Obsessed with Answers: Understanding What Causes OCD
What Causes OCD? The 4 Core Factors You Need to Understand
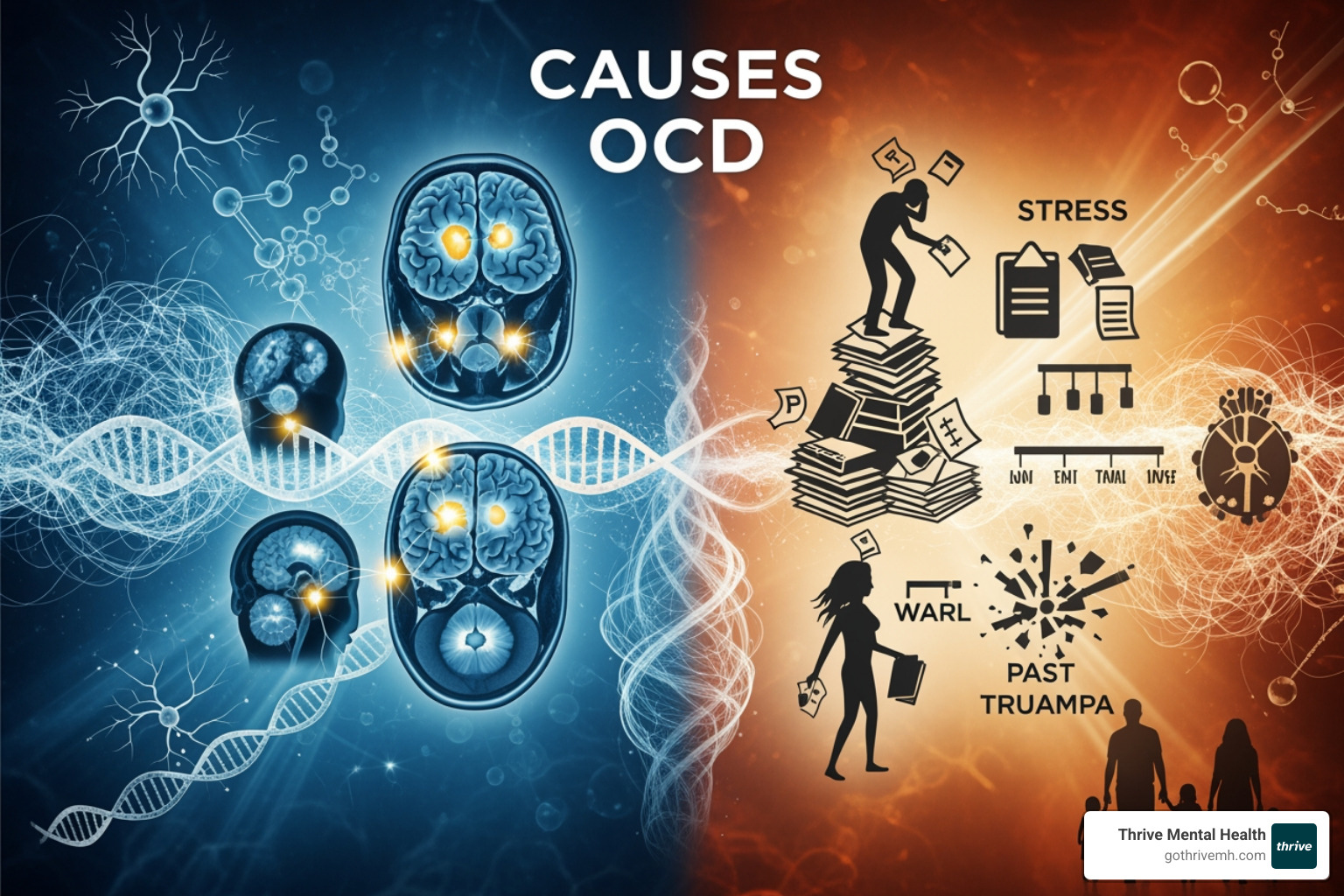
You’re asking “what causes OCD?” because you want a clear answer and a path to relief. The search for a single “smoking gun” is frustrating, but understanding the real causes is the first step toward taking back control. OCD isn’t a character flaw or a sign of weakness; it’s a treatable medical condition rooted in a complex mix of biology, genetics, environment, and psychology.
Quick Answer: The Four Main Contributors to OCD
| Factor | What It Means |
|---|---|
| Biological | Brain circuit dysfunction (CSTC loop) and neurotransmitter imbalances (serotonin, glutamate, dopamine) |
| Genetic | Heritability of ~48%; 4x higher risk if a family member has OCD |
| Environmental | Stress, trauma, infections (PANDAS/PANS), and major life changes can trigger onset |
| Psychological | Learned thought patterns, misinterpretation of intrusive thoughts, and inflated sense of responsibility |
The bottom line? OCD isn’t caused by weakness, bad parenting, or a character flaw. It’s a treatable medical condition with roots in how your brain is wired, how your genes express themselves, and how you’ve learned to respond to anxiety.
Here’s what matters most: you don’t need to pinpoint the exact cause to get better. Evidence-based treatment—especially Exposure and Response Prevention (ERP) therapy—works regardless of what triggered your OCD in the first place.
I’m Nate Raine, CEO of Thrive Mental Health, and I’ve spent over a decade at the intersection of mental health innovation and data-driven care. At Thrive, with our specialized OCD treatment centers in Florida, we treat hundreds of clients with OCD using evidence-based programs designed around what causes OCD at the neurological and behavioral levels—so you can move from understanding to real recovery.

To get a clearer picture of OCD, explore these key topics:
The OCD Brain: Biological & Genetic Roots of the Disorder
When we talk about what causes OCD, we often start with the brain itself. Research shows that individuals with OCD exhibit distinct differences in brain structure and activity compared to those without the disorder. It’s not about a “broken” brain, but rather a brain that processes information and regulates emotions in a unique way.
One of the most consistently implicated areas is the Cortico-Striato-Thalamo-Cortical (CSTC) loop, often dubbed the brain’s “worry circuit.” This circuit involves several key regions:
- Orbitofrontal Cortex (OFC): Involved in decision-making and assessing risk. In OCD, it may be overactive, leading to an exaggerated sense of danger or incompleteness.
- Anterior Cingulate Cortex (ACC): Plays a role in error detection and conflict monitoring. An overactive ACC might contribute to the persistent feeling that something is “wrong.”
- Basal Ganglia: Crucial for habit formation and motor control. Hyperactivity here could explain the repetitive, ritualistic nature of compulsions.
- Thalamus: A relay station for sensory and motor signals.
In OCD, this CSTC loop is thought to be dysregulated, particularly with a hyperactive direct pathway relative to the indirect pathway. This imbalance can create a cycle where intrusive thoughts (obsessions) get “stuck,” and the brain struggles to disengage from them, leading to the urge to perform compulsions to find temporary relief. While brain imaging studies reveal these differences, it’s a classic “chicken or egg” dilemma: do these brain differences cause OCD, or are they a consequence of living with the disorder? The answer likely lies in a complex interplay.
What Causes OCD in the Brain’s Chemistry?
Beyond structure, brain chemistry also plays a significant role in what causes OCD. Neurotransmitters—the chemical messengers of the brain—are heavily involved.
Serotonin Hypothesis: More Complex Than We Thought
For a long time, a popular theory was that OCD was simply caused by a “chemical imbalance,” specifically a deficit in serotonin. This idea gained traction because Selective Serotonin Reuptake Inhibitors (SSRIs), which increase serotonin levels in the brain, are often effective in treating OCD symptoms. However, we now understand this is an oversimplification. While serotonin pathways are undeniably involved, the “chemical imbalance” theory alone doesn’t fully explain the disorder. The brain’s chemistry is far more intricate, and serotonin may be more involved in maintaining OCD symptoms rather than being their sole cause.
Emerging Players: Glutamate and Dopamine
Recent research points to other neurotransmitters as crucial contributors. The glutamate system is gaining attention as an emerging factor in OCD onset and progression. Glutamate is the brain’s primary excitatory neurotransmitter, and imbalances in its function can impact learning, memory, and anxiety circuits. Similarly, dopamine pathways, which are associated with reward, motivation, and habit formation, are also implicated. Dysregulation in dopamine could contribute to the difficulty individuals with OCD have in stopping compulsive behaviors, even when they know these actions are irrational.
The bottom line is that the neurobiological underpinnings of OCD are complex, involving multiple brain regions and neurotransmitter systems working in concert. It’s not just one chemical out of whack, but rather a nuanced symphony of brain activity that goes awry. Understanding this complexity is crucial as we develop more targeted and effective treatments. For those curious about the solutions, you can find More about OCD treatment on our site.
Is OCD Genetic? Unpacking the Role of Heredity
The question of what causes OCD often leads to our family trees. Is OCD something you inherit? The answer is a resounding “sometimes.” Genetics play a significant, though not exclusive, role.
The Numbers Don’t Lie: Heritability and Family Risk
Research consistently shows a familial component to OCD. The heritability quotient for OCD is estimated to be approximately 48%. This means that nearly half of the risk for developing OCD can be attributed to genetic factors. Interestingly, this estimate reduces to 35% when maternal effects (like prenatal exposure to stress or infection) are considered, highlighting the early influence of environment.
If a close family member has OCD, your risk of developing the disorder is significantly higher. Studies indicate that a person with OCD is 4 times more likely to have another family member with OCD than someone without the disorder. Specifically, between 10% to 20% of children who have a parent with OCD will develop the condition themselves. However, this also means 80% to 90% will not, even with a genetic predisposition.
Twin Studies: Nature vs. Nurture
Twin studies have been instrumental in understanding the genetic contribution. Research on twins suggests that genetics have a stronger role than environmental factors in the expression and development of OCD. Even in identical twins, where one develops OCD, the other doesn’t always, indicating that genes alone are not the sole determinant. This points to a gene-environment interaction, where genetic predispositions might be “activated” by certain life experiences or stressors.
Genetic Predisposition vs. Destiny
So, while OCD isn’t a simple inherited disease like eye color, genetic factors undoubtedly create a predisposition. This doesn’t mean you’re destined to develop OCD if a family member has it, but it does mean your brain might be wired in a way that makes you more susceptible. It’s a complex interplay where your genetic blueprint interacts with the world around you. For a deeper dive into the genetic landscape, you can explore A meta-analysis on the genetic epidemiology of OCD.
How Life Events and Learned Behaviors Can Trigger OCD
Your brain’s wiring is only part of the story. The “nurture” side of the equation—your life experiences, environment, and learned responses—plays a critical role in what causes OCD to surface and take hold.

Imagine a brain predisposed to OCD—a car with a sensitive alarm system. Environmental factors are the unexpected bumps in the road, the sudden loud noises that set off that alarm. These external influences don’t necessarily cause the alarm system to exist, but they can certainly activate it.
The Cognitive-Behavioral Model: How We Learn OCD
Psychological theories offer powerful insights into how OCD symptoms take hold and persist. The cognitive-behavioral model suggests that OCD is not just a brain malfunction but also a learned pattern of thinking and behaving. It often starts with:
- Misinterpreting Intrusive Thoughts: Everyone has intrusive thoughts—random, unwanted mental images or urges. For most, these pass quickly. But for someone predisposed to OCD, these thoughts might be interpreted as personally meaningful, dangerous, or a sign of a character flaw.
- Thought-Action Fusion: This is the belief that merely thinking about an action is morally equivalent to performing it, or that thinking about a negative event increases its likelihood.
- Inflated Sense of Responsibility: Individuals with OCD often feel an exaggerated sense of responsibility to prevent harm, even for things outside their control. This leads to anxiety and the urge to perform compulsions to “neutralize” the thought or prevent the feared outcome.
This creates a vicious cycle: obsession leads to anxiety, which leads to compulsions for temporary relief, which then reinforces the belief that the compulsion was necessary. Breaking this cycle is precisely what evidence-based therapies like Exposure and Response Prevention (ERP) aim to do. To better understand this internal struggle, we encourage you to read about Understanding Intrusive Thoughts in OCD.
What Causes OCD to Emerge After Stress or Trauma?
While stress and trauma aren’t direct causes of OCD, they can act as powerful catalysts, particularly in individuals with a genetic or biological predisposition. We often see OCD symptoms emerge or worsen during periods of significant life upheaval.
Stressful Life Events as Triggers
Major life changes, even positive ones, can disrupt our routines and increase stress, potentially triggering OCD symptoms. Events like:
- Starting a new job or moving to a new city.
- The birth of a baby (leading to perinatal or postpartum OCD, which affects a high incidence of women).
- A divorce or relationship breakup.
- Major academic or career pressure.
Everyday stress can also exacerbate existing symptoms. When our bodies and minds are under pressure, the brain’s “worry circuit” can become even more sensitive, making it harder to dismiss intrusive thoughts and resist compulsions.
Childhood Trauma and Adverse Experiences
Adverse childhood experiences, such as trauma, neglect, or abuse, have also been identified as risk factors that can influence the development or onset of OCD. While the exact mechanisms are still being researched, it’s understood that such experiences can alter brain development and stress response systems, increasing vulnerability to mental health conditions like OCD.
The Infection Connection: PANDAS/PANS
A fascinating and distinct area of research connects certain infections to the sudden onset of OCD in children. This phenomenon is known as:
- PANDAS (Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal infections): In a subgroup of children, a strep throat infection can trigger an autoimmune response. The body’s antibodies, intended to fight the strep bacteria, mistakenly attack parts of the brain, particularly the basal ganglia, leading to a sudden, dramatic onset or worsening of OCD symptoms and tics.
- PANS (Pediatric Acute-onset Neuropsychiatric Syndrome): This is a broader category, where similar sudden-onset OCD and neuropsychiatric symptoms occur after other types of infections (e.g., Lyme disease, influenza) or even non-infectious inflammatory reactions.
Children with PANDAS/PANS often develop symptoms seemingly overnight, with a very severe impact on their life. This differs significantly from other forms of childhood OCD that typically have a more gradual onset. Research continues to explore these connections, with studies like this one on PANDAS and brain activity providing crucial insights into how infections might play a role in what causes OCD in some cases.
It’s Not Your Fault: Debunking Common Myths About OCD
After exploring the complex causes of OCD, one thing must be crystal clear: it is not your fault. Harmful myths and misconceptions create shame and prevent people from seeking help. It’s time to debunk them.
For instance, OCD often begins in the teen or young adult years, but it can start in childhood. Boys frequently develop OCD at a younger age than girls. However, by adulthood, women are about 1.6 times as likely as men to be affected by OCD overall, though specific subtypes like Symmetry OCD might be more prevalent in men. These differences hint at varying developmental and hormonal influences that intersect with other causal factors.
[5] Destructive Myths About What Causes OCD: And Why They’re Wrong
It’s crucial to debunk common misconceptions about OCD, not only for understanding but for fostering empathy and encouraging individuals to seek help.
- “It’s just bad parenting.” This is a harmful and entirely unfounded myth. OCD is a medical condition with complex roots, not a result of how someone was raised. While family dynamics can influence how symptoms are expressed or managed, they do not cause the disorder itself.
- “It’s a sign of weakness or a character flaw.” Absolutely not. OCD has nothing to do with a person’s strength of character, willpower, or moral fiber. It’s a disorder that affects anyone, regardless of their personal attributes.
- “You can just ‘snap out of it.'” If only it were that simple. OCD involves deeply ingrained brain pathways and learned patterns that cannot be overcome by sheer will. Telling someone with OCD to “just stop” is like telling someone with a broken leg to “just walk it off.”
- “OCD is all about being neat and organized.” While some people with OCD have obsessions around order and symmetry, this is just one subtype. Many others struggle with contamination fears, intrusive thoughts of harm, religious scrupulosity, or other distressing themes that have nothing to do with tidiness. Differentiating OCD from perfectionism is key; perfectionism is a personality trait, while OCD is a debilitating disorder driven by anxiety.
- “OCD is a choice.” No one chooses to have distressing, intrusive thoughts or to spend hours performing rituals that interfere with their life. The compulsions provide temporary relief from intense anxiety, not pleasure, and individuals often feel trapped by their symptoms.
Understanding these complexities and dispelling myths is the first step towards recovery. The most empowering truth is this: you don’t need to pinpoint the exact cause of your OCD to find effective treatment. Whether it’s genetic, biological, environmental, or psychological, the path to managing symptoms and reclaiming your life is clear. If you’re wondering Do I have OCD?, getting an accurate diagnosis is the critical next step.
Frequently Asked Questions About What Causes OCD
Is OCD purely genetic?
No, it’s a complex mix of genetic predisposition and environmental factors. Heritability is estimated to be around 48%, meaning genes play a significant but not exclusive role. Environmental factors, like stress or trauma, can interact with these genetic vulnerabilities.
Can a stressful event cause OCD?
A stressful or traumatic event can act as a trigger for OCD in individuals who are already predisposed, but it is not considered a sole cause. Stress tends to exacerbate existing symptoms or precipitate their onset in those who are vulnerable.
Is OCD caused by a simple chemical imbalance?
This is an outdated and oversimplified view. While neurotransmitters like serotonin and glutamate are involved, OCD is better understood as a disorder of brain circuitry and communication, not just a lack of one chemical. The brain’s functioning is far more intricate than a simple imbalance.
Does OCD get worse with age?
OCD symptoms can fluctuate throughout life, often worsening during periods of high stress or major life transitions. However, with effective, evidence-based treatment, symptoms can be managed and significantly reduced at any age. It’s not an inevitable progression to worse symptoms.
From Understanding to Action: You Can Manage OCD [Even Without a Single Answer]
We’ve dug into the complex web of what causes OCD, from brain chemistry to life events. The most important takeaway isn’t finding a single answer—it’s knowing that a clear, proven path to recovery exists regardless of the cause.
But here’s the powerful truth: the exact origin of your OCD doesn’t dictate your future. The path to recovery is clear, proven, and accessible. At Thrive Mental Health, we specialize in evidence-based treatments that address the symptoms and underlying mechanisms of OCD, regardless of its initial cause.
Our gold standard treatment is Exposure and Response Prevention (ERP) therapy, a highly effective form of cognitive-behavioral therapy that helps you confront your fears without resorting to compulsions, gradually rewiring your brain’s responses. We combine this with other therapeutic modalities and, where appropriate, medication management, to provide comprehensive, individualized care.
We understand that seeking help can be a challenge, which is why Thrive Mental Health offers specialized virtual and hybrid Intensive Outpatient Programs (IOP) and Partial Hospitalization Programs (PHP) designed for adults and young professionals. Our programs combine clinical expertise, flexible scheduling, and measurable results, offering more support than weekly therapy but less than inpatient care.
With in-person centers across Florida and comprehensive virtual programs, we make evidence-based treatment accessible to residents throughout the state. Our services are also available to individuals in California, Indiana, Arizona, and South Carolina. We work with major insurance providers like Cigna, Optum, and Florida Blue, to help make treatment affordable. Learn about our OCD treatment programs in Florida and take the first step towards reclaiming your life from OCD.
Ready for support? Thrive offers virtual and hybrid IOP/PHP programs with evening options. Verify your insurance in 2 minutes (no obligation) → Start your benefits check for Exposure and Response Prevention Therapy or call 561-203-6085. If you’re in crisis, call/text 988.