EMDR Unveiled: What to Expect When You’re Expecting Healing

What is EMDR Like: Unveiled for Healing 2025
What It Really Feels Like to Do EMDR—And Why It Works
What is EMDR like? It’s awake, alert, and surprisingly not as intense as you might fear. You’re not hypnotized. You’re not forced to relive every detail of your trauma. Instead, you focus briefly on a difficult memory while your therapist guides your eyes back and forth—or uses tapping or sounds—to help your brain reprocess what’s stuck. Most people describe it as feeling calm, controlled, and even a little strange at first, but effective.
Quick Answer: What Happens During EMDR
- You stay in control: You’re awake, aware, and can stop anytime
- Brief focus on trauma: You identify the memory without retelling the whole story
- Bilateral stimulation: Eye movements, tapping, or sounds help your brain reprocess
- Phases, not chaos: 8 structured phases guide you from history-taking to closure
- Sessions are 60-90 minutes: Single-event trauma may improve in 3-6 sessions; complex trauma takes longer
- Results can be rapid: Studies show 84-90% of single-trauma survivors no longer meet PTSD criteria after just three 90-minute sessions
EMDR (Eye Movement Desensitization and Reprocessing) is a psychotherapy designed to reduce the emotional charge of traumatic memories. It works by activating your brain’s natural healing process—similar to how REM sleep helps you process the day—while you’re awake and guided by a trained therapist.
Unlike traditional talk therapy, EMDR doesn’t require you to narrate every painful detail. Instead, you focus on the memory while engaging in bilateral stimulation (usually eye movements, but also tapping or tones). This helps your brain “digest” the experience and store it with less emotional intensity.
I’m Anna Green, LMHC, LPC, Chief Clinical Officer and founder of Thrive Mental Health, and I’ve been trained in EMDR for over a decade, using it to help clients with complex trauma, PTSD, and anxiety disorders. I’ve seen what EMDR is like for people who thought they’d never feel safe in their own minds again—and watched them reclaim their lives in weeks, not years.
Relevant articles related to what is emdr like:
How EMDR Works: Reprogramming Your Brain’s Response to Trauma
Your brain is wired to heal itself. When you cut your finger, your body knows exactly what to do—it clots, scabs, and rebuilds. Trauma should work the same way. But sometimes, it doesn’t.
That’s where EMDR comes in.
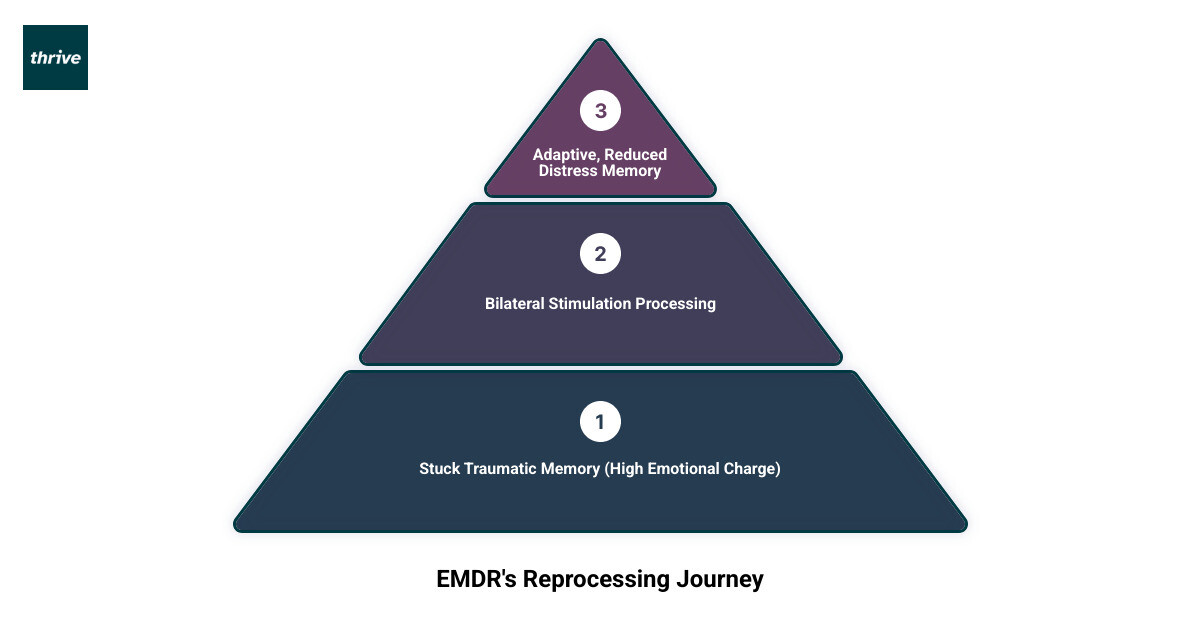
What is EMDR like when it comes to how it actually works? It’s based on something called the Adaptive Information Processing (AIP) model, which is just a fancy way of saying your brain has a natural filing system. When something distressing happens, your brain tries to process it, make sense of it, and store it away with the rest of your memories.
But traumatic experiences can get stuck. They don’t get filed properly. Instead, they stay raw, unprocessed, and emotionally charged—like a wound that never closes. That’s why you might have flashbacks, nightmares, or sudden waves of panic years after something happened. Your brain is still treating the memory like it’s happening right now.
EMDR helps your brain finish the job. It removes the block and jump-starts your brain’s natural healing process. The goal isn’t to erase the memory—it’s to help your brain store it in a way that doesn’t overwhelm you anymore. Instead of feeling like it’s still happening, it becomes something that happened. Past tense. Done.
The tool that makes this possible is called bilateral stimulation (BLS). This is the part that feels a little unusual at first, but it’s also what makes EMDR so effective.
Bilateral stimulation is rhythmic, left-right stimulation of your brain. It can happen through eye movements (following your therapist’s finger or a light bar), hand-tapping (alternating taps on your knees or hands), or auditory tones (sounds that alternate between your left and right ear through headphones).
Why does this work? Researchers believe it mimics what your brain does during REM sleep—the phase where your brain naturally sorts through the day, processes emotions, and consolidates memories. By engaging BLS while you focus on a distressing memory, EMDR helps your brain make new connections and integrate the memory into a healthier, more adaptive network.
The result? The emotional charge drops. Negative beliefs about yourself start to shift. Physical tension releases. You stop feeling like you’re reliving the trauma and start feeling like you’re remembering it—calmly, without the panic.
Here’s what’s important to understand: EMDR is about reprocessing, not reliving. You’re not being asked to describe every painful detail or immerse yourself in the worst moments. Your therapist acts as a guide, helping you steer the experience safely. You stay grounded. You stay in control. The goal is to digest the experience, let go of the unhelpful emotions and beliefs, and keep what’s useful—like the lessons learned or the strength you gained.
This approach is backed by serious research. The World Health Organization (WHO) endorses EMDR as one of the recommended treatments for PTSD in both adults and children. It’s not experimental. It’s evidence-based, structured, and proven to work.
If you want to dive deeper into the specific techniques used in EMDR, check out our article on Exploring EMDR Therapy Techniques for Trauma Recovery. It walks through the tools and methods therapists use to help you reprocess trauma safely and effectively.
What is an EMDR Session Like? A Phase-by-Phase Breakdown
If you’re curious about what is EMDR like when you’re actually sitting in the room (or on a video call), here’s the truth: it’s structured, collaborative, and surprisingly calm. You’re not thrown into the deep end. You’re not forced to white-knuckle your way through a traumatic memory alone. Instead, you and your therapist move through a clear, eight-phase process designed to keep you safe, grounded, and in control every step of the way.

EMDR therapy follows an eight-phase treatment protocol that takes you from history-taking all the way through to lasting resolution. Think of it like building a house: you need a solid foundation before you can put up the walls. Your therapist acts as your guide throughout, but you remain in the driver’s seat. You decide what to share, when to pause, and how fast to go.
Phases 1 & 2: Building Your Foundation (History & Preparation)
The first two phases are all about laying the groundwork. This is where trust is built, plans are made, and you’re equipped with the tools you’ll need to feel safe throughout the process.
Phase 1 is history-taking. Your therapist will spend time getting to know you—your background, your current struggles, and what brought you to therapy. You’ll identify specific “target memories” to work on. These might be traumatic events from your past, present-day triggers that set you off, or even future situations you’re anxious about. This isn’t about recounting every painful detail; it’s about mapping out where the work needs to happen. Your therapist is also listening for your strengths and resilience, the parts of you that have kept you going.
Phase 2 is preparation, and it’s crucial. Before you ever touch a difficult memory, your therapist will teach you coping skills and grounding techniques to help you manage any distress that comes up. You’ll learn things like the safe/calm place exercise, where you create a mental sanctuary you can retreat to when things feel overwhelming. You might practice the butterfly hug (a self-soothing technique involving gentle taps on your chest), coherent breathing, or mindfulness exercises.
These aren’t just nice-to-haves—they’re essential. They help you stay within your window of tolerance, that sweet spot where you can process difficult emotions without getting flooded or shutting down completely. At Thrive Mental Health, we never rush this phase. We believe that effective EMDR is built on thorough preparation. If you’re wondering how to find a therapist who takes this approach seriously, our article on Choosing the Right EMDR Therapist: Tips and Considerations walks you through what to look for.
Phases 3-6: The Core Processing Work (Assessment to Body Scan)
Once you’re prepared and feel secure, you move into the heart of the work. This is where the actual reprocessing happens, and it’s where what EMDR is like becomes most tangible.
Phase 3 is assessment. You and your therapist will zero in on a specific target memory. For that memory, you’ll identify the most vivid visual image that represents it, a negative belief you hold about yourself because of it (like “I’m not safe” or “I’m powerless”), and a positive belief you’d rather hold instead (like “I’m safe now” or “I have control”). You’ll also notice what emotions and physical sensations come up when you think about the memory and the negative belief.
Then comes the rating. You’ll rate how disturbing the memory feels right now using the Subjective Units of Disturbance (SUD) scale, where 0 means no disturbance at all and 10 is the worst you can imagine. You’ll also rate how true your positive belief feels using the Validity of Cognition (VOC) scale, where 1 is completely false and 7 is completely true. These numbers give you and your therapist a baseline to track your progress.
Phase 4 is desensitization, and this is where bilateral stimulation comes in. While you hold the target memory, the negative belief, and the physical sensations in mind, your therapist will guide you through sets of eye movements (or tapping, or tones—whatever form of bilateral stimulation works for you). Each set lasts about 20 to 30 seconds. After each set, your therapist will ask, “What are you noticing?” and you’ll briefly share whatever thoughts, feelings, images, or sensations came up—no judgment, no analysis, just noticing.
This process repeats, and often what happens is surprising. The memory might shift. New insights might emerge. The emotional charge starts to drain away. You keep going until your SUD level drops significantly—ideally to a 0 or 1—and the memory no longer feels overwhelming.
Phase 5 is installation. Once the distress is reduced, your therapist helps you strengthen that positive belief. While you hold the positive belief in mind alongside the original memory, you’ll do more sets of bilateral stimulation. The goal is to get your VOC rating up to a 6 or 7, so the new belief feels genuinely true. You’re not just saying “I’m safe now”—you’re feeling it in your body and your brain.
Phase 6 is the body scan. Your therapist will guide you through a mental check-in from head to toe, looking for any lingering tension or discomfort related to the memory. If anything pops up—a tightness in your chest, a knot in your stomach—you’ll do more bilateral stimulation to process it until your body feels clear and calm.
Phases 7 & 8: Closing the Loop (Closure & Re-evaluation)
The final two phases ensure you don’t leave a session feeling raw or unfinished, and that your progress sticks.
Phase 7 is closure. Even if a memory isn’t fully processed by the end of the session, your therapist will guide you back to a calm, grounded state. You might use your safe place visualization or another resourcing technique. You’ll also be given a heads-up about what to expect between sessions—sometimes your brain keeps processing on its own, and you might notice vivid dreams, new insights, or shifting emotions. Your therapist may ask you to keep a journal of anything that comes up so you can discuss it next time.
Phase 8 is re-evaluation. At the start of each new session, your therapist will check in on the memories you’ve already worked on. How’s your SUD level now? Is the positive belief still holding strong? This ensures the changes are lasting and gives you both a chance to address any new material that surfaced between sessions. Over time, you’ll work through past memories, present triggers, and future scenarios, creating a comprehensive path to healing.
Understanding what EMDR is like phase by phase can take some of the mystery—and the fear—out of the process. It’s not chaotic. It’s not unpredictable. It’s a clear, compassionate roadmap designed to help your brain do what it does best: heal.
The Full Experience: Before Your First Session and After It Ends
Understanding what is EMDR like isn’t just about what happens in the therapy room. It’s also about those first nervous sessions when you’re not quite sure what to expect, and the days afterward when your brain keeps working on healing—sometimes in surprising ways.
What to Expect in Your First Few Sessions
Here’s something that might ease your mind: your first few EMDR sessions won’t involve diving straight into trauma processing. I’ve had countless clients arrive at their first appointment braced for an immediate emotional deep-dive, only to find that we spend those early sessions simply talking, building trust, and learning tools together.
Your therapist’s first priority is creating a foundation of safety. You’ll spend time getting to know each other, discussing your history without needing to relive painful details, and clarifying what you hope to achieve through therapy. Think of it as laying the groundwork before building the house—you need a solid base before you can do the deeper work.
A significant part of these initial sessions focuses on teaching you coping skills and grounding techniques. Remember those resourcing tools from Phase 2—the safe place visualization, the butterfly hug, coherent breathing? You’ll practice these until they feel natural, like having a well-stocked emotional first-aid kit. These aren’t just nice-to-have extras; they’re essential tools that keep you within your window of tolerance when processing begins.
The pace is entirely yours. If you’ve had therapy experiences where you felt rushed or pushed beyond your comfort zone, EMDR takes a different approach. You won’t move forward until you feel genuinely prepared and confident. Your therapist is there to guide, not to push. If you need more time in the preparation phase, that’s perfectly okay—and actually, it’s smart therapy.
What is EMDR like after the session is over?
Here’s where things get interesting. When your session ends and you walk out the door, your brain doesn’t clock out. It keeps processing, integrating, and reorganizing the material you worked on. This integration period between sessions is actually part of the therapy itself.
Many clients notice more vivid dreams or shifts in their sleep patterns. Your brain is doing its nighttime filing work, similar to how EMDR mimics REM sleep during sessions. Don’t be surprised if you dream about seemingly random things—that’s often your brain making new connections and sorting through old material.
You might also experience sudden insights or new perspectives on old situations. A memory you haven’t thought about in years might surface, or you might suddenly understand a pattern in your relationships that never made sense before. Some clients describe it as puzzle pieces finally clicking into place.
Emotional shifts are common too. You might feel waves of sadness, anger, relief, or even a strange sense of emptiness where intense feelings used to live. These shifts are temporary and actually indicate that the therapy is working—the emotional charge attached to memories is dissipating. It’s like removing a heavy backpack you didn’t realize you’d been carrying.
Occasionally, you might notice a temporary increase in sensitivity or distress. This usually feels mild and passes quickly, but it’s your brain actively reprocessing material. The coping skills you learned in those early sessions become crucial here. Use them. Practice your safe place visualization, try the butterfly hug, or reach out to supportive people in your life.
Self-care becomes more important than ever during EMDR treatment. Your nervous system is doing hard work, so support it with the basics: gentle movement, nutritious food, adequate sleep, and connection with people who make you feel safe. Think of it as giving your brain the fuel it needs to heal.
If you find yourself feeling overwhelmed between sessions, don’t wait—reach out to your therapist. They can help you use your resources more effectively or adjust the pace of treatment.
If you’re in crisis, call/text 988 right now. You are not alone.
While EMDR is considered safe when delivered by a trained professional, it’s worth understanding the full picture. Our article on the Dangers of EMDR Therapy provides insights into potential challenges and how to ensure your therapeutic experience remains safe and effective.
Is EMDR Right for You? Key Differences & Conditions Treated
Deciding on the right therapeutic path can feel like a big decision. Understanding what is EMDR like in comparison to other therapies and what conditions it effectively treats can help you make an informed choice.
What is EMDR like compared to traditional talk therapy?
If you’ve tried traditional talk therapy before, you might be wondering how EMDR is different. The contrast is significant, and for many people, it’s exactly what makes EMDR work when other approaches haven’t.
In traditional talk therapy, you typically spend a lot of time talking through your experiences, examining your thoughts, and building a narrative around what happened. The therapist helps you understand patterns, challenge negative beliefs, and develop new coping strategies. It’s cognitive and verbal—you’re working through problems by talking about them, sometimes for months or years.
What is EMDR like by comparison? It’s much less about talking and much more about internal processing. You don’t need to provide lengthy narratives or explain every detail of what happened. Instead, you briefly identify the memory while your therapist guides you through bilateral stimulation. Your brain does the heavy lifting, making new connections and processing the stuck material while you simply notice what comes up.
The focus in EMDR is on your body’s sensations, emotions, and the images that arise—not on constructing a coherent story for your therapist. Many clients find this incredibly relieving, especially if talking about trauma feels too overwhelming or retraumatizing. You might spend an entire session processing a memory without ever fully describing what happened.
| Feature | EMDR Therapy | Traditional Talk Therapy |
|---|---|---|
| Primary Focus | Internal processing of emotions, sensations, and beliefs linked to memories. Less emphasis on verbal narrative. | Cognitive restructuring and behavioral changes through discussion and insight. |
| Session Structure | Structured 8-phase protocol with bilateral stimulation during processing phases. | Varies widely; often conversational and client-led. |
| Verbal Detail Required | Minimal. You identify the memory without extensive storytelling. | Extensive. You often need to explain and explore experiences in detail. |
| Homework | Journaling observations, practicing resourcing skills, self-care. | Often includes thought records, behavioral experiments, or skill practice. |
Another key difference is the speed of results. EMDR often works faster than traditional talk therapy, particularly for single-incident trauma. While talk therapy might take months to years to process a traumatic event, EMDR can sometimes resolve it in just a few sessions. For a deeper comparison of different therapy approaches, our article on CBT vs DBT vs EMDR breaks down how these modalities differ and which might be right for your specific situation.
Conditions EMDR Can Help With
EMDR was originally developed for Post-Traumatic Stress Disorder (PTSD), and it remains one of the most effective treatments for trauma-related conditions. Studies consistently show that 84-90% of single-trauma survivors no longer meet PTSD criteria after just three 90-minute sessions. That’s remarkable.
But EMDR’s applications extend far beyond PTSD. Because it targets the way distressing memories are stored and processed, it can help with a wide range of conditions where past experiences contribute to current symptoms.
Anxiety and panic attacks often respond well to EMDR, especially when they’re rooted in specific triggering events or memories. If your anxiety stems from past experiences—a humiliating moment, a frightening incident, or accumulated stress—EMDR can help reprocess those memories and reduce their emotional charge.
Depression that’s connected to unresolved grief, trauma, or negative beliefs about yourself (“I’m worthless,” “I’m a failure”) can also benefit from EMDR. By targeting the experiences that created these beliefs, EMDR helps shift your internal narrative.
Phobias—whether it’s fear of flying, driving, medical procedures, or social situations—often have a root memory that EMDR can address. Processing the original distressing experience can dramatically reduce or eliminate the phobic response.
Complicated grief is another area where EMDR shows powerful results. If you’re stuck in your grief, unable to move forward, or experiencing intrusive images or thoughts about a loss, EMDR can help you process the pain while preserving the love and positive memories. Our article on EMDR Therapy for Grief explores this application in depth.
Even performance anxiety—whether related to public speaking, sports, or professional situations—can be addressed with EMDR. By processing memories of past failures or embarrassing moments and installing positive beliefs about your capabilities, EMDR helps you approach performance situations with confidence rather than dread.
Practical Considerations: Insurance and Location
One of the most common questions we hear is, “Will my insurance cover EMDR?” The good news is that most major insurance plans do cover EMDR therapy when it’s provided as part of mental health treatment. At Thrive Mental Health, we work with many major insurance providers, including Cigna, Optum, and Florida Blue, among others.
EMDR is typically billed under psychotherapy codes, so if your plan covers therapy sessions, it will likely cover EMDR. The key is finding a provider who’s in-network with your insurance and properly trained in EMDR. Coverage details vary by plan, so we recommend verifying your specific benefits before starting treatment.
Thrive Mental Health serves clients in Indiana and California, offering both virtual and in-person options through our intensive outpatient (IOP) and partial hospitalization (PHP) programs. Our virtual therapy options mean you can access expert EMDR treatment from the comfort of your home, which is especially helpful if you’re dealing with anxiety about leaving your house or if you live in an area with limited mental health resources.
We also offer evening sessions, making it easier to fit treatment into your work and life schedule. You don’t have to choose between your job and your healing.
Ready to find out if EMDR is right for you? You can verify your insurance in 2 minutes with no obligation, or call us at 561-203-6085 to speak with someone who can answer your questions.