Everything You Need to Know About Stress Vomiting

What is Stress Vomiting? Your #1 Guide to Relief
When Your Stomach Reacts to Stress: Understanding a Common Physical Response
If you or someone you know is in crisis or experiencing suicidal thoughts, please call or text the 988 Suicide & Crisis Lifeline at 988. Help is available 24/7, and you are not alone.
What is stress vomiting? It’s when your body responds to extreme stress or anxiety by triggering nausea and vomiting—not because you’re physically sick, but because your brain and gut are deeply connected. This isn’t motion sickness or food poisoning. It’s your body’s fight-or-flight response affecting your digestive system.
Quick Answer:
- What it is: Vomiting triggered by emotional or psychological stress
- Why it happens: Stress hormones (cortisol, adrenaline) disrupt normal digestion
- Key sign: Occurs during high-stress situations without other illness symptoms
- Common with: Anxiety disorders, panic attacks, and major life stressors
- Risk increase: Anxiety disorders raise nausea risk by more than 3x
Have you ever felt so anxious before a big presentation that your stomach turned? Or been so stressed about an upcoming event that you felt physically sick? You’re not imagining it. Your gut and brain communicate constantly through what scientists call the gut-brain axis—and when stress floods your system, your stomach often pays the price.
The physical toll of stress goes far beyond worry and racing thoughts. When your body perceives a threat (real or imagined), it activates your fight-or-flight response. Blood flow diverts away from digestion. Stomach acid increases. Your gut becomes hypersensitive. For some people, this cascade ends in nausea or vomiting.
Research shows this connection is both common and significant. Studies indicate that anxiety disorders increase the risk of nausea by more than three times, and stress vomiting may be even more prevalent in people with severe anxiety disorders.
I’m Anna Green, LMHC, LPC, Chief Clinical Officer at Thrive Mental Health. Throughout my career treating complex anxiety presentations and leading evidence-based programs, I’ve helped countless clients understand what is stress vomiting and develop effective strategies to address both the symptom and its root cause.
What is Stress Vomiting? The Science Behind the Gut-Brain Reaction
What is stress vomiting? At its core, it’s your body’s physical response to emotional overwhelm—a fascinating and sometimes frustrating example of how deeply our minds and bodies are connected. It’s not a disease or illness in itself. Rather, it’s a symptom that shows up when stress or anxiety becomes so intense that your digestive system simply can’t function normally.
Think of it this way: your brain and gut are constantly texting each other. When everything’s calm, they’re sharing friendly updates. But when stress hits? Your brain sends urgent alerts that can completely disrupt your stomach’s ability to do its job.
How the Fight-or-Flight Response Triggers Nausea
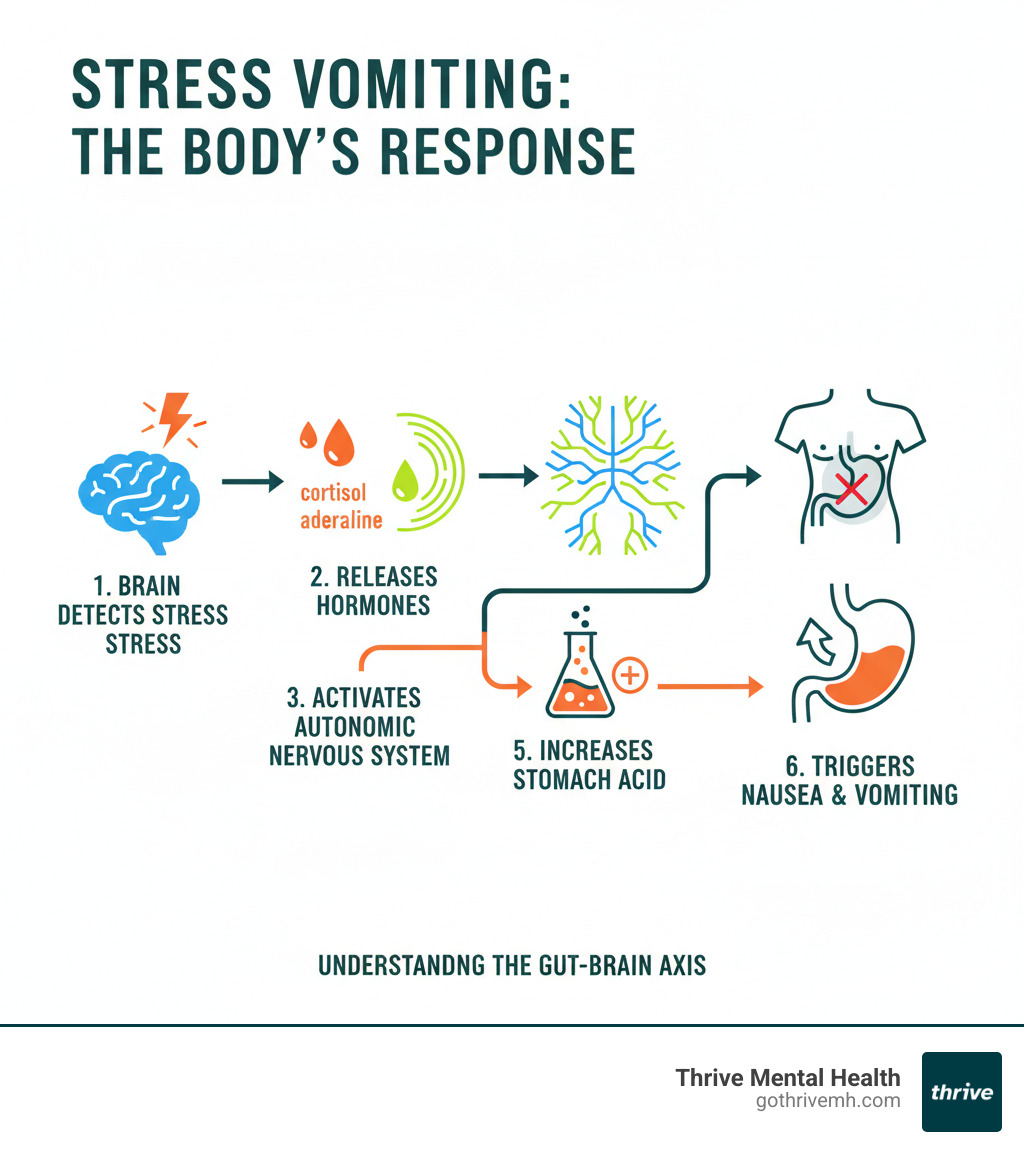
The story of stress vomiting begins with your body’s ancient survival system—the fight-or-flight response. When your brain perceives a threat (whether it’s a bear in the woods or an upcoming job interview), it immediately floods your system with stress hormones, primarily cortisol and adrenaline. These hormones are designed to help you survive danger.
Here’s where things get uncomfortable for your stomach. Your autonomic nervous system kicks into high gear, and your body makes a split-second decision: survival comes first, digestion comes later. As Cleveland Clinic research explains, when we’re under stress, our body releases a flood of hormones to prepare us to face or flee from a perceived threat.
This survival mode creates a perfect storm for nausea. Blood flow diverts away from your digestive system to your heart, lungs, and muscles—the organs you’d need to fight or run. Meanwhile, your stomach produces more acid, which can irritate the lining and trigger that queasy feeling. Your digestive tract may experience erratic contractions or spasms, and suddenly everything just feels… wrong.
Muscle tension in the abdomen adds to the discomfort, creating physical pressure that can activate the vomiting reflex mechanism. Your gut also becomes hypersensitive during stress, meaning sensations that wouldn’t normally bother you suddenly feel overwhelming. What might normally be mild fullness now registers as intense nausea.
Understanding the Gut-Brain Axis and Its Role in What is Stress Vomiting
The connection between stress and your stomach runs along something scientists call the gut-brain axis—a sophisticated two-way communication highway linking your central nervous system to your digestive system. This isn’t just a metaphor. There’s actual physical wiring connecting your emotional state to your gut function.
The star of this show is the vagus nerve, which acts like a fiber-optic cable sending signals back and forth between your brain and gut at lightning speed. When anxiety strikes, your brain sends urgent messages down this nerve that directly influence how your stomach behaves. This brain-gut communication happens constantly, whether you’re aware of it or not.
This is why emotions affect the stomach so powerfully. When you’re nervous, worried, or panicked, those feelings don’t just stay in your head—they travel directly to your digestive system. Your gut becomes more reactive, more sensitive, more prone to upset. Even the balance of bacteria in your digestive tract can shift during chronic stress, further impacting both your physical comfort and your mood.
Heightened gut sensitivity means your stomach overreacts to normal digestive processes. A little gas? Feels like major cramping. Slight fullness? Registers as severe nausea. It’s as if the volume has been turned way up on every sensation. For more information about how anxiety shows up in your daily life beyond digestive symptoms, you can explore our guide on anxiety symptoms and their impact on daily life.
What is Stress Vomiting vs. Other Digestive Issues?
Figuring out whether you’re dealing with stress vomiting or something else is important for getting the right help. While the physical act of vomiting looks the same, the cause—and therefore the treatment—is quite different.
The clearest sign of stress vomiting is the lack of other illness symptoms. You won’t have a fever. You’re not achy all over. You don’t have that general “I’m coming down with something” feeling that comes with a virus or food poisoning. You might feel awful, but it’s a different kind of awful—more anxious than sick.
Timing is everything when differentiating from food poisoning or motion sickness. Stress vomiting tends to happen right before, during, or shortly after a stressful situation. The connection is usually pretty obvious once you start paying attention. Before the big presentation? Nauseous. During the difficult conversation? Stomach churning. After the anxiety-provoking event ends? Often, the symptoms start to ease.
You’ll also notice there’s no contamination or infection involved. You didn’t eat questionable leftovers. You’re not in a moving vehicle. There’s no bug going around the office. The trigger is purely emotional or psychological.
Finally, stress vomiting typically shows up alongside other anxiety symptoms—racing heart, shortness of breath, trembling, sweating, or overwhelming worry. These accompanying signs point to stress as the culprit rather than a physical illness.
Understanding that what is stress vomiting is fundamentally different from other digestive problems is the first step toward addressing it effectively. Once you recognize the emotional root cause, you can start working on solutions that actually help.
Symptoms and Conditions Linked to Stress Vomiting
When you’re trying to understand what is stress vomiting, it helps to recognize that the actual vomiting is rarely an isolated symptom. Your body typically sends multiple warning signals that your stress response has kicked into overdrive.

The physical signs often start subtle and build. You might first notice nausea—that queasy, unsettled feeling in your stomach that makes you wonder if you’re about to get sick. This is frequently accompanied by abdominal pain or cramping, sometimes described as a tight knot or band around your middle. Many people also experience dizziness or lightheadedness, which can result from your body’s stress response redirecting blood flow or from mild dehydration if you’ve already vomited.
Your appetite often disappears completely during periods of high stress. This loss of appetite is your body’s way of shutting down non-essential functions when it thinks you’re facing a threat. You might also notice changes in your bowel habits—stress can cause either diarrhea or constipation, sometimes alternating between the two.
Beyond digestive symptoms, you’ll likely experience the classic signs of anxiety: rapid heartbeat, shortness of breath, trembling hands, sweating, muscle tension throughout your body, and overwhelming feelings of worry or panic. These symptoms cluster together because they’re all part of the same stress response system.
The connection between anxiety and digestive distress is backed by solid research. Studies show that anxiety disorders increase the risk of nausea by more than three times. That’s a significant jump, and it underscores just how powerful the mind-body connection really is when it comes to stress and our stomach.
Psychogenic and Anticipatory Vomiting
Two specific patterns emerge when we look closely at stress-related vomiting, and understanding these patterns can help you recognize what’s happening in your own body.
Psychogenic vomiting refers to vomiting that stems directly from psychological or emotional factors rather than a physical illness. There’s nothing wrong with your stomach itself—no virus, no food poisoning, no structural problem. Instead, your emotional state has become so overwhelming that your brain triggers a physical response. It’s your mind-gut connection working in overdrive, unable to process the emotional intensity any other way.
Anticipatory vomiting is perhaps even more distressing because it happens before the stressful event even occurs. Your body has learned to associate certain situations with extreme stress, and now just thinking about or approaching that situation triggers nausea and vomiting. It’s a conditioned response, similar to how Pavlov’s dogs learned to salivate at the sound of a bell.
Think about the student who vomits every morning during finals week, even before leaving for school. Or the person who becomes physically ill on the drive to a job interview. Their bodies have learned that these situations equal stress, and the vomiting reflex kicks in automatically. The anxiety of anticipation becomes its own trigger, creating a cycle that can be hard to break without proper support.
These patterns often serve as early warning signs that stress and anxiety are significantly affecting your physical health and quality of life.
Cyclic Vomiting Syndrome (CVS)
While most stress vomiting occurs in direct response to identifiable stressors, there’s a more complex condition where stress plays a major but not exclusive role. Cyclic Vomiting Syndrome (CVS) is a rare disorder that creates a particularly challenging pattern of symptoms.
CVS is characterized by severe, recurring episodes of intense nausea, vomiting, and exhaustion. These aren’t brief bouts of stress-related nausea—they’re dramatic episodes that can last for hours or even days, during which a person might vomit multiple times per hour. Between episodes, the person feels completely normal, which is one of the hallmarks of this condition.
The episodes tend to follow a predictable pattern, often starting at the same time of day and lasting for similar durations. What makes CVS particularly relevant to our discussion of what is stress vomiting is that stress is one of the most common triggers for these episodes. Other triggers include anxiety, excitement, lack of sleep, infections, and certain foods.
There’s also a fascinating link to migraines—many people with CVS either have migraines themselves or have family members who do. Researchers believe the conditions may share similar underlying mechanisms in the brain and nervous system.
If you experience severe, cyclical vomiting patterns, work with a healthcare provider for proper diagnosis and management. Organizations like The Cyclical Vomiting Syndrome Association UK provide valuable resources for understanding and managing this condition.
The Strong Link Between Anxiety and Nausea
The relationship between anxiety disorders and digestive symptoms, particularly nausea and vomiting, is one of the clearest demonstrations of the gut-brain connection at work. Different types of anxiety manifest in different ways, but they all have the potential to wreak havoc on your stomach.
Generalized Anxiety Disorder (GAD) keeps your body in a constant state of heightened alert. When you’re worrying about everything from your job performance to your relationships to world events, your stress response never fully turns off. This chronic activation means your digestive system is perpetually disrupted, leading to ongoing nausea, stomach discomfort, and sometimes vomiting.
Panic attacks represent the acute, intense end of the anxiety spectrum. During a panic attack, your stress response explodes into overdrive within seconds. Your heart races, you can’t catch your breath, the room spins—and your stomach often rebels violently. The sudden flood of stress hormones can trigger immediate nausea and vomiting as your body prioritizes survival functions over digestion.
Social anxiety disorder creates anticipatory stress around social situations. The fear of judgment, embarrassment, or scrutiny can build to such intensity that people experience severe nausea or vomiting before social events, presentations, or even casual gatherings. This can become self-perpetuating—the fear of becoming sick in public adds another layer of anxiety.
Post-Traumatic Stress Disorder (PTSD) leaves people with a hair-trigger stress response. Flashbacks, nightmares, or even subtle reminders of past trauma can activate the same intense physical reaction as the original traumatic event. This often includes severe nausea and vomiting as the body floods with stress hormones.
Recent research has confirmed what clinicians have observed for years: stress vomiting may be more common in people with more severe anxiety disorders. The more intense and pervasive your anxiety, the more likely you are to experience these physical manifestations.
Understanding how conditions like agoraphobia and panic can create physical symptoms helps us recognize that anxiety isn’t just happening in your head—it’s happening throughout your entire body, and your stomach is often the first to let you know something needs to change.
How to Stop Stress Vomiting: Management and Treatment
When you’re dealing with what is stress vomiting, you need both immediate relief and a long-term game plan. Think of it like putting out a fire while also fireproofing your house—you address the crisis in the moment, then build strategies to prevent it from happening again.
The truth is, stopping stress vomiting isn’t just about settling your stomach. It’s about understanding why your body is reacting this way and giving yourself the tools to calm both your mind and your gut. Let’s walk through what actually works.
Immediate Coping Strategies
When that wave of nausea hits and you feel like you might throw up, your body is screaming for help. Here’s how to answer that call in the moment.
Deep breathing exercises are your first line of defense. I know it sounds almost too simple, but slow, deliberate breaths genuinely interrupt the stress response. Try the four-four-four pattern: breathe in for four counts, hold for four, exhale for four. This activates your parasympathetic nervous system—basically, it tells your body “we’re safe now, stand down.”
Grounding techniques pull you out of the anxiety spiral and back into the present moment. The 5-4-3-2-1 method is particularly effective: identify five things you can see, four you can touch, three you can hear, two you can smell, and one you can taste. It sounds quirky, but it redirects your brain away from panic and toward concrete, calming observations.
Sipping cold water slowly can help settle your stomach. The key word is sipping—small amounts, not gulping. Cold water can be soothing, and staying hydrated helps prevent the added misery of dehydration if you do vomit.
Herbal teas have been used for centuries to calm upset stomachs for good reason. Ginger tea is famous for fighting nausea, but research shows peppermint can help reduce mild nausea too. Keep some peppermint tea bags handy, or even try inhaling the scent of diluted peppermint oil when nausea strikes.
Progressive muscle relaxation releases the physical tension that builds up when you’re stressed. Start at your toes and work upward—tense each muscle group for five seconds, then release. You’ll be surprised how much tension you’re holding in your shoulders, jaw, and stomach without even realizing it.
Sometimes the simplest fix is the most effective: step outside for fresh air. Stuffy, enclosed spaces can make nausea worse. A few minutes breathing deeply in fresh air can work wonders.
Long-Term Stress Management Techniques
Here’s the reality: if stress keeps triggering your vomiting, you need to address the stress itself. Band-aids help in the moment, but building resilience prevents the wounds from happening in the first place.
Regular exercise is one of the most powerful stress-busters we have. You don’t need to become a marathon runner—just 30 minutes of moderate activity most days makes a real difference. Exercise releases endorphins, those natural mood-lifters, and helps your body metabolize stress hormones more efficiently. Find something you actually enjoy, whether that’s dancing, hiking, swimming, or just walking around your neighborhood.
A healthy diet supports your gut health and gives your body the resources it needs to handle stress. This doesn’t mean perfection—it means being mindful about what you eat. Eating smaller, frequent meals instead of three large ones can prevent your stomach from feeling overwhelmed. Pay attention to foods that seem to trigger digestive issues for you and consider limiting them, especially during high-stress periods.
Quality sleep isn’t negotiable when you’re dealing with anxiety and stress vomiting. Aim for seven to nine hours per night. When you’re sleep-deprived, everything feels harder, your anxiety spikes, and your body struggles to regulate itself. Create a calming bedtime routine and stick to consistent sleep and wake times.
Mindfulness and meditation train your brain to respond differently to stress. Even 10 to 20 minutes daily can reshape how you react to anxiety-provoking situations. There are countless free apps and guided meditations available—find one that resonates with you and commit to it.
Identifying your triggers is detective work that pays off. Start noticing patterns. Does your stomach react before certain types of meetings? When you’re around specific people? When you’re running late? Once you know what sets you off, you can develop specific strategies to manage those situations—or sometimes, avoid them altogether.
Cognitive reframing is a game-changer. This technique, central to Cognitive Behavioral Therapy, involves catching and challenging the negative thoughts that fuel your anxiety. Instead of “I’m going to mess this up and everyone will judge me,” you learn to think “I’m prepared, and even if it’s not perfect, I’ll handle it.” Learning how CBT can transform negative thought patterns gives you a roadmap for this kind of mental shift.
Professional Treatment Options
Sometimes self-help strategies aren’t enough, and that’s completely okay. When stress vomiting is frequent, severe, or significantly impacting your daily life, professional treatment can be life-changing.
Cognitive Behavioral Therapy (CBT) is one of the most effective treatments for anxiety disorders, which are often at the root of stress vomiting. CBT helps you identify the thought patterns and behaviors that keep you stuck in anxiety cycles, then teaches you practical skills to break free. It’s not just talk therapy—it’s skills training that changes how your brain processes stress.
Anti-anxiety medications may be recommended by your healthcare provider if your anxiety is severe. These medications, called anxiolytics, can help manage symptoms while you work on longer-term solutions through therapy. They’re typically used short-term or alongside therapy, not as a standalone solution.
Anti-nausea medications (antiemetics) can provide temporary relief during acute episodes. Your doctor can prescribe these if you’re experiencing frequent vomiting that’s affecting your ability to eat, work, or function normally. They treat the symptom while you address the underlying cause.
For those dealing with severe anxiety that’s disrupting their life, Intensive Outpatient Programs (IOP) and Partial Hospitalization Programs (PHP) offer comprehensive, structured treatment without requiring residential care. These programs combine individual therapy, group therapy, and skills training to address the root causes of your anxiety and build lasting coping strategies. Our telehealth therapy and outpatient programs bring this expert-led care directly to you, whether you’re in California, Indiana, or anywhere else—with flexible scheduling options including evening sessions.
The bottom line? Stress vomiting responds to treatment when you address both the physical symptoms and the underlying stress and anxiety. You don’t have to keep living with your stomach in knots.
When to Seek Professional Help
Sometimes what is stress vomiting moves beyond something you can manage on your own. Your body is telling you it needs more support—and that’s not a sign of weakness. It’s actually a sign of self-awareness.
You should reach out to a healthcare provider if you’re experiencing frequent or severe vomiting. When episodes happen regularly or become intense enough to disrupt your day, that’s your signal to get professional help. Your body shouldn’t have to work this hard to process stress.
Dehydration is a serious concern. If you can’t keep fluids down, or you notice signs like decreased urination, dry mouth, excessive thirst, or feeling lightheaded, you need medical attention quickly. Dehydration can escalate fast and create additional health complications beyond the stress itself.
Blood in your vomit always requires immediate medical attention. This isn’t something to wait out or monitor at home. The same goes for severe abdominal pain—intense or persistent stomach pain alongside vomiting should be evaluated by a doctor right away to rule out other medical conditions.
Unexplained weight loss is another red flag. If stress vomiting is preventing you from eating normally and you’re losing weight without trying, your body isn’t getting the nourishment it needs. This creates a cycle where physical weakness can actually make stress feel even more overwhelming.
Think about your daily life. If stress vomiting interferes with your work, school, social activities, or overall quality of life, that’s your answer. You deserve to live without constantly worrying about when the next episode might hit. You shouldn’t have to plan your day around access to a bathroom or avoid situations that matter to you because of this symptom.
A medical evaluation serves another important purpose: ruling out other conditions. While stress may be the primary trigger, a doctor can help determine if there’s another underlying medical cause contributing to your symptoms. Getting the correct diagnosis ensures you receive the most effective treatment.
You don’t have to manage this alone. Professional mental health services can provide the support and strategies that make a real difference. Understanding the benefits of utilizing mental health services can help you take that first step toward relief.
At Thrive Mental Health, we offer flexible, expert-led, evidence-based care custom to your individual needs. We understand that finding affordable and accessible mental health support can feel overwhelming—especially when you’re already dealing with physical symptoms. That’s why we work with various insurance providers, including Cigna, Optum, and Florida Blue, to make our programs more accessible.
Whether you’re in Indiana or California, our virtual and hybrid programs ensure you can receive the care you need from anywhere. You don’t have to choose between getting help and managing the logistics of your daily life. We meet you where you are.
Frequently Asked Questions about Stress Vomiting
You’re not alone if you have questions about what is stress vomiting means for your health. These are some of the most common concerns I hear from clients, and I want to address them clearly and honestly.
How can I tell if my vomiting is from stress or something else?
The timing tells you a lot. Stress vomiting typically happens during periods of high anxiety—right before a big meeting, during a conflict, or when you’re anticipating something stressful. Unlike a stomach bug or food poisoning, you won’t usually have a fever, body aches, or other signs of physical illness.
Here’s what makes stress vomiting distinct: it’s closely tied to your emotional state. When the stressor passes or lessens, your symptoms often improve. That said, if you’re vomiting without any clear connection to stress, or if it continues even after you’ve calmed down, it’s time to see a doctor. Other medical conditions can cause similar symptoms, and ruling those out is crucial.
Can stress cause you to throw up every day?
Yes, unfortunately it can. When you’re dealing with chronic stress or a severe anxiety disorder, your body doesn’t get a chance to fully relax. You remain in that heightened “fight-or-flight” state day after day, and your digestive system pays the price.
This constant activation keeps disrupting normal digestion. Your gut becomes hypersensitive, overreacting to sensations that wouldn’t normally bother you. The result? Daily nausea or vomiting that feels relentless and exhausting. If this sounds familiar, please know that you don’t have to live this way—professional treatment can help break this cycle.
Does throwing up relieve stress?
This is an important question, and the answer might surprise you. While some people do feel a momentary physical relief after vomiting—the nausea subsides temporarily—vomiting doesn’t actually resolve your stress or anxiety. It doesn’t address what’s causing those feelings in the first place.
What’s more concerning is that for some people, vomiting can become a conditioned response. Your brain starts to associate stress with vomiting, and the pattern reinforces itself. Before you know it, your body automatically reacts with nausea whenever you feel anxious, creating a harmful cycle that’s increasingly difficult to break. This is why addressing the underlying stress through therapy and coping strategies is so important.
What should I eat after stress vomiting?
Your stomach needs gentle care after an episode. Start by rehydrating slowly—take small, frequent sips of clear liquids like water or electrolyte drinks. Avoid gulping, and stay away from sugary or acidic beverages that might irritate your stomach further.
Once you’re keeping liquids down and feel ready for food, introduce bland, easily digestible options. Think crackers, plain toast, white rice, or applesauce—foods that are part of what’s often called the BRAT diet (bananas, rice, applesauce, toast). Keep portions small at first.
As your stomach settles over the next few hours or days, you can gradually reintroduce your normal diet. Listen to your body—it will tell you when it’s ready for more complex foods. If you’re having trouble keeping anything down for more than 24 hours, that’s a sign to seek medical attention.
Take Control of Your Health Today
You’ve learned what is stress vomiting is—a very real physical response to emotional and psychological overwhelm. And here’s what matters most: it’s treatable. You don’t have to live with the constant fear that stress will send you running to the bathroom or keep you from living your life fully.
The path forward isn’t just about managing nausea in the moment. It’s about addressing what’s driving the stress and anxiety in the first place. When you tackle the root cause—whether that’s an anxiety disorder, unprocessed trauma, or chronic life stressors—the physical symptoms often improve dramatically or disappear entirely.
Think of stress vomiting as your body’s alarm system. It’s not broken; it’s actually working overtime to tell you something needs attention. By combining immediate relief techniques like deep breathing and grounding with long-term strategies like regular exercise, healthy eating, and quality sleep, you create a foundation for lasting change. And when self-care isn’t enough—which is completely normal and nothing to feel ashamed about—professional support can make all the difference.
At Thrive Mental Health, we’ve built our programs around one core belief: you deserve care that actually fits your life. Our virtual and hybrid Intensive Outpatient (IOP) and Partial Hospitalization (PHP) programs offer comprehensive, evidence-based treatment that meets you where you are. Whether you’re managing a demanding job, caring for family, or simply need flexibility, our evening options ensure treatment doesn’t mean putting your life on hold.
Our expert clinicians understand the mind-body connection intimately. We’ve helped countless individuals break free from the cycle of stress-induced physical symptoms by addressing anxiety, building resilience, and teaching practical coping skills that work in real-world situations. You’ll work with a dedicated team who sees you as a whole person, not just a set of symptoms.
We also know that cost and insurance coverage are real concerns. That’s why we work with Cigna, Optum, Florida Blue, and other major insurers to make quality mental health care accessible. Whether you’re in Indiana, California, or anywhere else through our virtual programs, you can get the support you need.
Ready for support? Thrive offers virtual and hybrid IOP/PHP with evening options. Verify your insurance in 2 minutes (no obligation) → Start benefits check or call 561-203-6085.
If you’re in crisis, call/text 988 right now. You are not alone.
