Navigating United Health: In-Network Mental Health Services
Why Finding IOP Providers That Work With the United Health Company for Mental Health Services Matters
IOP providers that work with the united health company for mental health services are more accessible than you might think—but finding them requires knowing where to look and how your benefits actually work. If you’re struggling with anxiety, depression, or burnout and weekly therapy isn’t enough, an Intensive Outpatient Program (IOP) could be your next step. The good news: UnitedHealthcare (including plans managed by Optum) typically covers IOP treatment when it’s medically necessary, often through a large network of providers across the country.
Quick Answer: How to Find UHC-Covered IOP Providers
- Check the Optum provider directory at liveandworkwell.com (access code: “united”)
- Call the number on your UHC ID card to verify specific benefits and get a list of in-network IOPs
- Use the MyUHC portal at myuhc.com to search for behavioral health providers
- Contact prospective IOP providers directly and ask them to verify your coverage before starting treatment
- Consider virtual IOPs that accept UHC and serve Florida residents
What You Need to Know:
- Most UHC plans cover IOPs for conditions like depression, anxiety, PTSD, bipolar disorder, and co-occurring substance use disorders
- Prior authorization is typically required before starting IOP treatment
- In-network providers significantly reduce your out-of-pocket costs (average copays around $30/session vs. potentially full cost out-of-network)
- Virtual IOPs are often covered with the same benefits as in-person care
- Medical necessity is determined by the severity of your symptoms and whether less intensive treatment (like weekly therapy) has been insufficient
Finding the right level of care can feel overwhelming, especially when you need more than weekly therapy but don’t require hospitalization. IOPs fill this gap, offering structured treatment while you maintain your daily life. But navigating your UnitedHealthcare benefits to find and pay for this care can be confusing.
This guide cuts through the jargon. We’ll show you exactly how to find IOP providers that work with the united health company for mental health services, what to expect for costs, and how to verify your coverage to get the help you need.
About the Author:
I’m Nate Raine, CEO of Thrive Mental Health. With over a decade of experience in behavioral health systems, I’ve helped countless individuals steer complex insurance networks like UnitedHealthcare to access high-quality IOP treatment. At Thrive, we work directly with UHC and Optum across Florida to make care accessible and affordable.
IOP providers that work with the united health company for mental health services vocabulary:
- intensive outpatient programs in florida
- united healthcare insurance coverage for mental health in florida
Your UHC/Optum Plan & IOP: What’s Actually Covered (And What It Costs)
The good news is that UnitedHealthcare (UHC) generally covers Intensive Outpatient Programs (IOPs) for mental health. UHC’s behavioral health benefits are managed through Optum, which has an extensive network of over 210,000 practitioners, making it likely you’ll find in-network IOP providers that work with the united health company for mental health services. Thanks to mental health parity laws, UHC covers mental health conditions with the same priority as physical health conditions.
However, coverage depends on two key factors: medical necessity and prior authorization. Medical necessity means a healthcare professional has determined an IOP is the right level of care for your diagnosis, and less intensive options aren’t sufficient. Prior authorization is the process where your provider submits your treatment plan to UHC/Optum for approval before you begin. Reputable IOP providers handle this process for you.
Choosing in-network versus out-of-network providers is crucial for managing costs. Your out-of-pocket expenses will be significantly higher with out-of-network providers, and some services may not be covered at all. Sticking with in-network providers saves you money and simplifies the claims process.
Studies confirm the effectiveness of structured therapy like IOPs, with many patients showing significant improvement within months.

What Mental Health Conditions Does UHC Cover for IOP?
UnitedHealthcare’s coverage for IOPs extends to a broad spectrum of mental health conditions, provided they are deemed medically necessary. We’ve seen UHC policies cover IOPs for:
- Depression: IOPs provide intensive support for managing symptoms of major or persistent depressive disorder.
- Anxiety Disorders: IOPs offer tools to manage generalized anxiety, panic disorder, and social anxiety. With nearly a third of U.S. adults reporting anxiety or depression symptoms, effective treatment is critical.
- Post-Traumatic Stress Disorder (PTSD): IOPs provide specialized, trauma-focused therapies in a supportive group environment.
- Bipolar Disorder: IOPs help individuals manage mood swings, maintain medication adherence, and build stability.
- Co-occurring Disorders: UHC often covers integrated treatment for dual diagnoses, like mental health and substance use disorders. IOP outcomes for substance use can be comparable to residential programs.
- Obsessive-Compulsive Disorder (OCD): Intensive therapy within an IOP is highly effective for managing OCD.
- Trauma: IOPs help individuals process various forms of trauma and build resilience.
- Attention-Deficit/Hyperactivity Disorder (ADHD): IOPs offer behavioral therapy and skill-building for adults whose daily life is impacted by ADHD.
Specific coverage can vary by your individual plan and the severity of your symptoms. Always verify with UHC or your chosen provider.
Breaking Down Your Costs: Deductibles, Copays, and Coinsurance
Navigating the financial side of mental health care can be confusing, but understanding a few key terms will empower you to make informed decisions about IOP providers that work with the united health company for mental health services.
- Deductible: The amount you pay for covered services before your insurance starts paying. For example, if your deductible is $1,000, you pay the first $1,000 of IOP costs.
- Copayment (Copay): A fixed amount you pay for a service after meeting your deductible. For IOP, this might be a set fee per session (e.g., $30).
- Coinsurance: The percentage of costs you pay after meeting your deductible. If your coinsurance is 20%, you pay 20% of the bill, and UHC pays 80%.
- Out-of-Pocket Maximum: The most you’ll pay for covered services in a year. After you hit this limit, UHC pays 100% of covered costs, providing a financial safety net.
Here’s a simplified comparison of potential costs for in-network vs. out-of-network IOP:
| Cost Component | In-Network IOP (Example) | Out-of-Network IOP (Example) |
|---|---|---|
| Deductible | Applies (e.g., $1,000) | Applies (may be separate, higher OON deductible) |
| Copay | $30 per session (after deductible) | Often no copay; you pay full rate, then seek reimbursement |
| Coinsurance | 20% (after deductible) | 40-50% or more (after OON deductible), or no coverage at all |
| Total Cost | Lower, predictable, capped by out-of-pocket maximum | Significantly higher, less predictable, full provider rate may be charged |
| Prior Auth | Handled by provider | Often patient’s responsibility |
Does UHC Cover Virtual IOP Providers That Work With the United Health Company for Mental Health Services?
Yes, UnitedHealthcare plans frequently cover virtual IOPs. This telehealth coverage is a lifeline for those needing flexible and accessible mental health support. At Thrive Mental Health, our virtual IOPs across Florida are often covered by UHC when medically necessary.
Virtual programs must meet the same clinical standards as in-person care, offering individual and group therapy via video. This parity in coverage means your benefits should apply equally whether you attend in-person or virtually. The key requirement is that your provider must be licensed in the state where you are located during treatment. Virtual IOPs offer undeniable convenience, allowing you to get intensive support without disrupting your life.
Are There Limits on IOP Treatment Duration with UHC?
UHC does not set a universal limit on IOP duration; instead, coverage is based on medical necessity. Your provider will conduct regular concurrent reviews with UHC/Optum, submitting clinical updates to show you still require and benefit from intensive care. This means continued coverage depends on your documented progress.
There is no fixed number of weeks or sessions covered. As you improve, your care team will work with UHC on step-down care planning to transition you to a less intensive option, like weekly therapy. Research shows that consistent attendance in an IOP leads to better outcomes, which helps justify continued coverage.
How to Find IOP Providers That Work With the United Health Company for Mental Health Services
Finding an IOP that accepts your insurance can be tough. Fortunately, UnitedHealthcare provides several reliable ways to find IOP providers that work with the united health company for mental health services in Florida.
- UHC Provider Directory: Log into the MyUHC portal at myuhc.com to search for behavioral health providers in your plan’s network.
- Optum’s Live and Work Well Portal: Since Optum manages UHC’s behavioral health benefits, their portal, LiveandWorkWell.com (access code: “united”), is an excellent resource for finding providers.
- Psychology Today Filters: Websites like Psychology Today let you filter searches by location (e.g., Tampa, FL; Orlando, FL) and by insurance, specifically selecting UnitedHealthcare.
- Call the Number on Your ID Card: This is the most direct method. A UHC representative can verify your benefits and provide a list of in-network IOPs in your area. Contact United Healthcare directly for plan inquiries.
- Ask a Potential Provider to Verify for You: Many IOPs, including Thrive Mental Health, offer free insurance verification. We contact UHC on your behalf to confirm your benefits and explain any costs, taking the burden off you.

How to Verify Your Specific UHC Insurance Coverage for IOP
Before starting an IOP, it’s critical to verify your exact UHC benefits. Follow this step-by-step guide:
- Gather Your Information: Have your UHC insurance card ready with your Member ID, Group Number, and the behavioral health phone number.
- Call UHC Member Services: Call the behavioral health number and state you’re seeking coverage for a mental health IOP.
- Key Questions to Ask: To ensure you get all the necessary details, ask these specific questions:
- “Does my plan cover Intensive Outpatient Programs (IOPs) for mental health?”
- “Is prior authorization required for IOP services?”
- “What are my in-network and out-of-network benefits for IOPs?”
- “What is my deductible, and how much of it have I met?”
- “What are my copays or coinsurance percentages for in-network IOP services?”
- “Is there an out-of-pocket maximum for my plan?”
- “Are there any limits on the number of sessions or duration of IOP treatment?”
- “Does my plan cover virtual (telehealth) IOPs?”
- “Can you provide a list of in-network IOP providers that work with the united health company for mental health services in my area (e.g., Orlando, FL; Miami, FL; Jacksonville, FL)?”
- Use the MyUHC Portal: Log into your MyUHC account to find details on your deductible, copays, and in-network providers.
- Take Notes: Note the date, representative’s name, and a reference number for your call. This is useful if issues arise later.
Verifying your benefits is a crucial step toward accessing care without unexpected financial burdens.
What to Expect from In-Network IOP Providers That Work With the United Health Company for Mental Health Services
Choosing an in-network IOP provider that works with UnitedHealthcare offers clear advantages:
- Lower Costs: In-network providers have negotiated rates with UHC, which means your deductible, copays, and coinsurance will be significantly lower.
- Direct Billing: The provider bills UHC directly, so you only handle your copay or coinsurance. No administrative headaches.
- Pre-Vetted Providers: In-network IOPs are credentialed by UHC/Optum, ensuring they meet quality and licensing standards for effective care.
- Easier Authorization Process: In-network providers know UHC’s authorization process, which streamlines your path to starting treatment.
- Reduced Financial Surprises: Your costs are more predictable, making it easier to budget for treatment without worrying about unexpected bills.
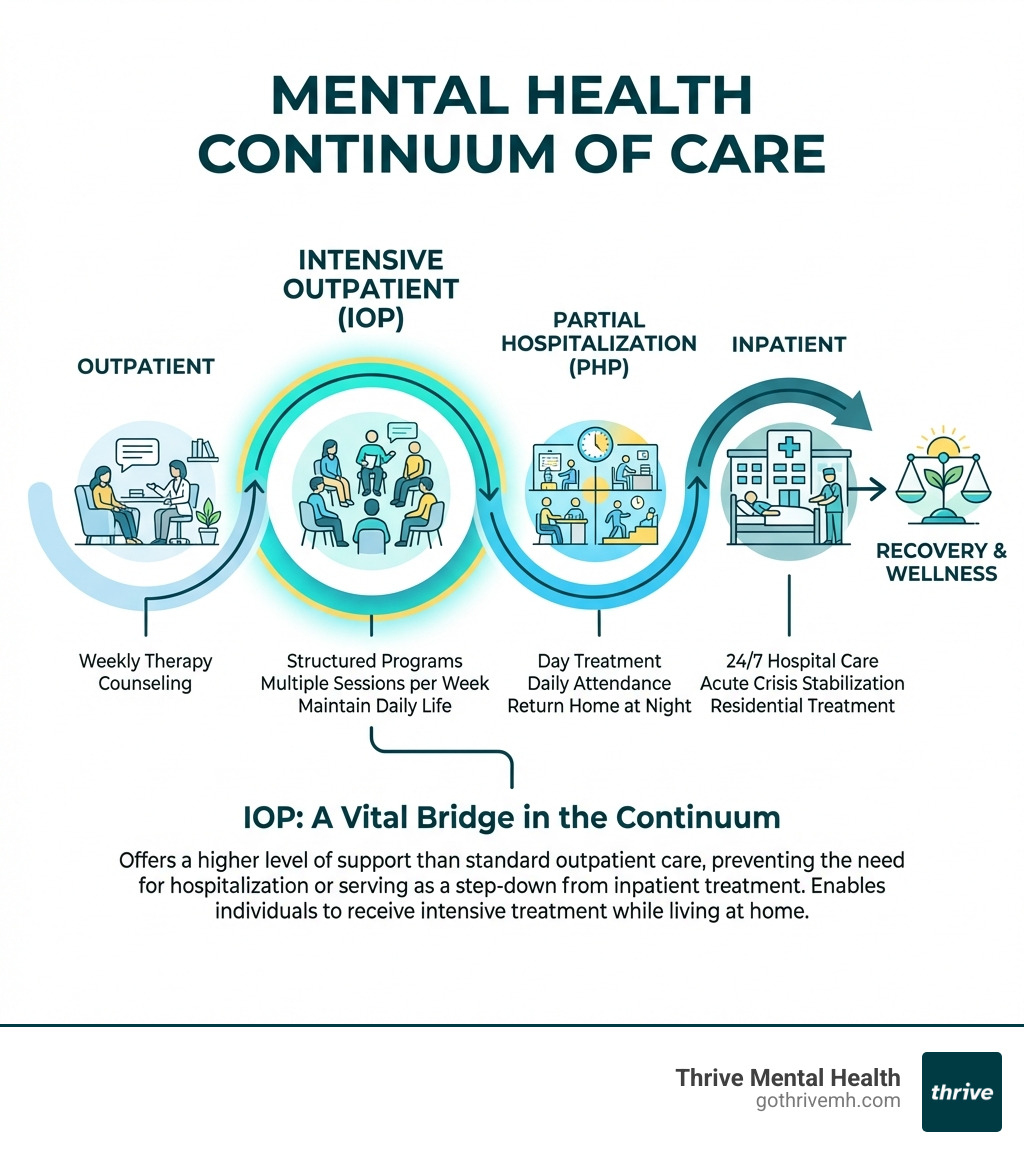
IOP vs. Other Care Levels: How UHC Views Your Treatment Path
Understanding the mental health continuum of care helps you see where an IOP fits and how UHC views your treatment. This spectrum of services matches you with the right intensity of care for your needs.
- Inpatient Hospitalization: The highest level of care, providing 24/7 monitoring in a hospital for acute mental health crises.
- Partial Hospitalization Program (PHP): A step down from inpatient. It involves structured, all-day therapy sessions several days a week, but you return home at night.
- Intensive Outpatient Programs (IOPs): The middle ground. IOPs offer more support than weekly therapy (e.g., 3-hour sessions, 3-5 days a week) but allow you to live at home and maintain daily responsibilities.
- Traditional Outpatient Therapy: The least intensive level, consisting of weekly or bi-weekly therapy sessions for managing stable conditions or as step-down care.
When UHC Recommends IOP Over Inpatient or PHP
UHC recommends an IOP based on medical necessity when you meet these criteria:
- No Need for 24/7 Supervision: You are not an immediate danger to yourself or others and don’t require constant monitoring.
- Stable Living Environment: You have a safe and supportive home to return to after treatment.
- Need for More Than Weekly Therapy: Standard therapy isn’t enough to manage your symptoms, but you don’t require a full-day PHP.
- Transitioning from Higher Care: You are stepping down from an inpatient or PHP program and need continued support to prevent relapse.
- Moderate-to-Severe Symptoms: You have symptoms of depression, anxiety, or PTSD that benefit from a structured, multi-modal therapeutic approach.
The decision for an IOP is made in consultation with a mental health professional who assesses your clinical needs and determines the most appropriate level of care, which UHC then reviews for medical necessity.
The Fine Print: Navigating UHC Claims, Denials, and Documentation
Navigating insurance claims can be frustrating, but understanding the process helps. Your in-network IOP provider that works with the united health company for mental health services will handle most of it. They submit claims to UHC/Optum with the correct diagnosis (ICD-10) and procedure (CPT) codes within the required timeframe (usually 90 days).
After a claim is processed, you’ll get an Explanation of Benefits (EOB). This isn’t a bill; it’s a statement showing what was covered, what UHC paid, and what you owe. Always review your EOBs.
Common reasons for a claim denial include:
- Lack of prior authorization.
- Services deemed not medically necessary.
- Using an out-of-network provider.
- Claims filed past the deadline.
- Incorrect or incomplete information.
What Documentation Is Needed to Process UHC Claims?
Proper documentation is key for claim approval. Both you and your provider have a role.
Provider’s Role: Your IOP provides UHC with:
- Clinical assessments and diagnosis codes (ICD-10)
- Treatment plans and procedure codes (CPT)
- Progress notes to prove medical necessity for ongoing reviews
Patient’s Role: Your main job is to give your provider accurate insurance information (Member ID, Group Number) and sign any necessary consent forms for billing and authorization.
How to Appeal a UHC Denial for IOP Services
A denial from UHC isn’t the final word. You have the right to appeal the decision. Here’s an overview of the process:
- Understand the Denial: Review your denial letter to see the exact reason. This is key to your appeal.
- Request an Internal Review: You or your provider can file a written appeal with UHC, submitting supporting documents like letters of medical necessity and progress notes to strengthen your case.
- Request an Expedited Appeal: If waiting poses a risk to your health, you can request an urgent appeal for a faster decision.
- File for an External Review: If the internal appeal fails, you can have your case reviewed by an independent third party whose decision is binding.
- Gather Documentation: Collect all relevant records from your IOP, including your treatment plan, progress notes, and assessments.
- Get Provider Help: Your IOP provider, like Thrive Mental Health, can be a huge asset. We can provide clinical documentation and guide you through the appeals process.
You are not alone in this process. Advocating for your care is your right, and resources are available to help you steer it.
Frequently Asked Questions about UHC and IOP
Does United Healthcare require a referral for an IOP?
Most UHC plans, managed through Optum, do not require a primary care physician referral for behavioral health services like IOP. However, the IOP provider will almost always need to obtain prior authorization from UHC/Optum before starting treatment to ensure it’s covered.
How do I know if an IOP is “medically necessary” for my UHC plan?
Medical necessity is determined by UHC/Optum based on clinical information provided by your IOP. Generally, it means you have a diagnosed mental health condition that significantly impairs your daily functioning, and your needs can’t be met with less intensive care (like weekly therapy), but you don’t require 24/7 inpatient supervision.
Can I use my United Healthcare plan for an IOP in a different state?
Coverage depends on your specific plan (HMO, PPO, etc.). PPO plans typically offer more flexibility with out-of-state providers, but it’s crucial to confirm whether the provider is in-network with your plan. Virtual IOPs can often serve you as long as the provider is licensed in the state where you are physically located during treatment, such as our virtual programs accessible to residents throughout Florida.
Ready for Support That Fits Your Life?
Finding the right level of care is a critical step toward feeling better. Intensive Outpatient Programs offer a powerful middle ground, providing robust support while you maintain your daily life. With United Healthcare, this level of care is often more accessible and affordable than you might think, especially when you choose an in-network provider. By understanding your benefits and how to steer the system, you can open up the expert treatment you deserve.
Ready for support? Thrive offers virtual and hybrid IOP/PHP programs with evening options. Verify your insurance in 2 minutes (no obligation) or call 561-203-6085. If you’re in crisis, call/text 988.