Mind on Repeat: A Guide to Obsessive Thoughts

What You Need to Know About Obsessive Thoughts
Obsessive thoughts are unwanted, intrusive, and recurring thoughts, images, or urges that cause distress and feel impossible to control. While everyone experiences occasional worries, obsessive thoughts become problematic when they dominate your thinking, trigger intense anxiety, and lead to repetitive behaviors (compulsions) that interfere with daily life.
Key differences between normal thoughts and obsessive thoughts:
| Normal Intrusive Thoughts | Obsessive Thoughts (OCD) |
|---|---|
| Occasional and fleeting | Persistent and recurring |
| Easy to dismiss or ignore | Feel “stuck” and hard to shake |
| Cause mild discomfort | Cause significant distress |
| Don’t disrupt daily life | Interfere with work, relationships, and functioning |
| No compulsive response needed | Trigger urges to perform rituals or compulsions |
Ever had a thought that just wouldn’t leave? A disturbing image that pops into your mind at the worst possible moment? An endless worry that loops like a broken record?
You’re not alone. Research shows we have over 6,000 thoughts daily—and not all of them are pleasant or welcome. For most people, these intrusive thoughts are fleeting annoyances. But for more than 6 million Americans, these thoughts become obsessions that trigger anxiety and compulsive behaviors, disrupting their ability to function.
The difference between a passing worry and an obsession isn’t the content of the thought—it’s what happens next. Do you shrug it off and move on? Or does the thought take hold, demanding your attention and driving you to perform rituals to make it stop?
This guide will help you understand what obsessive thoughts really are, how they differ from everyday worries, and what works to break free from them. Whether you’re questioning if your thoughts are “normal” or you’re already caught in the exhausting cycle of obsessions and compulsions, you’ll find clear, evidence-based answers here.
I’m Nate Raine, CEO of Thrive Mental Health. At Thrive, we specialize in intensive outpatient programs for OCD and related conditions, combining the latest research with compassionate, personalized care for clients throughout Florida.
Relevant articles related to obsessive thoughts:
Intrusive Thoughts vs. OCD Obsessions: What’s the Real Difference?

We all experience unwanted intrusive thoughts. Our brains are constantly generating a stream of consciousness, and sometimes, that stream carries “junk thoughts”—random, meaningless ideas, images, or urges that pop into our heads. For most people, these thoughts are like clouds passing in the sky; you notice them, and then they drift away.
However, for some, these thoughts can become “sticky.” Dr. Martin Seif and Dr. Sally Winston, experts in anxiety disorders, describe this phenomenon where unwanted intrusive thoughts get stuck, causing significant distress and anxiety. This “sticky mind” can turn a fleeting thought into a persistent, tormenting loop. You can learn more about this concept in their work, such as “Unwanted Intrusive Thoughts: Images, Sensations, and Stories.”
The crucial difference between a normal intrusive thought and an obsession in Obsessive-Compulsive Disorder (OCD) lies in how the thought is processed and the distress it causes. OCD obsessions are ego-dystonic, meaning they clash with a person’s values, beliefs, and sense of self. Someone with a loving nature might be tormented by violent images, or a devout individual might experience blasphemous thoughts. The sheer contradiction between the thought and their true character causes anguish, leading them to believe the thought is dangerous or meaningful.
This is why more than 6 million people in the United States are troubled by these persistent, distressing thoughts. They aren’t just annoying; they feel threatening and can consume hours of a person’s day.
Normal Worries vs. OCD Compulsions
It’s important to distinguish between everyday repetitive behaviors and OCD compulsions. Not every routine or habit signifies OCD. We all have rituals: our morning coffee routine, a specific way we prepare for bed, or how we approach learning a new skill. These are generally functional, often pleasurable, and don’t stem from intense anxiety or a need to prevent a catastrophic outcome.
OCD compulsions, on the other hand, are performed because of the intense anxiety generated by obsessive thoughts. They are not done for pleasure, but out of a need to reduce distress or prevent a feared event. The person often feels driven to perform them and would rather not, as they are time-consuming and often torturous.
| Normal Repetitive Behaviors | OCD Compulsions |
|---|---|
| Motivation: Functional, enjoyable, or practical. | Motivation: Driven by intense anxiety, fear, or distress from obsessive thoughts. |
| Impact: Do not significantly interfere with daily life. | Impact: Time-consuming (often over an hour a day), cause significant distress, and interfere with work, school, social life, and relationships. |
| Control: Can be easily stopped or altered. | Control: Feel uncontrollable, even if the person recognizes they are excessive or irrational. |
| Outcome: Achieve a desired positive outcome or routine. | Outcome: Aim to prevent a feared negative outcome or reduce anxiety, but only offer temporary relief. |
| Examples: Bedtime routine, religious practices, arranging tools efficiently, exercising regularly. | Examples: Excessive handwashing, checking locks repeatedly, counting, mental reviewing, seeking constant reassurance. |
For a deeper dive into the nature of these behaviors, you can explore more on compulsions and how they manifest.
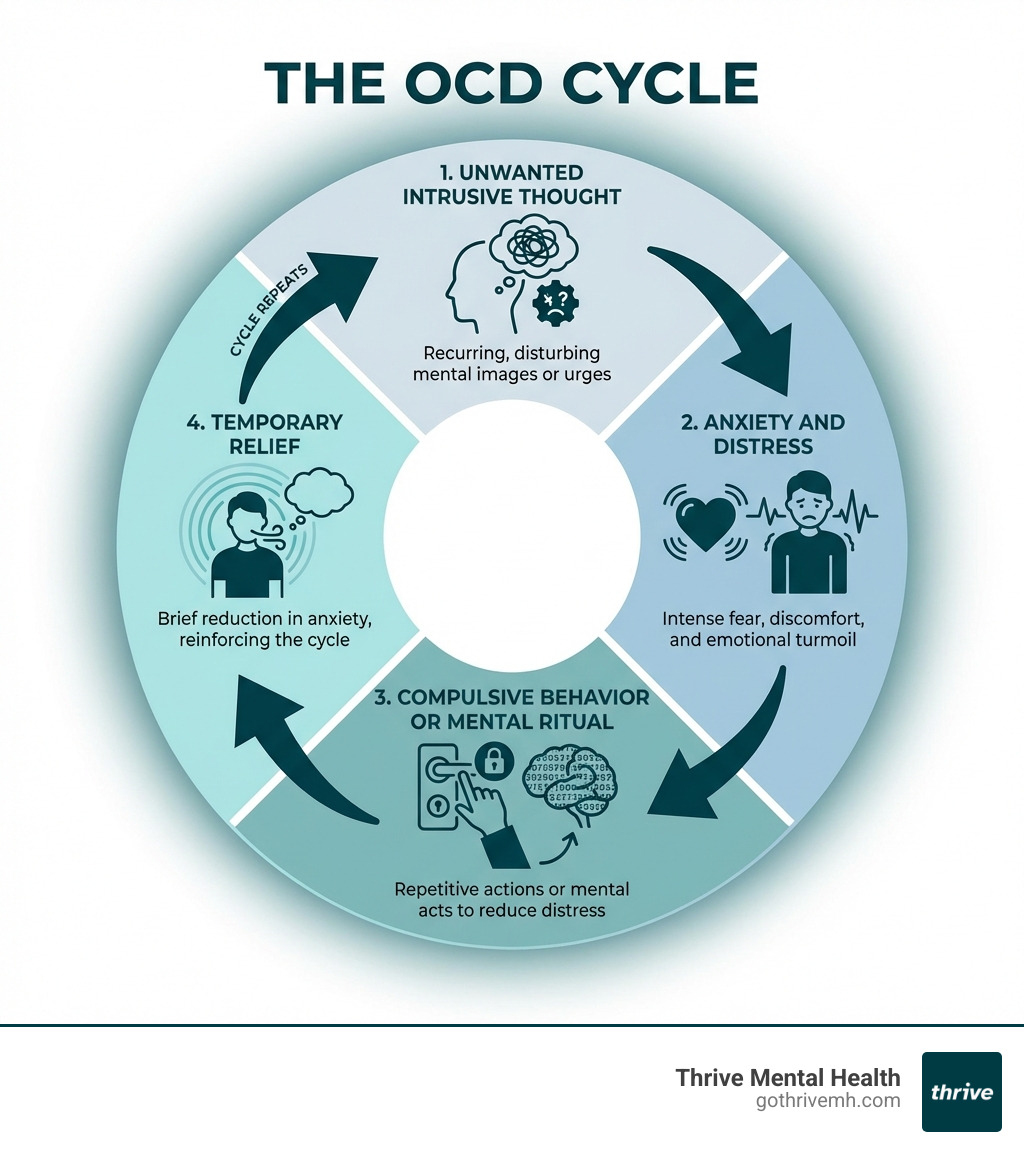
The Vicious Cycle: How Obsessive Thoughts Fuel Compulsions
The core of Obsessive-Compulsive Disorder is a self-perpetuating cycle. It begins with an obsession, which is an unwanted, intrusive thought, image, or urge. This obsession triggers intense anxiety or distress. To alleviate this feeling, the individual performs a compulsion—a repetitive behavior or mental act. This compulsion provides temporary relief, but it also reinforces the idea that the obsession was dangerous and the compulsion was necessary. The relief is short-lived, and soon, another obsessive thought emerges, restarting the cycle.
Common themes of obsessive thoughts
Obsessive thoughts can latch onto almost any theme, often targeting what a person values most or fears the most. Some common themes include:
- Contamination/Germs: Fear of dirt, germs, diseases, or environmental contaminants.
- Harm/Aggression: Thoughts or images of harming oneself or others, often without any intent to do so.
- Unwanted Sexual Thoughts: Disturbing sexual thoughts or images that feel taboo or inconsistent with one’s values.
- Religion/Scrupulosity: Preoccupation with moral or religious purity, fear of sinning, or intense guilt over perceived wrongdoing.
- Symmetry/Orderliness: A need for things to be “just right,” balanced, or in a specific order.
- Relationships (ROCD): Persistent doubts or worries about a romantic partner, their feelings, or one’s own feelings.
What are physical and mental compulsions?
Compulsions are the repetitive actions or mental acts performed in response to an obsession.
Physical Compulsions:
- Washing and Cleaning: Excessive handwashing, showering, or cleaning objects or surfaces.
- Checking: Repeatedly checking locks, appliances, light switches, or written work.
- Repeating: Doing actions multiple times (for example, walking through a doorway) to feel “right” or prevent a bad event.
- Ordering and Arranging: Lining up or arranging items symmetrically or in a specific pattern.
Mental Compulsions:
These are internal rituals that are not visible to others. This is often referred to as “Pure O” (Purely Obsessional OCD), though the term is misleading because compulsions are still present, even if they are mental. You can read more about pure O on the OCD-UK website.
Examples include:
- Mental Review: Ruminating over past events or conversations to gain certainty or ensure no harm was done.
- Praying/Repeating Words: Silently repeating specific phrases, prayers, or numbers to neutralize a bad thought.
- Counting: Performing tasks while counting to a “safe” number or in specific patterns.
- Thought Neutralization: Trying to “undo” a bad thought by thinking a “good” thought.
- Reassurance Seeking: Repeatedly asking others to confirm that things are okay or that one is not a “bad” person.
These compulsions, whether physical or mental, offer a brief escape from anxiety but ultimately keep the OCD cycle going. For a comprehensive overview of how these symptoms manifest, refer to our page on OCD Symptoms.
Could It Be OCD? [Signs, Causes, and When to Worry]

If you are struggling with thoughts of harming yourself or others, please call or text the 988 Suicide & Crisis Lifeline at 988 or chat at 988lifeline.org. You are not alone.
Distinguishing between typical worries and the signs of Obsessive-Compulsive Disorder can be challenging. Many people experience intrusive thoughts, but in OCD, these thoughts become all-consuming and lead to significant distress and impairment.
Here are some diagnostic clues that your obsessive thoughts might be indicative of OCD:
- Time-Consuming: Your obsessions and compulsions take up a significant amount of time, often more than one hour per day.
- Significant Distress: The thoughts cause intense anxiety, fear, guilt, or disgust.
- Impaired Functioning: The symptoms interfere with daily life, making it difficult to perform at work or school, maintain relationships, or engage in social activities.
- Lack of Pleasure: While compulsions might provide temporary relief from anxiety, they do not bring pleasure. You often feel driven to perform them, even if you recognize they are irrational.
If these signs resonate with your experience, it is a strong indicator that you should seek professional evaluation. Take our OCD Quiz for a preliminary assessment—it is not a diagnostic tool, but it can guide your next steps. Since professional treatment is often covered by insurance, you can verify your benefits in minutes to see what your plan includes.
What causes obsessive thoughts and OCD?
The exact cause of OCD is not fully understood, but research points to a combination of biological, genetic, and environmental factors.
- Genetics: Having a first-degree relative with OCD (a parent, sibling, or child) increases the likelihood of developing the disorder.
- Brain Structure and Biology: Studies show differences in the brain structure and function of individuals with OCD, particularly in areas related to fear, decision-making, and impulse control. Imbalances in neurotransmitters like serotonin may also play a role.
- Temperament: Certain temperamental traits in childhood, such as reserved behavior, negative emotions, anxiety, and depression, can be risk factors.
- Childhood Trauma and Stress: Experiencing childhood trauma or stressful life events can increase the risk of developing OCD or trigger its onset.
- PANDAS: In some cases, particularly in children, a sudden onset or worsening of OCD symptoms and tics can occur after a streptococcal infection. This condition is known as Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections (PANDAS).
OCD symptoms typically begin between late childhood and young adulthood, though they can start at any age. For more detailed information, visit the National Institute of Mental Health’s page on Obsessive-Compulsive Disorder (OCD). If you are questioning whether your experiences align with these patterns, our “Do I Have OCD?” resource can provide further insights: Do I Have OCD?.
The Gold Standard: How to Treat Obsessive Thoughts and OCD
When it comes to treating obsessive thoughts and OCD, effective, evidence-based treatments are available. While there is no cure in the sense of making the thoughts disappear forever, treatment can help you manage symptoms, reduce distress, and reclaim your life. The primary treatment approaches involve psychotherapy, often in combination with medication.
Psychotherapy, particularly Cognitive Behavioral Therapy (CBT), is considered the cornerstone of OCD treatment. Medications, primarily Selective Serotonin Reuptake Inhibitors (SSRIs), can also be helpful in managing symptoms, especially for moderate to severe cases.
Exposure and Response Prevention (ERP) Therapy
ERP is considered the gold standard of psychotherapy for OCD and is effective in many cases. It is a type of CBT that directly targets the cycle of obsessions and compulsions.
ERP involves gradually exposing you to the situations, thoughts, or images that trigger your obsessions and anxiety, while preventing you from engaging in your usual compulsive behaviors or mental rituals. The core idea is to teach your brain that the feared outcome will not happen, and that you can tolerate the anxiety without performing compulsions.
For example, if you have a contamination obsession, ERP might involve touching a “dirty” object (exposure) and then resisting the urge to wash your hands (response prevention). Over time, your brain learns a new response. The anxiety naturally decreases through a process called habituation, and the power of the obsession weakens.
We leverage ERP in our Intensive Outpatient (IOP) and PHP programs, helping Florida residents regain control with specialized care available both in-person and virtually. You can explore more about this therapy on our dedicated page: Exposure and Response Prevention Therapy.
Cognitive Behavioral Therapy (CBT)
CBT is a broader therapeutic approach that encompasses ERP and is valuable in treating OCD. While ERP focuses on changing behaviors, CBT also helps you identify and challenge the cognitive distortions and unhelpful thought patterns that fuel your obsessions.
In CBT, you work to:
- Identify Obsessive Thoughts: Recognize the specific thoughts, images, or urges that trigger your distress.
- Challenge Cognitive Distortions: Question the validity and helpfulness of these thoughts.
- Develop Alternative Responses: Learn new ways to respond to obsessive thoughts that do not involve compulsions.
Experts like Dr. Martin Seif, a co-founder of ADAA and a clinician in anxiety disorders, have helped develop and refine these treatment methods. You can learn more about Dr. Seif and his contributions to anxiety treatment.
CBT, especially when combined with ERP, gives you tools to manage your obsessive thoughts and break free from the cycle of OCD. To understand the full spectrum of available treatments, including medication options, visit our guide on How to Treat OCD.
7 Daily Strategies to Manage Intrusive Thoughts [Actionable Tips]
Living with intrusive thoughts can feel overwhelming, but there are strategies you can use in daily life to manage them. These tips, rooted in principles of CBT and mindfulness, can help you change your relationship with these thoughts and reduce their impact.
- Label the Thought: When an unwanted thought pops up, acknowledge it as “an intrusive thought” or “an OCD thought.” This creates distance, reminding you that it is just a thought, not a command or a reflection of your character.
- Accept, Don’t Fight: Trying to suppress distressing thoughts can make them more persistent. Instead, practice accepting that the thought is there. You do not have to like it or agree with it; simply allow it to exist without engaging.
- Practice Mindfulness/Meditation: Mindfulness helps you observe your thoughts and feelings without judgment. It trains you to stay present, rather than getting pulled into mental spirals. Studies show that mindfulness can reduce negative responses to distressing thoughts and imagery.
- Ground Yourself in the Present: When obsessive thoughts start to take over, engage your senses to reconnect with your environment. For example, notice several things you can see, touch, hear, smell, and taste.
- Delay the Compulsion: If you feel an urge to perform a compulsion, try delaying it, even for a few minutes. Tell yourself, “I will wait.” Often, the urge will lessen during that delay. Gradually extend the delay to show yourself that you can tolerate the discomfort.
- Identify Your Triggers: Notice what situations, emotions, or physical states (such as stress or lack of sleep) tend to precede your obsessive thoughts. Recognizing these triggers can help you prepare and apply coping strategies early.
- Prioritize Self-Care: Consistent sleep, a healthy diet, and regular exercise support your overall resilience. These habits are not cures, but they make it easier to handle distress.
The goal is not to eliminate all intrusive thoughts—that is not realistic. The goal is to change your reaction so they lose their power over you. While these strategies can provide relief, breaking the cycle of severe obsessive thoughts often requires more structured support. A Florida-based Intensive Outpatient Program (IOP) can provide the structured, local support needed for lasting change. For more insights into managing these thoughts, explore our resource on Intrusive Thoughts OCD.
When to Seek Professional Help in Florida [And Where to Find It]
It is natural to wonder when your obsessive thoughts cross the line from a common human experience to a condition requiring professional intervention. Certain signs indicate it is time to seek expert help:
- Quality of Life Impacted: Your obsessions and compulsions significantly interfere with daily life, relationships, work, or school.
- Time Consumption: You spend more than an hour a day on obsessive thoughts or compulsive behaviors.
- Significant Distress: The thoughts cause anxiety, fear, guilt, or disgust that you find difficult to manage.
- Impaired Functioning: You avoid situations or cannot complete tasks because of your symptoms.
- Suicidal Thoughts: If your distress leads to thoughts of harming yourself or others, seek immediate help.
Callout Box:
If you are in crisis, call or text 988 right now. You are not alone.
At Thrive Mental Health, we understand that finding the right support is crucial. We offer a spectrum of care designed to meet varying needs:
- Weekly Therapy: For individuals with mild to moderate symptoms who can manage with regular outpatient sessions.
- Intensive Outpatient Programs (IOP): For those who need more structure than weekly therapy but do not require inpatient care. Our IOPs provide several hours of therapy per day, multiple days a week, focusing on evidence-based treatments like ERP and CBT. We offer both virtual and in-person IOPs in locations across Florida, including Tampa Bay, St. Petersburg, Miami, Orlando, Boca Raton, West Palm Beach, Jacksonville, Fort Lauderdale, Naples, and Sarasota.
- Partial Hospitalization Programs (PHP): For individuals needing a higher level of care, our PHPs offer more intensive, full-day treatment and can serve as a step-down from inpatient care or an alternative to hospitalization.
Our specialized programs, including our Virtual IOP for OCD, are designed for adults and young professionals, combining clinical expertise with flexible scheduling. We work with major insurance providers such as Cigna, Optum, Florida Blue, and Aetna to make treatment accessible. We can help you verify your benefits and understand your options.
When your thoughts are taking over, professional help can provide the tools and support you need to regain control.
Frequently Asked Questions about Obsessive Thoughts
Can obsessive thoughts go away on their own?
While mild intrusive thoughts can fade, OCD-related obsessive thoughts typically require treatment like ERP to resolve. They rarely disappear without intervention and can worsen over time.
Are obsessive thoughts a sign of psychosis?
No. A key feature of OCD is that the individual recognizes the thoughts are a product of their own mind, even if they feel uncontrollable and distressing. This insight into reality is different from psychosis, where a person may lose touch with reality and believe their thoughts or delusions are real.
How do I know if my intrusive thoughts are “bad enough” for therapy?
If your thoughts cause significant distress, take up more than an hour of your day, or interfere with your work, relationships, or ability to enjoy life, it is time to seek professional help. If you are questioning whether they are “bad enough,” that is often a sign that they are already impacting you more than you realize.
Conclusion: Take Back Control From Your Thoughts
Living with obsessive thoughts can feel like a constant battle. But you are not your thoughts. Intrusive, unwanted ideas are often just signals from an overactive brain, not reflections of your true desires or intentions.
Effective, evidence-based treatment is available. Through approaches like Exposure and Response Prevention (ERP) and Cognitive Behavioral Therapy (CBT), you can learn to challenge the power of these thoughts, break free from compulsive behaviors, and regain a sense of control. Thrive Mental Health offers specialized virtual and in-person IOP/PHP programs for OCD, designed for adults and young professionals across Florida.
Ready for support? Thrive offers virtual and hybrid IOP/PHP programs with evening options. Verify your insurance in 2 minutes (no obligation) → Start benefits check or call 561-203-6085. If you are in crisis, call or text 988.