What is Trauma Unpacking Responses and Vicarious Experiences
What is Trauma? (And Why It’s Not Just “In Your Head”)

What is trauma? Trauma is a deeply personal response to distressing events, not the event itself. It’s the overwhelming psychological and physical reaction that occurs when your ability to cope is exceeded—leaving you feeling helpless, unsafe, or fundamentally changed.
Quick Answer:
- Trauma is the response, not the event. Two people can experience the same situation—one may process it without lasting impact, while the other develops symptoms.
- It’s incredibly common. Nearly 90% of U.S. adults have faced at least one potentially traumatic event in their lifetime.
- It affects your whole system. Trauma rewires your brain, dysregulates your nervous system, and can impact your relationships, physical health, and sense of self.
- Healing is possible. With the right support and evidence-based treatment, you can process trauma and reclaim control of your life.
Feeling stuck in survival mode—hypervigilant, exhausted, disconnected? You might not even realize that what you’re experiencing is trauma. Understanding what trauma actually is, and how it shows up in your life, is the first step toward getting control back.
This guide unpacks the science behind trauma, its hidden effects, and the proven paths to recovery. Whether you’re dealing with a single event or years of accumulated stress, you’ll learn how to recognize trauma’s impact and what to do about it.
I’m Nate Raine, CEO of Thrive Mental Health, and I’ve spent over a decade leading behavioral health innovation—building programs that help people understand what is trauma and access the intensive, evidence-based care that makes real recovery possible. At Thrive, we’ve helped thousands of adults move beyond survival and into healing through trauma-informed IOP and PHP programs across Florida.
Handy what is trauma terms:
What is Trauma? [The Clinical Definition vs. The Human Experience]
To truly grasp what is trauma, we must look beyond a simple definition. The American Psychological Association (APA) defines trauma as “any disturbing experience that results in significant fear, helplessness, dissociation, confusion, or other disruptive feelings intense enough to have a long-lasting negative effect on a person’s attitudes, behavior, and other aspects of functioning” APA Dictionary of Psychology. This clinical understanding highlights that trauma isn’t just about the event itself, but our subjective, deeply personal response to it.
For us, this means recognizing that while an event might be objectively distressing, it’s the internal experience—the feeling of being overwhelmed, the shattered sense of safety, the profound helplessness—that defines what is trauma. Our ability to cope is exceeded, leaving us with a lingering sense of threat even when the danger has passed. This profound disruption can manifest as the classic fight, flight, or freeze response, becoming a default setting in our nervous system.

The Events That Cause Trauma
The events that can trigger trauma are as varied as human experience itself. They can be sudden, isolated incidents or prolonged, insidious experiences that erode our sense of self over time. Often, these are events that challenge our view of the world as a just, safe, and predictable place APA Dictionary of Psychology.
Here’s a list of Potentially Traumatic Events (PTEs) that can lead to a trauma response:
- Single-incident events: These are often one-time, unexpected occurrences like serious accidents (e.g., car crashes), violent assaults (e.g., muggings, rape), or sudden, unexpected loss of a loved one. The research indicates that the sudden loss of a loved one is the most commonly reported individual traumatic event, and witnessing death or serious bodily harm is the second most common.
- Chronic stressors: These involve repeated or prolonged exposure to distressing situations. Examples include ongoing physical, sexual, or emotional abuse, domestic violence, neglect, bullying, or living in poverty where exposure to violence and instability is constant.
- Witnessing harm to others: Experiencing trauma isn’t limited to direct exposure. Witnessing violent acts, serious injuries, or death inflicted upon others can be deeply traumatizing.
- Natural disasters: Events like earthquakes, hurricanes, floods, or wildfires can cause widespread trauma, impacting entire communities.
- Combat exposure: Military personnel frequently face life-threatening situations, leading to high rates of trauma. Recurrent physical violence, such as combat, carries the highest risk of developing PTSD, ranging from 13% to 14%.
- Serious medical diagnoses or procedures: A life-threatening illness, invasive medical procedures, or prolonged hospitalization can also be deeply traumatic, especially if there’s a perceived loss of control or significant pain.
Who Is Most at Risk?
It’s a common misconception that trauma only affects certain populations. In reality, trauma has no boundaries regarding age, gender, socioeconomic status, race, ethnicity, or sexual orientation screening.mhanational.org. Studies show that approximately 70% of individuals worldwide report experiencing lifetime traumas, and nearly 90% of adults in the U.S. report exposure to at least one potentially traumatic event during their lifetime [statpearls.com].
However, while trauma is ubiquitous, certain populations and factors can increase vulnerability:
- Vulnerable populations:
- Children and the elderly: The risk of developing PTSD follows a bimodal pattern, with the highest risks during childhood, adolescence, and after age 65 [statpearls.com]. Children’s developing brains are particularly vulnerable to long-lasting impacts, and severe social neglect or deprivation can lead to specific attachment disorders [psychiatry.org].
- First responders and veterans: Professions with repeated exposure to traumatic events (police, firefighters, paramedics, military personnel) face heightened risks.
- Individuals with pre-existing mental health conditions: Trauma is especially common in the lives of people with mental and substance use disorders [screening.mhanational.org].
- Risk factors: Prior trauma exposure, particularly in childhood, significantly increases the likelihood of developing PTSD later in life [nimh.nih.gov]. A lack of social support, pre-existing mental health conditions, and genetic predispositions can also contribute to vulnerability [pubmed.ncbi.nlm.nih.gov/11068961].
- Systemic factors: Poverty, racism, discrimination, and community violence disproportionately affect certain groups, increasing their exposure to trauma. For example, racially motivated shootings can add to the trauma and grief experienced by Black Americans [apa.org]. Culturally responsive care is often needed to address trauma and chronic stress resulting from systemic issues like U.S. immigration policy [apa.org].
3 Types of Trauma You Need to Know [Acute, Chronic, & Complex]
Trauma is not one-size-fits-all. Its manifestations are incredibly diverse, shaped by the nature of the event, its duration, and our individual circumstances. Understanding these different types of trauma is crucial for identifying the right support and validating the experiences of ourselves and others.
Acute, Chronic, and Complex Trauma
These categories help us understand the patterns and severity of traumatic experiences:
| Type of Trauma | Description | Examples | Potential Impact |
|---|---|---|---|
| Acute Trauma | A single, highly stressful event. The psychological response is often immediate and intense, though symptoms typically last from a few days to a few months. | A car accident, a sudden violent assault, a natural disaster, sudden death of a loved one. | Shock, anxiety, fear, difficulty sleeping. If unresolved, can lead to PTSD. |
| Chronic Trauma | Prolonged or repeated exposure to distressing experiences. Differs from acute trauma in its ongoing nature. | Living in a war zone, recurrent bullying, long-term poverty, ongoing domestic violence. | Persistent anxiety, depression, hypervigilance, emotional numbness, difficulties with trust and relationships. |
| Complex Trauma (C-PTSD) | Multiple, chronic, or prolonged exposure to traumatizing events, often interpersonal in nature and occurring in childhood. It involves not just symptoms of PTSD but also pervasive difficulties with self-concept, emotional regulation, and relationships. | Childhood abuse or neglect, abandonment, prolonged captivity, human trafficking. | Severe difficulties forming healthy attachments, identity confusion, emotional dysregulation, chronic feelings of shame/guilt, dissociation. |
Complex PTSD, in particular, tends to result from long-term, chronic trauma and can profoundly affect a person’s ability to form healthy, trusting relationships [camh.ca]. When experienced in childhood, it’s often referred to as ‘developmental trauma’ [camh.ca]. At Thrive Mental Health, we offer specialized trauma-focused care designed to address these deep-seated impacts.
Vicarious, Collective, and Moral Trauma
Beyond individual experiences, trauma can also manifest on broader scales:
- Secondary/Vicarious Trauma: This occurs when we witness trauma or are closely connected to it without directly experiencing the event ourselves. It’s common among professionals like therapists, first responders, journalists, or healthcare workers who are repeatedly exposed to the suffering of others. Its effects can be similar to general trauma [cookiepro.com].
- Collective Trauma: When a traumatic event happens to a large number of people at the same time, it can lead to collective trauma. This shared experience can manifest in both personal symptoms and ‘social symptoms’ like societal reactions or avoidance of certain groups. Examples include natural disasters, pandemics, or acts of terrorism [cookiepro.com]. The 2023 Stress in America™ report highlighted the psychological impacts of collective trauma, including increased stress and chronic health issues [apa.org].
- Generational Trauma: Also known as intergenerational trauma, this refers to trauma experienced across generations of a family, culture, or group. It impacts current generations through learned behaviors, environmental factors, or how older generations were parented. Emerging research suggests trauma can lead to epigenetic changes—alterations in gene expression—that can be passed down to offspring, influencing their stress response and susceptibility to mental health issues [ncbi.nlm.nih.gov/pmc/articles/PMC6127768/].
- Moral Injury: This distinct form of trauma arises when we’re put in a situation that goes against our deep-seated morals, values, or beliefs. It’s often seen in contexts requiring difficult decisions about others’ lives, such as military combat, or working within failing systems, like healthcare. Feelings of guilt, shame, and betrayal are central to moral injury [protect-advice.org.uk].
- Racial Trauma: The mental and emotional injury caused by racial bias, discrimination, and exposure to racism. This can be acute (e.g., a hate crime) or chronic (e.g., daily microaggressions, systemic oppression), leading to profound psychological distress and impacting an individual’s sense of safety and belonging.
The Lasting Impact: How Trauma Rewires Your Brain, Body, and Life
The effects of trauma are far-reaching, fundamentally altering not just our minds but our bodies and relationships. It’s often said that “the body keeps the score,” and this couldn’t be more accurate when it comes to what is trauma.
The Physical and Neurological Impact of what is trauma
Trauma leaves an indelible mark on our biology. Our brains, designed for survival, adapt to constant threat, often getting stuck in a state of hyperarousal. This involves several key neurological changes:
- HPA Axis Dysregulation: The Hypothalamic-Pituitary-Adrenal (HPA) axis, our central stress response system, becomes dysregulated. This can lead to abnormal cortisol levels, which are crucial for stress regulation. Individuals with PTSD, for example, have shown improved suppression of cortisol after certain tests according to research published in the Journal of Nervous and Mental Disease.
- Brain Structure Alterations: Key brain areas are affected:
- Amygdala: This “fear center” often becomes overactive, leading to increased fear responses and hypervigilance, as documented in neuroimaging studies of PTSD patients.
- Hippocampus: Responsible for memory and spatial navigation, the hippocampus can shrink in volume, which may contribute to memory problems and difficulty differentiating past trauma from present safety, according to research in Biological Psychiatry.
- Prefrontal Cortex (PFC): Involved in executive functions like decision-making, emotional regulation, and impulse control, the PFC can become less active. This can impair our ability to calm ourselves and think rationally under stress, as shown in functional MRI studies.
- Chronic “Fight or Flight”: The sympathetic nervous system remains on high alert, leading to persistent physical symptoms such as fatigue, chronic pain, headaches, digestive issues, and cardiovascular problems documented in psychosomatic medicine research.
- Increased Risk for Long-Term Health Problems: This chronic physiological stress increases the risk for a host of physical health conditions, including autoimmune disorders, heart disease, and diabetes. The Adverse Childhood Experiences (ACE) Study powerfully demonstrated the relationship between childhood abuse and household dysfunction and many of the leading causes of death in adults [https://www.ajpmonline.org/article/S0749-3797(98)00017-8/fulltext].
Recognizing the Signs: The Emotional and Psychological Symptoms of what is trauma
Crisis Support: If you’re in crisis or struggling with thoughts of self-harm, call or text 988 right now. You are not alone.
Understanding what is trauma also means recognizing its diverse emotional and psychological footprint. While many people recover from traumatic events without lasting negative effects, others experience significant difficulties [screening.mhanational.org].
- PTSD vs. Acute Stress Disorder (ASD): It’s important to distinguish between these. ASD symptoms occur within three days to one month after a traumatic event, while Posttraumatic Stress Disorder (PTSD) symptoms must last for more than a month and significantly interfere with daily life [psychiatry.org]. About half of individuals with ASD go on to develop PTSD. Common symptoms of PTSD fall into four categories:
- Intrusive memories: Unwanted, recurring memories of the event, vivid flashbacks (feeling like you’re reliving the trauma), or distressing nightmares [psychiatry.org].
- Avoidance behaviors: Actively avoiding places, people, activities, objects, or situations that remind you of the traumatic event. This can also include internal avoidance, like trying to suppress thoughts or feelings related to the trauma [psychiatry.org].
- Negative changes in mood and thinking: Persistent negative beliefs about oneself, others, or the world; feelings of guilt, shame, fear, or anger; emotional numbness; loss of interest in activities once enjoyed; difficulty remembering key aspects of the trauma [psychiatry.org].
- Hyperarousal and reactivity: Being constantly “on edge,” easily startled, irritable, having angry outbursts, difficulty concentrating, or experiencing sleep problems [psychiatry.org].
- Comorbidities: Trauma, particularly childhood trauma, is strongly associated with other mental health conditions. Research suggests children who experience trauma are twice as likely to develop a mental health condition in the future [bmj.com]. Common comorbidities include depression, anxiety disorders, and substance use disorders, which can often be a way of self-medicating the pain of trauma according to research in the American Journal of Psychiatry. Trauma exposure is also strongly associated with suicidal ideation and suicide attempts across the lifespan [statpearls.com]. Additionally, exposure to at least one traumatic event can significantly increase the risk of developing paranoid ideations and verbal hallucinations [statpearls.com].
How Trauma Fractures Connections
What is trauma if not a profound disruption of our ability to connect? Traumatic experiences impact relationships across various levels, including interpersonal connections, community dynamics, and even interactions within healthcare systems [istss.org].
- Difficulty with trust and intimacy: Trauma, especially complex trauma stemming from relational neglect or abuse, can make it incredibly difficult to trust others. This can lead to challenges in forming and maintaining intimate relationships, as the fear of betrayal or abandonment looms large.
- Social isolation and withdrawal: The emotional numbness, shame, and hypervigilance associated with trauma can lead to social isolation. We might withdraw from friends and family, feeling disconnected or believing no one can truly understand our experience.
- Strained family and romantic relationships: Heightened emotions like anger or aggression, or a tendency toward numbing and isolation, can strain existing relationships. Communication can break down, and partners or family members may struggle to understand our reactions.
- Impact on parenting and attachment styles: Trauma experienced in childhood can affect our own parenting styles, potentially perpetuating cycles of insecure attachment. Generational trauma, passed down through family dynamics, can influence how we relate to our children and how they, in turn, relate to the world [cookiepro.com].
- Feeling disconnected from others: A pervasive sense of detachment, sometimes described as derealization (feeling like you’re in a dream) or depersonalization (feeling outside your own body), can make genuine connection seem impossible [psychiatry.org].
How to Heal From Trauma: 5 Therapies That Actually Work
The journey of healing from trauma is not about erasing the past, but about integrating it into your life in a way that allows you to move forward. It’s a testament to human resilience, and with the right support, profound recovery is not just possible—it’s within reach.
Getting a Clear Diagnosis
The first critical step in addressing what is trauma and its impact is obtaining a professional evaluation. This helps us understand the specific nature of your symptoms and rule out other potential medical or psychological conditions that might mimic trauma responses.
- Importance of a professional evaluation: A thorough assessment by a trauma-informed clinician is crucial. They can differentiate between acute stress reactions, PTSD, and complex PTSD, which require nuanced approaches.
- Ruling out other medical conditions: Physical symptoms of trauma can sometimes overlap with other health issues. A comprehensive evaluation helps ensure that underlying medical conditions are not overlooked.
- Using validated assessment tools: Clinicians use specific, psychometrically sound tools to aid in diagnosis. For example, the Clinician-Administered PTSD Scale for DSM-5 (CAPS-5) is a structured interview widely used to assess PTSD symptoms [pubmed.ncbi.nlm.nih.gov/28493729]. Other tools like the Impact of Event Scale-Revised (IES-R) are also valuable [pubmed.ncbi.nlm.nih.gov/17369016].
- The role of a trauma-informed clinician: In Florida, our Thrive Mental Health clinicians are trained to recognize the subtle and overt signs of trauma, providing a safe and non-judgmental space for evaluation and treatment. They understand that trauma symptoms are often coping strategies developed in response to overwhelming stressors [camh.ca].
If you are in Florida—from Miami, Orlando, and Tampa Bay to Jacksonville, Boca Raton, and West Palm Beach—you can access our trauma-informed teams virtually or in person. We serve clients across the state, including in Fort Lauderdale, Naples, Sarasota, and St. Petersburg.
Therapies That Rebuild Safety and Control
Effective trauma treatment focuses on helping you process traumatic memories, regulate emotions, and rebuild a sense of safety and control. Therapy is the mainstay treatment for trauma-associated symptoms [statpearls.com].
- Trauma-Focused Cognitive Behavioral Therapy (TF-CBT): This approach helps you identify and challenge negative thought patterns related to the trauma, develop coping skills, and gradually process traumatic memories.
- Eye Movement Desensitization and Reprocessing (EMDR): EMDR involves guided eye movements or other bilateral stimulation while you recall distressing memories. It helps to reprocess these memories, reducing their emotional intensity. EMDR has been shown to be as effective as trauma-focused CBT in treating PTSD [pubmed.ncbi.nlm.nih.gov/16740177].
- Prolonged Exposure (PE): This therapy involves gradually confronting trauma-related memories, feelings, and situations that you have been avoiding. This helps reduce the fear and anxiety associated with them. PE has been shown to be highly effective, sometimes even more so than Cognitive Processing Therapy (CPT) [pubmed.ncbi.nlm.nih.gov/12182270].
- Somatic Experiencing (SE): SE focuses on the body’s physiological responses to trauma, helping you release stored tension and regulate your nervous system.
- Pharmacotherapy (SSRIs/SNRIs): Medications, particularly Selective Serotonin Reuptake Inhibitors (SSRIs) and Selective Norepinephrine Reuptake Inhibitors (SNRIs), are often used to manage symptoms like depression, anxiety, and hyperarousal associated with PTSD. Paroxetine and sertraline are FDA-approved for PTSD [statpearls.com]. A combination of psychotherapy and pharmacotherapy can be particularly effective [pubmed.ncbi.nlm.nih.gov/21908494].
- Higher levels of care: For individuals who need more intensive support than weekly outpatient therapy, programs like Virtual Intensive Outpatient Programs (IOP) or Partial Hospitalization Programs (PHP) offer structured, comprehensive treatment. Thrive Mental Health provides these programs virtually across Florida, offering flexible scheduling and expert-led care.
If you are unsure whether you need IOP, PHP, or weekly therapy, you can start by exploring our virtual IOP overview and then complete a quick insurance benefits check to see your options.
Building Resilience with Trauma-Informed Care
Resilience is not an innate trait; it’s a skill that can be developed and strengthened. It’s defined as the ability to adapt to significant change or overwhelming stressors, utilizing adaptive cognitions and behaviors that promote recovery from psychological insult [statpearls.com].
Trauma-informed care is a best practice that guides our approach to healing. It operates on five key principles:
- Safety: Ensuring physical and emotional safety for all individuals.
- Trustworthiness: Building trust through clear boundaries and consistency.
- Peer Support: Connecting individuals with shared experiences.
- Collaboration: Working together with individuals in their healing journey.
- Empowerment, Voice, and Choice: Valuing and strengthening individuals’ voices and choices in their treatment.
By integrating these principles, we create environments where healing can truly begin. At Thrive Mental Health, our programs are built on a foundation of trauma-informed care, helping you not only cope with the effects of trauma but also build lasting resilience. To dive deeper into how trauma shapes your thoughts and relationships, you can also read our related article on complex trauma, which explores how early experiences can echo into adulthood.
Frequently Asked Questions about Trauma
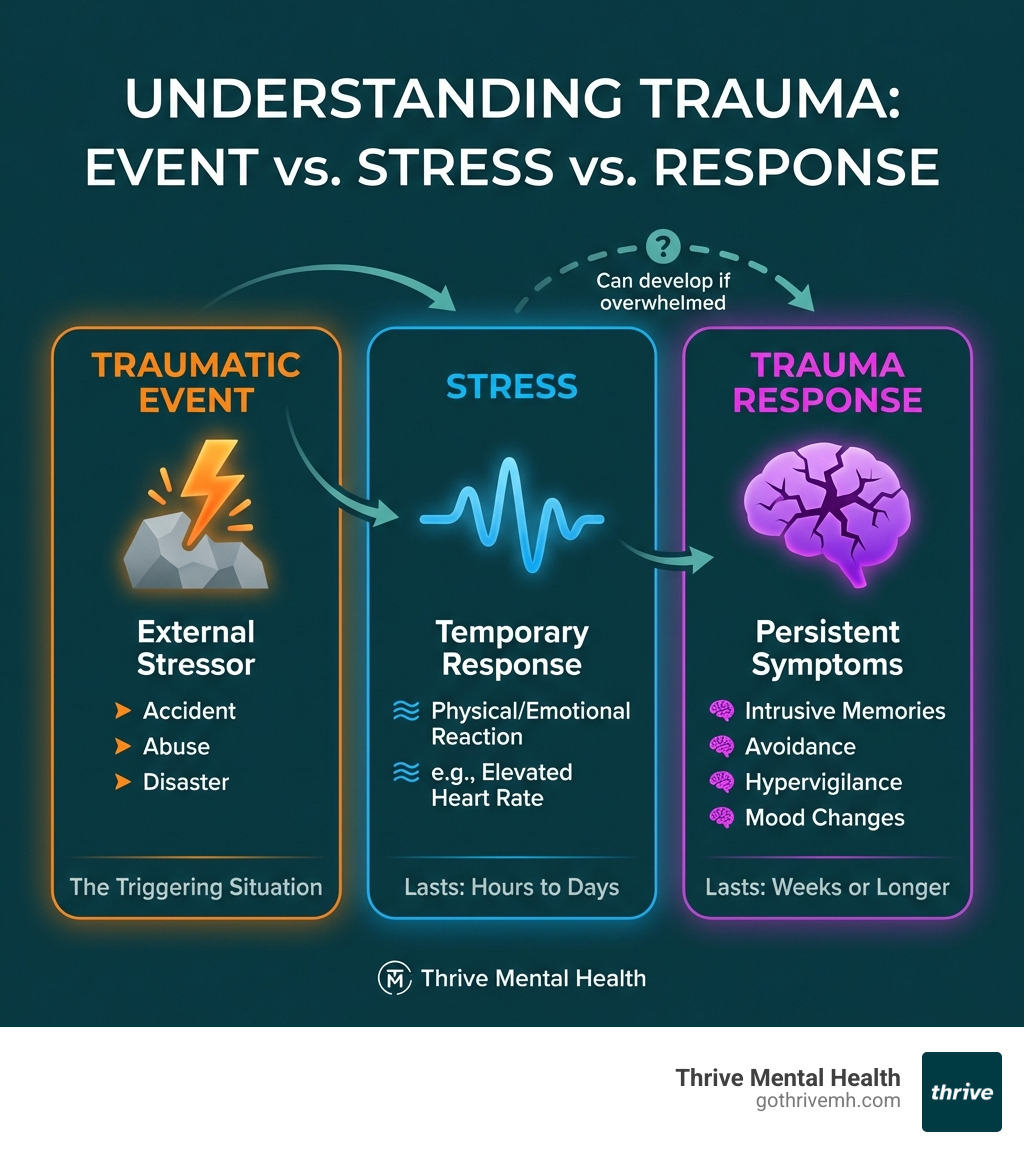
What is the difference between trauma and stress?
Stress is a normal reaction to a challenge, whether it’s a deadline at work or an argument with a friend. While stress can be uncomfortable, it’s typically manageable and resolves once the stressor is gone. Trauma, on the other hand, is a response to an event that is so overwhelming and distressing that it exceeds your ability to cope. It leaves a lasting impact on your mental, emotional, and physical well-being, often altering your sense of safety and fundamentally changing how you perceive the world.
Can you have trauma without developing PTSD?
Yes, absolutely. Many people experience traumatic events and their associated symptoms without meeting the full diagnostic criteria for Post-Traumatic Stress Disorder (PTSD). You can still experience significant distress, such as anxiety, depression, difficulty sleeping, or relationship challenges, even if your symptoms don’t perfectly align with a PTSD diagnosis. In these cases, trauma-informed support and therapy can still be incredibly beneficial for processing your experiences and improving your quality of life.
How long does it take to recover from trauma?
There is no set timeline for healing from trauma, as recovery is a deeply personal and non-linear process. The duration depends on many factors, including the type and severity of the trauma, individual risk factors, the support system available, and the type of treatment received. Some individuals may experience significant improvement within months, while others may require years of ongoing support. The goal isn’t to “get over” trauma, but to integrate the experience in a way that allows you to live a fulfilling life. With effective, evidence-based care, significant and lasting improvement is always possible.
Take the First Step Toward Healing Today
What is trauma? It’s a common and treatable response to overwhelming life events. Its effects can be profound, impacting your mental, physical, and relational health, but you do not have to manage it alone. With evidence-based, trauma-informed care, you can process your experiences, develop healthy coping skills, and build a resilient future. Thrive Mental Health provides expert-led programs designed for adults who need more than weekly therapy, with flexible options that fit your life and accept major insurance plans like Cigna, Optum, Florida Blue, Aetna, and more.
Whether you live in Florida—including Tampa Bay, St. Petersburg, Miami, Orlando, Boca Raton, West Palm Beach, Jacksonville, Fort Lauderdale, Naples, or Sarasota—you can access Thrive’s virtual and hybrid programs from home or one of our local centers.
Ready for support? Thrive offers virtual and hybrid IOP/PHP programs with evening options. Verify your insurance in 2 minutes (no obligation) → Start benefits check or call 561-203-6085. If you’re in crisis, call/text 988.