Understanding Psychiatric Intensive Outpatient Programs

More Than Weekly Therapy, Less Than a Hospital Stay
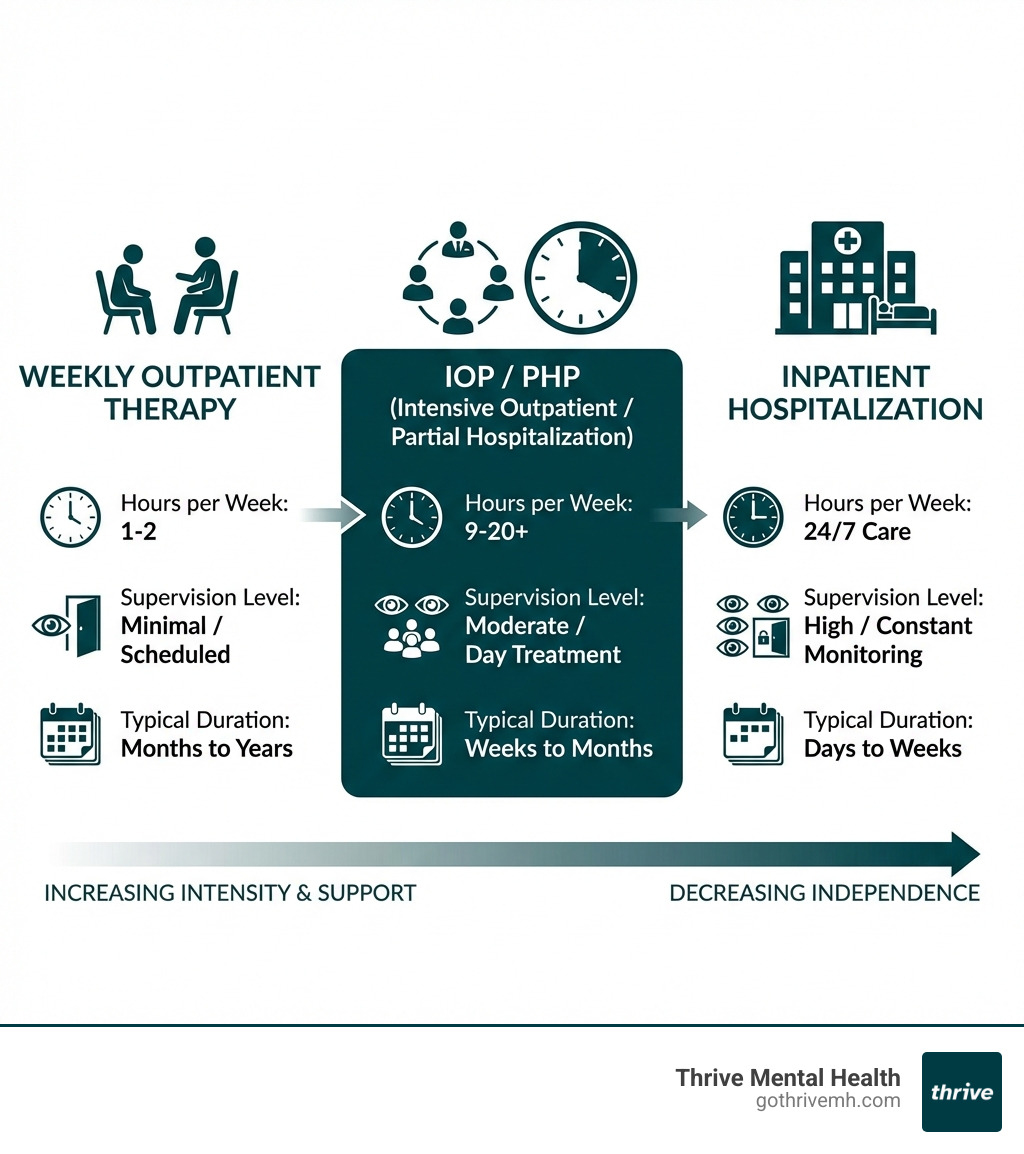
What is a psychiatric intensive outpatient program? It’s a structured mental health treatment that bridges the gap between traditional once-a-week therapy and full hospitalization. IOPs deliver 9-15 hours of evidence-based care per week—enough to create real change, but flexible enough to fit around work, school, or family responsibilities.
Quick Answer:
- Structure: 9-15 hours per week of treatment, typically 3-5 days
- Setting: Outpatient care (you go home each day, no overnight stay)
- Format: Combines group therapy, individual counseling, and family sessions
- Purpose: Step-up from weekly therapy or step-down from inpatient care
- Who it’s for: People needing intensive support but medically stable enough to live at home
If you’ve been in therapy for months without enough progress, or you’re stepping down from a higher level of care, an IOP might be exactly what you need. It’s designed for people who are functional enough to maintain daily life but struggling enough that once-weekly sessions aren’t cutting it.
The reality is that mental health care isn’t one-size-fits-all. Some people need a hospital. Others do fine with weekly therapy. But there’s a huge group in the middle—high-functioning professionals, college students, parents—who need more without losing their jobs or dropping out of life. That’s where IOPs come in.
I’m Nate Raine, CEO of Thrive Mental Health, and I’ve spent over a decade building innovative behavioral health programs that integrate clinical excellence with real-world flexibility. Understanding what is a psychiatric intensive outpatient program—and how to scale access to it—has been central to our mission of changing care for working adults and young professionals, with a strong focus on our communities here in Florida.
What is a psychiatric intensive outpatient program word roundup:
- how long are intensive outpatient programs
- mental health intensive outpatient program requirements
- outpatient psychiatric treatment
What is a Psychiatric Intensive Outpatient Program (IOP)? [And Is It Right For You?]
When we talk about what is a psychiatric intensive outpatient program, we’re referring to a flexible yet highly structured form of mental health treatment. Imagine needing more support than a weekly therapy session, but not requiring 24/7 supervision or an overnight stay in a facility. That’s precisely the sweet spot an IOP fills.
An IOP, also known as intensive outpatient treatment (IOT), is a non-residential program where individuals attend therapy sessions for several hours a day, multiple days a week. Unlike inpatient care, you return home each day, allowing you to maintain your daily responsibilities like work, school, or family commitments. This balance of intensive care and real-world application is a cornerstone of our approach at Thrive Mental Health.
Our IOPs typically involve 9 to 15 hours of structured treatment per week, spread across three to five days. This intensive schedule allows for deep therapeutic work, skill-building, and peer support, all while you continue to live your life. It’s a powerful step for individuals seeking to stabilize symptoms, develop coping strategies, and build a strong foundation for long-term recovery.
We’ve seen how effective this model can be, especially for adults and young professionals who are juggling careers, education, and family. It’s about getting the help you need without putting your life completely on pause.
Want to dive deeper into how our programs are structured to fit your life? Learn More info about our IOP services.

Conditions IOPs Effectively Treat
Psychiatric IOPs are incredibly versatile, designed to treat a wide array of mental health and co-occurring conditions. Our programs at Thrive Mental Health are built to address complex needs with compassionate, evidence-based care.
We commonly treat individuals struggling with:
- Depression: From persistent low mood to major depressive disorder, IOPs provide the structured support and therapeutic tools needed to steer and overcome depressive episodes.
- Anxiety Disorders: Including generalized anxiety disorder, social anxiety, panic disorder, and specific phobias. We help individuals develop coping mechanisms to manage overwhelming anxiety.
- Substance Use Disorders (SUD): IOPs are a highly effective treatment for SUDs, particularly for individuals who do not require detoxification but need intensive support to achieve and maintain sobriety. A 2015 literature review found that IOPs significantly reduce alcohol and drug use and improve mental health among people struggling with SUD. For many, IOP programs are often as effective as inpatient treatment for alcohol or drug use disorders, according to a meta-analysis from 2014. If you’re looking for Scientific research on IOP effectiveness for SUDs, this study offers valuable insights.
- Trauma and PTSD: For those struggling with the lingering effects of trauma, IOPs offer a safe and supportive environment to process experiences and develop healthy coping strategies.
- Eating Disorders: While some severe eating disorders may require inpatient care, IOPs can be crucial for individuals needing structured support for disordered eating patterns and body image issues.
- Bipolar Disorder: Managing the highs and lows of bipolar disorder requires consistent support. IOPs help individuals stabilize mood, adhere to medication plans, and develop self-management skills.
- Co-occurring Disorders: It’s common for mental health conditions to exist alongside substance use disorders. Our integrated approach allows us to treat both simultaneously, providing comprehensive care for complex needs.
Our programs are custom to the individual, recognizing that each person’s journey is unique. We focus on helping you develop effective coping strategies, improve communication skills, and address the root causes of your challenges.
Who is a Good Candidate for IOP?
Deciding if an IOP is the right fit is a crucial step. We look for individuals who need a significant level of support, but who are also able to manage their daily lives outside of structured treatment hours.
You might be a good candidate for a psychiatric IOP if you:
- Need more than weekly therapy: You’ve found that traditional outpatient therapy isn’t providing enough support or progress, and your symptoms are significantly impacting your daily functioning.
- Are medically stable: You do not require 24/7 medical supervision or immediate detoxification. Your physical health allows you to participate actively in an outpatient setting.
- Are not an immediate danger to yourself or others: This is a critical criterion. IOPs are designed for individuals who are safe to be in their home environment between sessions.
If you’re in crisis, call/text 988 right now. You are not alone.
The National Suicide Prevention Lifeline is available 24/7.
- Are motivated for change: You’re ready to engage actively in your treatment and commit to the program’s structure and therapeutic process.
- Have a supportive home environment: While not always a strict requirement, a stable and supportive living situation can greatly improve your success in an IOP.
- Are an adult or young professional: Our programs are specifically designed for adults aged 18 and older, including young professionals navigating the complexities of career and life.
- Are transitioning from inpatient or PHP: An IOP serves as an excellent “step-down” option, providing continued intensive support as you reintegrate into daily life after a higher level of care.
We conduct thorough initial assessments to ensure our IOP is the most appropriate level of care for your unique needs. Our goal is to set you up for success, providing the right support at the right time.
IOP vs. PHP vs. Outpatient: How to Choose the Right Level of Care
Understanding the spectrum of mental health care can feel like navigating a maze. At Thrive Mental Health, we offer various levels of care to ensure you get precisely what you need, when you need it. Let’s break down the differences between traditional outpatient therapy, Intensive Outpatient Programs (IOPs), and Partial Hospitalization Programs (PHPs).
This continuum allows for a “step-up” approach if symptoms worsen and more support is needed, or a “step-down” approach as you progress in your recovery and require less intensive care.
| Feature | Traditional Outpatient Therapy | Intensive Outpatient Program (IOP) | Partial Hospitalization Program (PHP) |
|---|---|---|---|
| Hours per Week | 1-2 hours | 9-15 hours (adults); 6-9 hours (adolescents) | 20+ hours |
| Session Frequency | 1-2 times per week | 3-5 days per week | 5-7 days per week |
| Structure Level | Low | Moderate to High | High |
| Supervision | Minimal | Moderate clinical oversight | High clinical and medical oversight |
| Ideal Candidate | Mild to moderate symptoms, stable, good coping skills | Moderate to severe symptoms, stable, needs structured support, maintains daily life | Severe symptoms, needs significant structure & supervision, alternative to inpatient, stepping down from inpatient |
| Setting | Clinic or virtual | Clinic or virtual | Clinic or virtual |
| Cost | Lowest | Moderate | Highest (among outpatient options) |
For a comprehensive look at the next level of care, explore More info about Partial Hospitalization Programs (PHP).
What is a psychiatric intensive outpatient program compared to a PHP?
The primary distinction between an IOP and a PHP lies in the intensity and time commitment.
- Partial Hospitalization Program (PHP): This is the most intensive form of outpatient treatment we offer. PHPs are often considered a full-day program, typically requiring 20 or more hours of treatment per week, usually 5 to 7 days a week, for several hours each day. It’s a robust alternative to inpatient hospitalization for those who need significant structure and supervision but don’t require 24/7 medical care. Patients attend during the day and return home at night.
- Intensive Outpatient Program (IOP): As we’ve discussed, an IOP is a half-day program, generally involving 9 to 15 hours of treatment per week, 3 to 5 days a week. It’s a step down from a PHP but still provides far more support than traditional outpatient therapy.
The choice between a PHP and an IOP often comes down to your symptom severity and the level of functional impairment you’re experiencing. If you’re transitioning from inpatient care or need a very high level of daily structure to manage acute symptoms, a PHP might be recommended. If your symptoms are stable enough to allow for more independence but still require robust support, an IOP is likely the better fit.
Many individuals will transition from a PHP to an IOP as their symptoms improve and they gain more skills, gradually stepping down their level of care while maintaining consistent support.
When is Traditional Outpatient Therapy Not Enough?
We all hope that weekly therapy sessions will be enough to tackle our mental health challenges, and for many, it is. But there are clear signs when it’s time to consider a more intensive approach like an IOP:
- Stalled Progress: You’ve been in weekly therapy for a while, but you feel stuck. You’re not seeing significant improvements, or you’re repeatedly addressing the same issues without resolution.
- Worsening Symptoms: Despite therapy, your symptoms are intensifying, becoming more frequent, or starting to interfere more significantly with your daily life, relationships, or work/school performance.
- Needing More Structure: You find it difficult to implement coping skills outside of your therapy session, or you struggle with accountability without more frequent check-ins and structured activities.
- Lacking a Support System: You may not have a strong support network at home or in your community, and you need the consistent peer and professional support that an IOP provides. Group therapy, a cornerstone of IOPs, offers invaluable peer support and a sense of community.
- Requiring Integrated Services: You need a more comprehensive approach that includes not just individual therapy, but also group therapy, family involvement, and potentially psychiatric evaluation and medication management, all coordinated under one roof.
If you’re nodding along to any of these, it’s a strong indicator that you might benefit from the added structure and comprehensive care of a psychiatric intensive outpatient program.
A Day in the Life: What Really Happens in an IOP?
So, what does a typical week look like in a psychiatric intensive outpatient program? While schedules can vary, our IOPs at Thrive Mental Health are designed with flexibility and comprehensive care in mind.
A common IOP schedule might involve attending sessions for 3-4 hours a day, 3-5 days a week. For example, some programs run Monday, Wednesday, and Thursday, with an optional Friday session. This allows for dedicated therapy time while leaving ample space for personal responsibilities.
The duration of an IOP is usually between 4 to 6 weeks, though this can be adjusted based on individual progress and clinical needs. The goal isn’t just to complete the program, but to stabilize symptoms, build robust coping skills, and prepare you for sustainable recovery.
One of the greatest benefits of our programs is the flexibility they offer. Many of our clients throughout Florida find success with our virtual IOP options, allowing them to receive expert-led care from the comfort of their home, fitting seamlessly into their busy lives.

Curious about how virtual treatment can work for you? Explore More info about virtual IOP.
Core Services and Therapeutic Modalities
At the heart of what is a psychiatric intensive outpatient program are its core services, designed to provide a holistic and multi-faceted approach to healing. Our programs integrate various therapeutic modalities to address your unique needs:
- Group Therapy: This is often the primary component of an IOP, offering a powerful environment for peer support, shared experiences, and learning. Group sessions provide a sense of community and validation, helping you realize you’re not alone.
- Individual Counseling: You’ll have dedicated one-on-one sessions with a therapist to address personal goals, process individual challenges, and tailor strategies to your specific situation.
- Family Involvement: We believe in the power of support systems. Family therapy sessions are often included to improve communication, strengthen relationships, and educate loved ones on how to best support your recovery journey.
- Medication Management: For many, medication is a critical component of mental health stability. Our programs may include psychiatric evaluations and ongoing medication management with qualified professionals to ensure optimal symptom control.
- Psychiatric Evaluation: A psychiatrist or psychiatrist extender will conduct an evaluation to assess your needs and guide treatment planning, especially regarding medication.
Common IOP group topics we cover include:
- CBT (Cognitive Behavioral Therapy) skills for challenging negative thought patterns.
- DBT (Dialectical Behavior Therapy) for emotion regulation, distress tolerance, and interpersonal effectiveness.
- Relapse prevention strategies, especially crucial for those with substance use disorders.
- Mindfulness and meditation practices to increase presence and reduce stress.
- Healthy relationships and communication skills.
- Coping with grief and loss.
- Stress management techniques.
- Building self-esteem and confidence.
- Exploring trauma and its impact.
What is a psychiatric intensive outpatient program’s approach to therapy?
Our approach to therapy within a psychiatric IOP is rooted in evidence-based practices, meaning we use therapeutic techniques that have been scientifically proven to be effective. We don’t just talk about change; we equip you with the tools to make it happen.
Key therapeutic approaches you’ll encounter include:
- Cognitive Behavioral Therapy (CBT): This therapy helps you identify and change unhelpful thinking patterns and behaviors that contribute to your mental health challenges. It’s about learning to reframe your thoughts and react differently to situations.
- Dialectical Behavior Therapy (DBT): Particularly effective for emotion regulation and interpersonal difficulties, DBT teaches skills in mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness.
- Acceptance and Commitment Therapy (ACT): ACT helps you accept difficult thoughts and feelings, commit to actions that align with your values, and live a more meaningful life, even in the presence of discomfort.
- Motivational Interviewing: This client-centered approach helps you explore and resolve ambivalence about change, strengthening your motivation to pursue recovery goals.
Beyond these core modalities, we focus on building coping skills that are practical and applicable to your everyday life. This includes learning how to manage stress, steer difficult emotions, communicate effectively, set healthy boundaries, and build a fulfilling life in recovery. Our aim is to empower you with the resilience and strategies you need to thrive long after you complete the program.
Your IOP Roadmap: Finding a Program, Using Insurance, and Planning for Success
Starting on an IOP journey is a significant step towards healing, and we’re here to guide you through it. From finding the right program to understanding insurance coverage and planning for life after treatment, we ensure you have a clear roadmap to success.
How to Find and Choose the Right IOP
Finding the right psychiatric IOP can feel like a big task, but we’ve made it simple. Here’s how to steer your options:
- Seek Referrals: Start by talking to your current doctor, therapist, or psychiatrist. They can provide personal recommendations based on your needs and their knowledge of reputable programs.
- Online Search: Use online directories and treatment locators. The The SAMHSA National Helpline and Treatment Locator is an excellent resource for finding programs in your area.
- Ask Key Questions: When you contact potential providers, be prepared with questions like:
- What is the program’s philosophy and treatment approach?
- What conditions do you specialize in treating?
- What does a typical daily/weekly schedule look like?
- What therapeutic modalities do you use (CBT, DBT, etc.)?
- What are the qualifications of your clinical staff?
- What is the typical duration of the program?
- Do you offer in-person or virtual IOP options? (At Thrive, we offer both in-person and virtual IOP options to serve clients throughout Florida).
- How do you handle aftercare planning?
- What are your admission requirements?
- Do you accept my insurance?
Choosing a program that aligns with your specific needs and preferences is crucial for a successful outcome. Whether you prefer the structure of an in-person center or the convenience of a virtual program, we have options designed to support your journey.
Are IOPs Covered by Insurance?
“Will my insurance cover this?” It’s one of the most common and important questions we hear. The good news is that psychiatric IOPs are often covered by major insurance plans, but understand the specifics.
Insurance coverage for IOPs is typically contingent on medical necessity criteria. This means that a clinical assessment must determine that an IOP is the appropriate and necessary level of care for your condition. Criteria often include:
- A diagnosable mental health condition.
- Significant functional impairment impacting daily life.
- A need for structured, intensive therapy that cannot be met by traditional outpatient care.
- Medical stability, meaning you don’t require 24/7 inpatient supervision.
At Thrive Mental Health, we work with many major insurance providers to serve our clients in Florida, including Florida Blue, Cigna, and Optum, among others. We understand that navigating insurance can be complex, which is why we offer a simple way to verify your benefits.
We encourage you to use our quick and easy tool to Check your insurance coverage now – it takes just a couple of minutes and there’s no obligation. We’re committed to making evidence-based treatment accessible, and understanding your insurance benefits is a key part of that.
Life After IOP: Aftercare and Sustaining Recovery
Completing a psychiatric IOP is a huge accomplishment, but it’s not the end of the journey. In fact, it’s a powerful new beginning. A critical component of any effective IOP is comprehensive aftercare planning, designed to help you sustain your recovery and continue thriving.
Our approach at Thrive Mental Health focuses on preparing you for life after IOP by:
- Discharge Planning: This begins early in your program. We work with you to create a personalized plan for your transition, which may include stepping down to a lower level of care, such as weekly individual therapy or support groups.
- Transitioning to a Lower Level of Care: This might involve connecting you with individual therapists, psychiatrists, or specialized outpatient programs in your Florida community to ensure continuous support.
- Building a Support System: We help you identify and strengthen your personal support network, including family, friends, and peer support groups. The sense of community fostered in IOPs is invaluable, and we encourage maintaining those connections.
- Alumni Programs: Many programs offer alumni networks, providing ongoing connection and support from others who have completed treatment.
- Relapse Prevention Strategies: You’ll leave the IOP equipped with a robust set of skills to recognize triggers, manage cravings or difficult emotions, and implement healthy coping mechanisms to prevent relapse.
We believe in a “wraparound care” approach, ensuring you have continuous support as you steer life post-IOP. This proactive planning helps you integrate the skills you’ve learned and maintain long-term wellness. Learn More info about wraparound care.
Frequently Asked Questions about Psychiatric IOPs
How long does an IOP program typically last?
Most IOPs last between 4 to 6 weeks, but the duration is custom to individual progress and clinical needs. The goal is to stabilize symptoms and build skills, not to adhere to a rigid timeline. Your treatment plan will be regularly reviewed and adjusted to ensure you’re getting the most effective care for as long as you need it.
Can I keep my job or go to school while in an IOP?
Yes. This is a primary benefit of IOPs. Programs are structured to provide intensive care while allowing you to maintain your daily responsibilities, with many offering morning, afternoon, or evening sessions to fit your schedule. This flexibility is particularly valuable for working adults and young professionals.
Are virtual IOPs as effective as in-person programs?
Research shows that for many individuals, virtual IOPs are just as effective as in-person treatment. They offer the same evidence-based therapies and expert-led groups, with the added benefits of convenience and accessibility from home. This allows us to make high-quality care accessible to individuals all across Florida, from the Panhandle to the Keys, regardless of their physical location.
Ready for Support That Fits Your Life?
A psychiatric intensive outpatient program offers a powerful, flexible middle ground for those who need serious support without putting their life on hold. It provides the structure, skills, and community to manage symptoms and build a foundation for lasting recovery.
Ready for support? Thrive offers virtual and hybrid IOP/PHP programs with evening options for Florida residents. Verify your insurance in 2 minutes (no obligation) → Start benefits check or call 561-203-6085. If you’re in crisis, call/text 988.