Navigating CPTSD: Your Comprehensive Overview

What Complex PTSD Really Means—And Why Understanding It Changes Everything
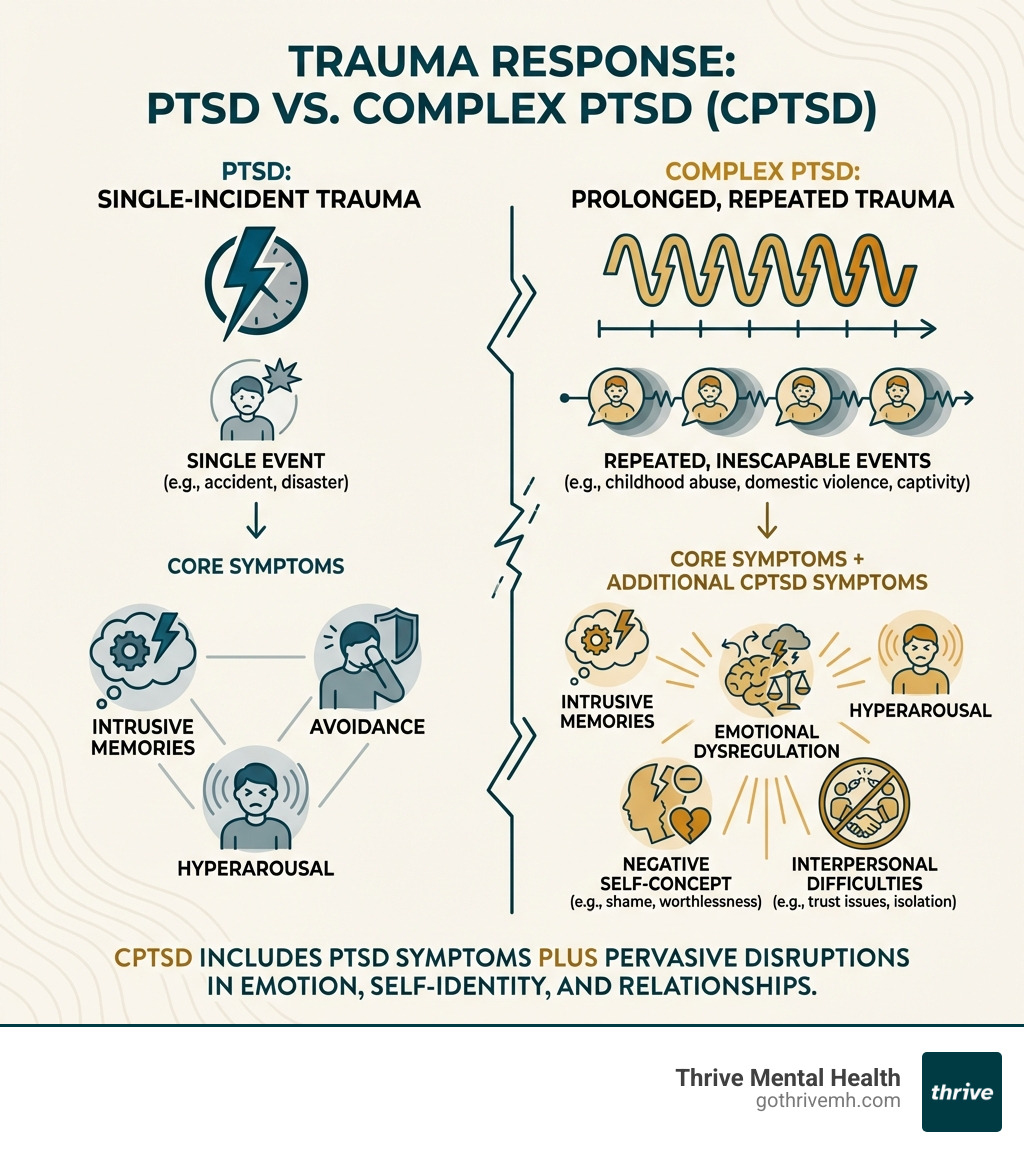
Complex PTSD is a mental health condition that develops after prolonged, repeated trauma—especially trauma you couldn’t escape. Unlike standard PTSD, which typically follows a single traumatic event, complex PTSD emerges from chronic abuse, neglect, or violence that happened over months or years.
Quick Answer: What is Complex PTSD?
| Aspect | What You Need to Know |
|---|---|
| What it is | A trauma disorder from repeated exposure to inescapable traumatic events |
| Key symptoms | PTSD symptoms + emotional dysregulation, negative self-image, relationship difficulties |
| Common causes | Childhood abuse/neglect, domestic violence, human trafficking, war, prolonged bullying |
| Diagnosis | Recognized in ICD-11; not separate in DSM-5 (included under PTSD) |
| Prevalence | Affects 1–8% of the global population; 4% in developed nations, 15% in war-exposed regions |
| Treatment | Trauma-focused therapy (CBT, EMDR), phase-based treatment, medication for co-occurring symptoms |
If you’ve experienced long-term trauma and struggle with intense shame, difficulty trusting others, or feeling disconnected from yourself, you’re not alone—and you’re not broken. Complex PTSD is a normal response to abnormal circumstances.
This condition doesn’t just affect your memories. It changes how you see yourself, how you relate to others, and how you move through the world. You might feel stuck in patterns of self-blame, struggle to regulate your emotions, or find it nearly impossible to trust anyone—even people who genuinely care about you.
The good news? Complex PTSD is treatable. With the right support, you can process what happened, rebuild your sense of self, and create a life that feels safe and fulfilling.
I’m Nate Raine, CEO of Thrive Mental Health, where we’ve helped thousands of adults recover from complex PTSD through evidence-based, trauma-informed programs across Florida. Our work integrates cutting-edge research with compassionate, personalized care designed to meet you where you are.
Complex ptsd helpful reading:
What Is Complex PTSD (CPTSD) and How Is It Different From PTSD?
When we talk about trauma, many people think of Post-Traumatic Stress Disorder (PTSD), which typically arises from a single, distinct event like a car accident or a natural disaster. However, complex PTSD (CPTSD) is a distinct condition that develops from prolonged, repeated, and often inescapable traumatic experiences. Think of it as a deeper, more pervasive type of trauma response that impacts your entire being.
The primary difference lies in the nature of the trauma and the resulting symptom profile. While both conditions involve classic PTSD symptoms such as re-experiencing the trauma (flashbacks, nightmares), avoidance behaviors, and hyperarousal (being on edge, easily startled), complex PTSD includes additional, profound disturbances in emotional regulation, self-perception, and relationships.
Let’s break down the key differences:
| Feature | Post-Traumatic Stress Disorder (PTSD) | Complex Post-Traumatic Stress Disorder (CPTSD) |
|---|---|---|
| Trauma Type | Single, acute, time-limited event (e.g., car crash, natural disaster, assault) | Prolonged, repeated, inescapable trauma (e.g., childhood abuse/neglect, domestic violence, human trafficking, war, torture) |
| Core Symptoms | Re-experiencing, Avoidance, Negative alterations in cognition/mood, Hyperarousal | All PTSD symptoms PLUS: Disturbances in Self-Organization (DSO): Emotional dysregulation, Negative self-concept, Interpersonal difficulties |
| Impact on Self | Primarily affects reactions to trauma; sense of self generally intact | Profoundly impacts identity, self-worth, and ability to relate to others |
| Onset | Can occur at any age after a single event | Often results from early-life, developmental trauma, but can occur at any age |
| Diagnostic Status | Recognized in DSM-5 and ICD-11 | Recognized as a distinct diagnosis in ICD-11; symptoms often captured within PTSD with dissociative features or other diagnoses in DSM-5 |
Key Differences in Symptoms and Causes
The causes of PTSD often involve a single, overwhelming event. For example, a veteran might develop PTSD after a combat incident, or someone might experience it after a violent attack. These are often referred to as single-incident traumas. While devastating, the individual’s core sense of self and ability to form relationships may remain relatively intact prior to the event.
In contrast, complex PTSD stems from chronic interpersonal trauma, meaning the trauma occurred within relationships and over an extended period. This can include:
- Childhood abuse or neglect: Physical, emotional, or sexual abuse by caregivers. Studies show that childhood trauma can significantly affect brain development, making it difficult for children to develop a sense of safety or stability.
- Domestic violence: Long-term abuse within an intimate relationship. One study found that complex PTSD was twice as common as PTSD in survivors of intimate partner violence.
- Human trafficking: Forced labor or commercial sex work. Reports indicate approximately 41% of human trafficking survivors develop complex PTSD.
- War or captivity: Prolonged exposure to extreme violence or being held captive.
- Severe bullying: Chronic and inescapable bullying, especially during formative years.
These experiences are often referred to as developmental trauma because they occur during critical periods of development, fundamentally shaping an individual’s sense of self, emotional regulation, and relational patterns. The resulting Disturbances in Self-Organization (DSO) are what truly set complex PTSD apart.
Why the “Complex” Matters for Your Healing Journey
The “complex” in complex PTSD isn’t just a descriptor; it signifies the intricate, pervasive impact these prolonged traumas have on an individual. This includes:
- Impact on identity: Survivors often struggle with a fragmented sense of self, feelings of worthlessness, shame, and guilt. They might believe they are inherently bad or undeserving of love and safety.
- Relational patterns: Chronic interpersonal trauma, especially betrayal trauma, can shatter the ability to trust others. This leads to difficulties forming healthy attachments, a fear of abandonment, or a tendency to repeat unhealthy relationship dynamics. We understand that developing healthy relationship patterns is a key step in recovery.
- Emotional regulation: The ability to manage and express emotions appropriately is severely compromised. This can manifest as intense mood swings, explosive anger, persistent sadness, or emotional numbness.
Understanding these complexities is crucial because it directly influences the treatment path. Standard PTSD treatments may not fully address the deep-seated issues of identity and relationship disturbance inherent in complex PTSD. For a deeper dive into how trauma shapes us, read our Beginners Guide to Understanding Trauma.
The Hidden Wounds: Recognizing the Symptoms of Complex PTSD
Complex PTSD can manifest in a myriad of ways, extending far beyond the typical fear-based responses seen in PTSD. These are the “hidden wounds” that often go unrecognized, making daily life incredibly challenging.

Core Symptoms of Complex PTSD You Can’t Ignore
Beyond the common PTSD symptoms like flashbacks, avoidance, and hypervigilance, individuals with complex PTSD often experience a cluster of symptoms related to their sense of self, emotional world, and relationships. These include:
- Emotional Dysregulation: This is a hallmark of complex PTSD. It involves intense and unpredictable mood swings, difficulty managing emotions, and feeling overwhelmed by emotional reactions. This can lead to explosive anger, persistent sadness, or extreme emotional numbness.
- Negative Self-Concept: A profound sense of worthlessness, shame, and guilt is common. Individuals may believe they are fundamentally flawed, bad, or responsible for the trauma they endured. This often leads to self-blame and low self-esteem.
- Interpersonal Difficulties: Forming and maintaining healthy relationships becomes incredibly challenging. This can involve difficulty trusting others, a fear of abandonment, a tendency to isolate, or patterns of unhealthy attachment. Our past trauma can influence our present relationships, and we often see clients struggling with How Abandonment Trauma Influences Your Relationships.
- Dissociation: Feeling disconnected from oneself, one’s body, or the world. This can manifest as periods of “spacing out,” feeling detached from reality, or experiencing memory gaps related to the trauma. Dissociation is a coping mechanism developed during inescapable trauma.
- Somatization: Many people with complex PTSD experience physical symptoms in response to mental distress. This is when psychological pain manifests physically. Common physical symptoms can include:
- Headaches
- Dizziness
- Chest pains
- Chronic fatigue
- Digestive issues
- Generalized chronic pain
These symptoms create a continuous cycle of distress, impacting every facet of an individual’s life. If you’re experiencing suicidal thoughts, please know there’s help available right now.
Crisis Support: If you are in crisis or having thoughts of suicide, call or text 988 to reach the Suicide & Crisis Lifeline. You are not alone.
How Chronic Trauma Rewires Your Brain and Body
Chronic trauma, especially during childhood, has a profound impact on brain development. Studies have shown that early, repeated trauma can alter brain structure, function, and connectivity, particularly in areas responsible for emotion regulation, memory, and stress response.
The effects of childhood maltreatment on the brain include changes in the prefrontal cortex (involved in decision-making and emotional control) and the amygdala (involved in fear processing). This can lead to a heightened fight-flight-freeze-fawn response, where the body is constantly on high alert, reacting to perceived threats even when objectively safe. This chronic state of arousal can contribute to physical health problems and make it difficult to relax or feel calm.
Furthermore, trauma can impact memory, leading to difficulties recalling specific events or experiencing fragmented memories. This is not uncommon, and we often explore Can Trauma Cause Memory Loss? with our clients. The brain’s attempt to protect itself by dissociating or fragmenting memories can make it harder to process the trauma later on.
Getting the Right Diagnosis: Is It CPTSD or Borderline Personality Disorder (BPD)?
One of the most challenging aspects of complex PTSD is its significant symptom overlap with other conditions, particularly Borderline Personality Disorder (BPD). This overlap often leads to misdiagnosis, which can delay appropriate treatment and cause further distress.

The Critical Distinctions That Define Your Treatment Path
Both complex PTSD and BPD can present with intense emotional dysregulation, impulsive behaviors, and unstable relationships. However, the underlying drivers and core fears often differ.
| Feature | Complex PTSD (CPTSD) | Borderline Personality Disorder (BPD) |
|---|---|---|
| Primary Cause | Prolonged, inescapable trauma (often interpersonal) | Complex interplay of genetic predisposition, brain chemistry, and environmental factors (trauma is a risk factor, but not always the sole cause) |
| Core Fear | Fear of betrayal, re-victimization, lack of safety/trust | Fear of abandonment, rejection, being alone |
| Self-Concept | Negative self-perception (worthless, shameful) due to trauma-based identity disturbance | Unstable self-image, identity diffusion, chronic feelings of emptiness |
| Relationship Patterns | Difficulty trusting, fear of intimacy, repeating trauma-informed dynamics | Intense, unstable relationships, idealization/devaluation, frantic efforts to avoid abandonment |
| Treatment Focus | Processing trauma, rebuilding self, developing emotional regulation & healthy relationships | Emotional regulation, interpersonal effectiveness, distress tolerance, identity development |
While there’s a strong association between childhood trauma and BPD, trauma isn’t always the direct cause of BPD. For complex PTSD, chronic trauma is a prerequisite for diagnosis.
The diagnostic landscape adds to the confusion. While the World Health Organization (WHO) included complex PTSD (6B41) as a distinct diagnosis in its ICD-11, the American Psychiatric Association (APA) does not recognize it as separate in the DSM-5. Instead, the DSM-5 includes a dissociative subtype of PTSD that captures some of the complex PTSD symptoms. This divergence means that depending on where you are and who you see, your diagnosis might differ.
Some experts believe complex PTSD, PTSD, and BPD may exist on a spectrum. The key is that an accurate diagnosis is paramount for effective treatment. We’ve seen how a misdiagnosis can lead to ineffective interventions, prolonged suffering, and even re-traumatization.
How to Talk to Your Doctor About a Potential Misdiagnosis
If you suspect your diagnosis might not fully capture your experiences, or if you’re worried that the treatment you’re receiving isn’t addressing your core issues, we encourage you to advocate for yourself. Here’s how:
- Educate yourself: Understand the symptoms of complex PTSD and how they differ from other conditions.
- Open communication: Discuss your concerns openly and honestly with your mental health professional. Share why you believe complex PTSD might be a better fit for your experiences.
- Ask about ICD-11 criteria: Since complex PTSD is recognized in the ICD-11, you can ask your provider if they are familiar with these criteria and how they compare to your symptoms.
- Seek a trauma-informed specialist: If your current provider is not familiar with complex PTSD or trauma-informed care, consider seeking a second opinion from a specialist who has extensive experience with complex trauma. These clinicians are trained to look beyond surface-level symptoms and understand the deep impact of chronic adversity. We understand the unique challenges of Understanding the Childhood Trauma Test: What You Need to Know and can guide you through the process.
An accurate diagnosis is your first step toward a recovery path that truly works.
Healing is Possible: Evidence-Based Treatments for Complex PTSD [2025 Guide]
Healing from complex PTSD is not about erasing the past, but about integrating your experiences, rebuilding your sense of self, and developing effective coping strategies to live a fulfilling life. While the journey can be challenging, we want you to know that significant recovery is absolutely possible.
Crisis Support: If you are in crisis or having thoughts of suicide, call or text 988 to reach the Suicide & Crisis Lifeline. You are not alone.
Because complex PTSD often involves deep-seated issues related to identity, relationships, and emotional regulation, a phased treatment approach is often recommended. This generally involves three stages:
- Stabilization and Safety: This initial phase focuses on establishing a sense of safety (both internal and external), developing emotional regulation skills, and building coping mechanisms. This is crucial before processing traumatic memories to prevent re-traumatization.
- Trauma Processing and Remembrance: Once stable, individuals can begin to process and integrate traumatic memories. This involves safely recalling and working through the emotions and narratives associated with the trauma.
- Integration and Reconnection: The final phase centers on integrating new coping skills into daily life, rebuilding healthy relationships, enhancing self-esteem, and finding meaning and purpose after trauma.
At Thrive Mental Health, we offer virtual and in-person Intensive Outpatient (IOP) and Partial Hospitalization (PHP) programs designed specifically for adults and young professionals struggling with complex PTSD. Our programs are available across Florida, including in Tampa Bay, St. Petersburg, Miami, Orlando, Boca Raton, West Palm Beach, Jacksonville, Fort Lauderdale, Naples, and Sarasota. We work with major insurance providers like Cigna, Optum, and Florida Blue to make treatment accessible.
What are the recommended treatment approaches for complex PTSD?
A combination of therapeutic interventions is often most effective for complex PTSD. Here are some of the leading evidence-based approaches we use:
- Trauma-Focused Cognitive Behavioral Therapy (TF-CBT): This therapy helps individuals identify and change negative thought patterns and behaviors related to their trauma. It’s often considered a gold standard for psychotherapy and is highly effective in treating PTSD and complex PTSD. We empower our clients to understand How CBT Can Transform Negative Thought Patterns.
- Eye Movement Desensitization and Reprocessing (EMDR): EMDR therapy helps process traumatic memories and reduce their emotional impact. It’s a powerful tool for integrating distressing experiences and is widely recognized for its effectiveness in trauma recovery. Find more in our EMDR Complete Guide.
- Dialectical Behavior Therapy (DBT): Originally developed for BPD, DBT is highly effective for complex PTSD due to its focus on emotional regulation, distress tolerance, interpersonal effectiveness, and mindfulness. It provides concrete skills to manage intense emotions and steer challenging relationships.
- Skills Training in Affective and Interpersonal Regulation (STAIR): This phase-based treatment specifically targets the emotional dysregulation and relationship difficulties common in complex PTSD. It helps individuals develop skills before engaging in direct trauma processing.
- Somatic Therapies: Approaches like Sensorimotor Psychotherapy and Somatic Experiencing focus on the body’s response to trauma. They help individuals release stored trauma from the body, reduce physical symptoms of distress, and reconnect with their bodily sensations in a safe way.
- Medication: While not a standalone treatment for complex PTSD, medication (such as antidepressants) can help manage co-occurring symptoms like depression, anxiety, or sleep disturbances, making therapy more effective.
Self-Help Strategies to Manage Symptoms and Reclaim Your Life
Alongside professional treatment, integrating self-help strategies into your daily life is vital for managing complex PTSD symptoms and fostering resilience.
- Grounding Techniques: When feeling overwhelmed or dissociated, grounding techniques can help you reconnect with the present moment. This might involve focusing on your five senses, describing your surroundings, or using a grounding object.
- Mindfulness: Practicing mindfulness can increase your awareness of your thoughts, feelings, and bodily sensations without judgment. This helps in emotional regulation and staying present.
- Establishing Safety: Create a safe physical and emotional environment. This might involve setting boundaries in relationships, decluttering your living space, or having a trusted support system.
- Setting Boundaries: Learning to say no, protecting your energy, and asserting your needs are crucial steps in reclaiming your personal power and preventing re-victimization.
- Journaling: Writing down your thoughts and feelings can be a powerful way to process emotions, identify triggers, and gain insight into your patterns.
- Self-Care: Prioritize activities that nourish your mind, body, and spirit. This could be exercise, spending time in nature, pursuing hobbies, or simply resting. Self-care is not a luxury; it’s a necessity for healing. We provide Effective strategies for managing trauma and its triggers to empower our clients daily.
Frequently Asked Questions about Complex PTSD
Can you have both CPTSD and BPD?
Yes, it’s absolutely possible to have co-occurring diagnoses of both complex PTSD and BPD. While they share many overlapping symptoms, they are considered distinct conditions with different underlying etiologies. Complex PTSD stems directly from prolonged, inescapable trauma, whereas BPD is a personality disorder with a complex interplay of genetic, neurobiological, and environmental factors, though trauma is a significant risk factor for BPD. A trauma-informed clinician is essential to distinguish between them and create an effective, integrated treatment plan that addresses both sets of symptoms.
Can complex PTSD be cured?
While “cured” might not be the right word in the sense of completely erasing every memory or impact, significant recovery is absolutely possible. The goal of treatment for complex PTSD is not to forget the trauma, but to process it, reduce its overwhelming power, and integrate it into your life story in a way that allows you to move forward. With effective treatment, individuals can learn to manage symptoms, regulate emotions, rebuild a stable sense of self, and form healthy relationships, leading to a fulfilling life. The impact of trauma can be profoundly reduced, enabling thriving rather than just surviving.
What does a CPTSD emotional flashback feel like?
Unlike a traditional PTSD flashback, which often involves re-experiencing the traumatic event with vivid sensory details (seeing, hearing, smelling), an emotional flashback in complex PTSD is different. It involves being suddenly and thrown back into the emotional state of the original trauma, without necessarily having clear visual memories. You might feel overwhelming shame, intense fear, profound hopelessness, utter powerlessness, or deep emptiness, as if you are that helpless child or trapped victim again. This can be incredibly confusing and overwhelming because there’s often no obvious trigger or clear memory attached, making it hard to understand what’s happening or why you feel that way.
How do you support someone with CPTSD?
Supporting someone with complex PTSD requires patience, empathy, and a trauma-informed approach. Here’s how we advise loved ones:
- Educate yourself: Learn about complex PTSD to understand their experiences better.
- Practice patience and empathy: Recognize that their behaviors and reactions are often trauma responses, not personal attacks.
- Offer a non-judgmental listening ear: Be present and listen without trying to “fix” them or offer unsolicited advice.
- Respect boundaries: Individuals with complex PTSD often have difficulty with boundaries. Respecting theirs is crucial for building trust.
- Encourage professional help: Gently suggest and support their journey to seek professional treatment, but avoid pressuring them.
- Avoid minimizing or blaming: Statements like “just get over it” or “it’s all in your head” are incredibly damaging. Validate their feelings and experiences.
- Prioritize your own self-care: Supporting someone with complex PTSD can be emotionally taxing. Ensure you have your own support system and practice self-care.
Your Path to Recovery Starts Now
Complex PTSD is a profound injury, but it does not have to be a life sentence. Understanding its unique features is the first step toward targeted, effective healing. With the right support and evidence-based care, you can process the past and build a future defined by strength and resilience. Thrive Mental Health provides expert-led, trauma-informed programs designed for adults who are ready to heal.
Ready for support? Thrive offers virtual and hybrid IOP/PHP programs with evening options. Verify your insurance in 2 minutes (no obligation) → Start benefits check or call 561-203-6085. If you’re in crisis, call/text 988.