategy for stability.
What to Expect During Your OCD Medication Trial
Improvement takes time. We use tools like the Yale-Brown Obsessive-Compulsive Scale (Y-BOCS) to objectively track symptoms. A partial response (some improvement) is a good sign, and we might increase the dose or add another medication. No response after an adequate trial means we’ll switch to a different option. About 20% of people don’t respond to their first medication; this is a normal part of finding the right fit for your brain.
What If First-Line Medication for OCD Isn’t Enough?
If an SSRI doesn’t provide enough relief after a full trial, you have several other options. This is known as treatment-resistant OCD, and it’s important not to lose hope. Your provider may suggest switching to a different SSRI, trying Clomipramine, adding a second medication (augmentation), or intensifying your therapy.
Second-Line Option: Clomipramine (Anafranil)
Clomipramine is a Tricyclic Antidepressant (TCA) and was the first medication proven effective for OCD. While highly effective, it’s now a second-line medication for OCD because it has more side effects than SSRIs, including dry mouth, constipation, weight gain, and sedation. It can also cause more serious cardiac issues, so regular monitoring with electrocardiograms (EKGs) is essential. For many who don’t respond to SSRIs, Clomipramine provides the breakthrough they need.
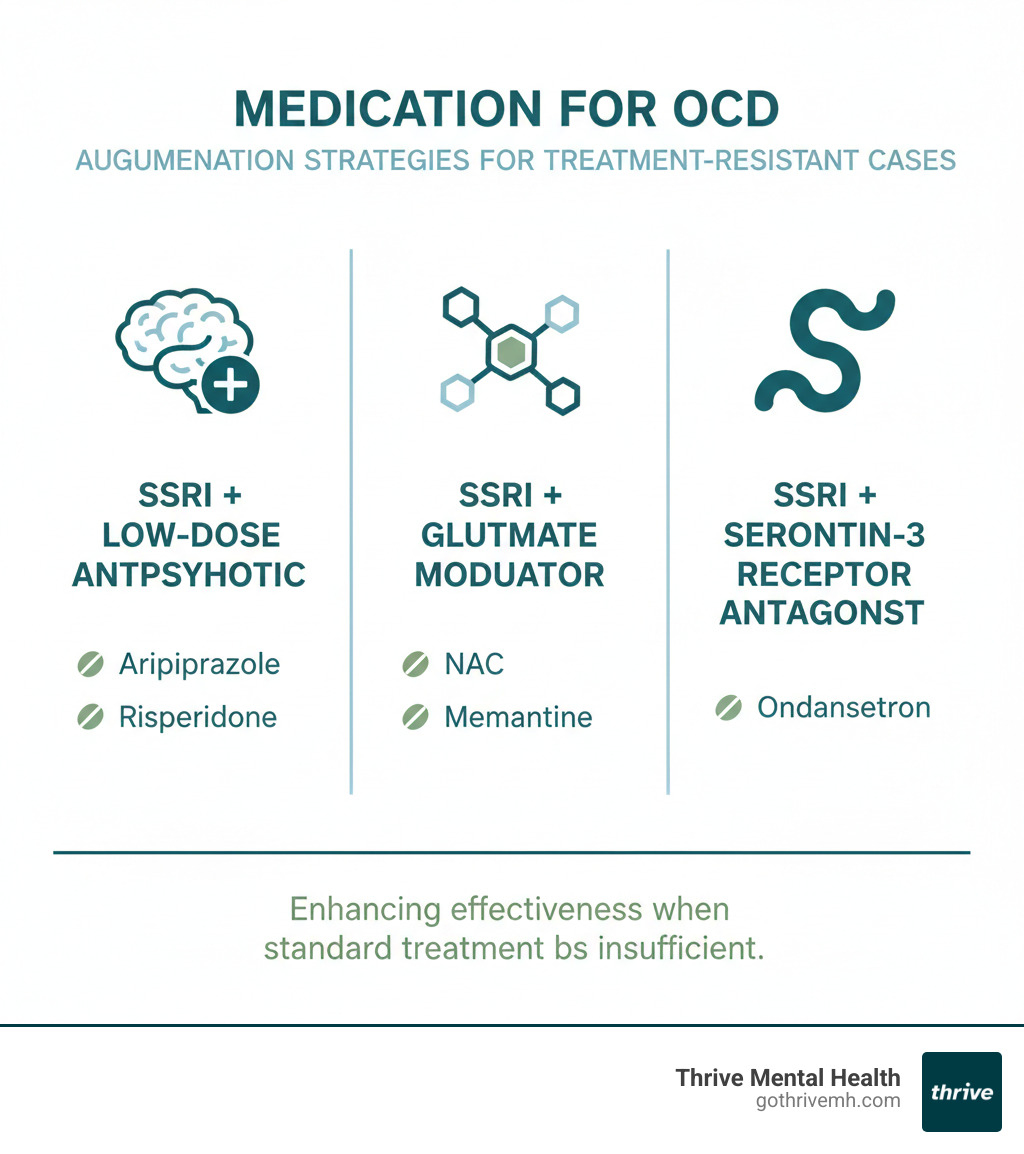
Augmentation: Boosting Your Medication’s Effectiveness
If an SSRI is partially working, augmentation can improve its effects. This involves adding a second medication to your regimen.
- Atypical Antipsychotics: Adding a low dose of a medication like risperidone (Risperdal) or aripiprazole (Abilify) helps about one-third of people who don’t fully respond to an SSRI alone.
- Glutamate Modulators: Newer options like N-Acetylcysteine (NAC) or memantine (Namenda) show promise with fewer side effects.
- Other Options: There is some evidence for adding serotonin-3 receptor antagonists like ondansetron (Zofran).
Crucially, augmentation works best when combined with intensive therapy. For many, intensifying Exposure and Response Prevention (ERP) therapy is more effective than adding another drug. At Thrive Mental Health, our virtual and hybrid IOP/PHP programs integrate these strategies for the best outcomes.
Managing Your OCD Treatment and Finding Support
Finding the right medication for OCD is just the start; managing your treatment effectively over time is key to success. Open communication with your healthcare provider is your most important tool. Track your symptoms and side effects, and be honest about what you’re experiencing so your plan can be adjusted.
Common Side Effects and How to Manage Them
Most SSRI side effects are temporary and fade within a few weeks. Common ones include nausea, restlessness or drowsiness, headaches, increased sweating, and sexual dysfunction. If side effects are persistent or intolerable, we have several strategies:
- Adjust the dose or slow the rate of increase.
- Change the timing of your medication (e.g., take at night for drowsiness).
- Switch to a different SSRI, as each has a unique side-effect profile.
Always discuss your full medical history, all other medications and supplements you take, and any concerns you have with your doctor. This includes alcohol or recreational drug use, as interactions can be dangerous.
Stopping or Switching Your OCD Medication
Never stop taking your medication abruptly, even if you feel better. Doing so can cause discontinuation syndrome, with unpleasant symptoms like dizziness, nausea, and “brain zaps.” More importantly, it creates a high risk of relapse, as OCD is a chronic condition. The protective effects of SSRIs don’t last once you stop taking them.
The only safe way to stop is through a gradual taper supervised by your provider. Tapering is most successful when you are actively engaged in therapy like Exposure and Response Prevention (ERP), which provides the skills to manage symptoms as medication is reduced. Our programs at Thrive Mental Health offer this integrated support.
When Should Medication Be Considered for OCD?
Deciding on the right treatment approach—therapy, medication for OCD, or both—depends on your symptom severity, personal preference, and available resources.
- For mild to moderate OCD: Psychotherapy, specifically Exposure and Response Prevention (ERP), is often the recommended first-line treatment and can be highly effective on its own.
- For moderate to severe OCD: The combination of an SSRI and ERP consistently produces the best results. Medication helps lower the intensity of obsessions, making it easier to engage in the challenging work of ERP.
- For severe or debilitating OCD: Starting medication first can be necessary to reduce distress to a level where therapy becomes possible. This also applies if you have significant co-occurring depression or anxiety.
- When ERP is unavailable: If you cannot find a trained ERP therapist, medication may be the most accessible primary treatment option. Thrive Mental Health’s virtual IOP and PHP programs can bridge this gap by providing expert ERP therapy remotely in Florida.
Your preference is a key part of the decision. A successful treatment plan honors your comfort level and values.
Medication for OCD in Children and Adolescents
OCD often begins in childhood or adolescence, and early treatment is vital. While psychotherapy is the first choice, medication for OCD can be an important tool for younger individuals.
Several SSRIs are FDA-approved for pediatric OCD:
- Sertraline (Zoloft): Age 6 and older
- Fluoxetine (Prozac): Age 7 and older
- Fluvoxamine (Luvox): Age 8 and older
- Clomipramine (Anafranil): Age 10 and older
For children and teens, Exposure and Response Prevention (ERP) therapy is the first-line treatment. Medication is typically considered only if symptoms are severe or if therapy alone is not enough.
When medication is used, close monitoring by a specialist is essential to track effectiveness, side effects, and growth. All antidepressants carry an FDA black box warning for a potential increase in suicidal thoughts in young people, especially during the initial weeks of treatment. This risk requires vigilance and open communication between the family and the provider. Our IOP and PHP programs at Thrive Mental Health provide this level of intensive, coordinated support for adolescents and young adults.
Newer Treatment Options for Treatment-Resistant OCD
If you’ve tried multiple medications and therapy without finding relief, it can be incredibly discouraging. However, treatment-resistant OCD does not mean treatment-impossible. It often means a more intensive approach is needed.
For many, the answer lies in a higher level of care. Intensive Outpatient Programs (IOP) and Partial Hospitalization Programs (PHP) provide a structured, immersive experience that can create breakthroughs when weekly therapy stalls.
At Thrive Mental Health, our IOP and PHP programs offer multiple hours of therapy per week, including expert-led Exposure and Response Prevention (ERP), group sessions, and coordinated medication management. This comprehensive approach addresses symptoms from multiple angles while allowing you to live at home and maintain your daily responsibilities.
While advanced medical interventions like Transcranial Magnetic Stimulation (TMS) and Deep Brain Stimulation (DBS) exist for the most severe cases, they are typically considered only after intensive therapy programs have been tried.
Don’t give up. A different approach may be what you need. Verify your insurance coverage in two minutes or call us at 561-203-6085 to discuss if a higher level of care is right for you.
Accessing OCD Care in Florida
Finding the right care for OCD shouldn’t feel like another obstacle to overcome. At Thrive Mental Health, we’ve built our programs around one simple belief: expert-led, evidence-based medication for OCD management and therapy should be accessible, flexible, and designed to fit into your life—not the other way around.
We offer virtual and hybrid intensive outpatient (IOP) and partial hospitalization (PHP) programs specifically designed for adults and young professionals who are ready to take control of their OCD. Our programs combine medication management with evidence-based therapies like Exposure and Response Prevention (ERP), all delivered by experienced clinicians who understand the unique challenges of OCD.
We know life doesn’t stop for treatment. That’s why we offer evening program options, so you can continue working, attending school, or managing your responsibilities while getting the intensive support you need. Whether you’re in Miami, Orlando, Tampa, Jacksonville, or anywhere else in Florida, you can access our care from the comfort and privacy of your own space.
Insurance shouldn’t be a barrier either. We accept a wide range of major insurance plans, including Cigna, Optum, and Florida Blue, to make treatment more affordable and accessible. Not sure if you’re covered? You can verify your insurance in 2 minutes—no obligation, no pressure, just clear answers about your options.
If you’re ready to explore how our IOP and PHP programs can support your journey with medication for OCD and therapy, we’re here to help. Learn more about our programs or reach out to our team. You don’t have to steer this alone.
Frequently Asked Questions About Medication for OCD
How long do I need to take medication for OCD?
Most guidelines recommend staying on medication for OCD for at least 12 months after your symptoms have significantly improved. Because OCD is a chronic condition with a high relapse rate, many people benefit from long-term or even lifelong treatment to maintain stability, especially if they have had multiple episodes.
Can I treat OCD without medication?
Yes. For mild to moderate OCD, Exposure and Response Prevention (ERP) therapy is a highly effective standalone treatment. However, for moderate to severe OCD, research consistently shows that combining medication with ERP yields the best and most durable results.
Which SSRI is best for OCD?
There is no single “best” SSRI for OCD, as all are considered equally effective. The right choice depends on individual factors like your specific symptoms, your health history, potential side effects, and your provider’s clinical judgment. Finding the best fit for you may take some trial and error.
Are there OCD medications for children?
Yes, several medications are FDA-approved for pediatric OCD: sertraline (Zoloft) for age 6+, fluoxetine (Prozac) for age 7+, fluvoxamine (Luvox) for age 8+, and clomipramine (Anafranil) for age 10+. Treatment for children requires close monitoring by a specialist and is usually combined with ERP therapy.
What if medication and therapy aren’t enough?
If you’re still struggling despite trying standard treatments, you are not out of options. The next step is often a higher level of care, such as an intensive outpatient (IOP) or partial hospitalization (PHP) program. These programs provide more structure and support to help you break through treatment resistance. Learn about Thrive’s virtual IOP/PHP programs to see if this is the right fit for you.
Summary: Medication for OCD—What You Need to Know
Navigating medication for OCD can be complex, but understanding the key principles makes it manageable. Here are the most important takeaways:
- SSRIs are the first-line treatment. They are effective for 40-60% of people but require higher doses and longer trials (8-12 weeks) than when used for depression.
- You have options if SSRIs aren’t enough. These include switching to another SSRI, trying the more powerful medication Clomipramine, or adding a booster drug (augmentation). Finding the right fit is a process.
- Side effects are manageable. Most are temporary. Working with your provider, you can adjust doses, timing, or switch medications to minimize them. Never stop medication abruptly due to the high risk of relapse and withdrawal symptoms.
- Medication works best with therapy. Combining medication with Exposure and Response Prevention (ERP) produces the most significant and lasting improvement.
- Treatment is a long-term commitment. Plan on at least 12 months of medication after symptoms improve to prevent relapse.
At Thrive Mental Health, we integrate medication management with intensive ERP in our virtual and hybrid IOP/PHP programs in Florida. We accept major insurance plans including Cigna, Optum, and Florida Blue to make comprehensive care accessible.
Ready for Support?
If you’re reading this and feeling overwhelmed by the complexity of medication for OCD, or if you’re wondering whether it’s time to seek more intensive help, please know that you don’t have to figure this out alone.
At Thrive Mental Health, we understand that OCD doesn’t follow a 9-to-5 schedule, which is why we’ve designed our programs with flexibility in mind. Our virtual and hybrid intensive outpatient (IOP) and partial hospitalization (PHP) programs include evening options specifically for adults and young professionals who need comprehensive care without putting their lives on hold.
Maybe you’ve tried medication and therapy but haven’t found the relief you’re looking for. Or perhaps you’re just starting to explore your options and need expert guidance. Either way, we’re here to support you through every step of your journey toward managing OCD.
Getting started is straightforward. You can verify your insurance coverage in just 2 minutes—there’s no obligation, no pressure, and no cost to check. Simply start your benefits check here, or call us directly at 561-203-6085 to speak with someone who understands what you’re going through.
If you’re in crisis right now, please call or text 988 immediately. You are not alone, and help is available 24/7.
Internal Links
- Intensive Outpatient Program (IOP) & Partial Hospitalization Program (PHP)
- Exposure and Response Prevention Therapy
- Verify Insurance
- Related Blog: How ERP Therapy Works for OCD
FAQ Schema (JSON-LD)
{
"@context": "https://schema.org",
"@type": "FAQPage",
"mainEntity": [
{
"@type": "Question",
"name": "How long do I need to take medication for OCD?",
"acceptedAnswer": {
"@type": "Answer",
"text": "Most people need to stay on medication for at least 12 months after symptoms improve. Some benefit from long-term or lifelong treatment to prevent relapse."
}
},
{
"@type": "Question",
"name": "Can I treat OCD without medication?",
"acceptedAnswer": {
"@type": "Answer",
"text": "Yes. Exposure and Response Prevention (ERP) therapy is highly effective, especially for mild to moderate OCD. For moderate to severe OCD, combining medication and ERP works best."
}
},
{
"@type": "Question",
"name": "Which SSRI is best for OCD?",
"acceptedAnswer": {
"@type": "Answer",
"text": "All SSRIs are considered equally effective. The best choice depends on your health history, side effects, and your provider’s recommendation."
}
},
{
"@type": "Question",
"name": "Are there OCD medications for children?",
"acceptedAnswer": {
"@type": "Answer",
"text": "Yes. FDA-approved options include sertraline (age 6+), fluoxetine (age 7+), fluvoxamine (age 8+), and clomipramine (age 10+). Children need close monitoring by a specialist."
}
},
{
"@type": "Question",
"name": "What if medication and therapy aren’t enough?",
"acceptedAnswer": {
"@type": "Answer",
"text": "If you have severe, treatment-resistant OCD, advanced options like intensive therapy or higher levels of care (such as IOP/PHP) may help. Learn about Thrive’s virtual IOP/PHP programs."
}
}
]
}