The 5 Best Mental Health Services for Dissociative Disorders

Feeling Disconnected? Here’s How to Find Your Way Back
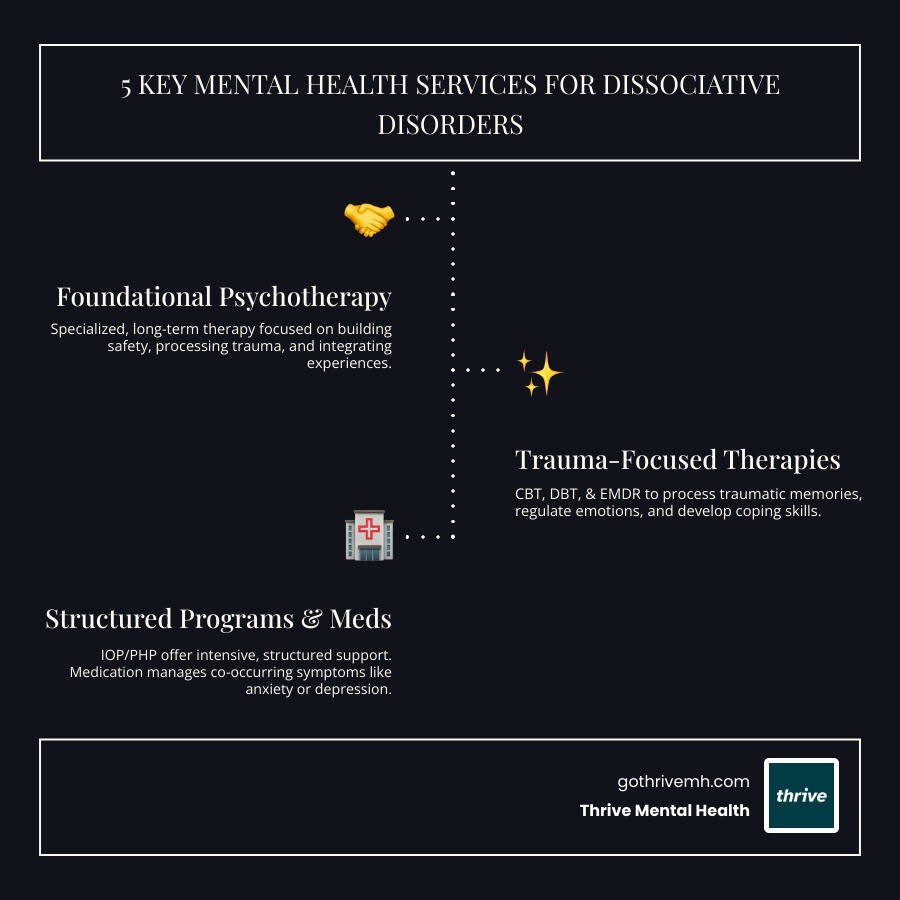
Which recommended mental health services support dissociative disorders? The most effective services include:
- Specialized, phase-oriented psychotherapy – Long-term individual therapy addressing trauma, safety, and integration
- Trauma-focused therapies – CBT, DBT, and EMDR to process memories and regulate emotions
- Intensive Outpatient Programs (IOP) – Structured support with multiple sessions per week
- Partial Hospitalization Programs (PHP) – Daily treatment for crisis stabilization without inpatient admission
- Medication management – Antidepressants and mood stabilizers to treat co-occurring depression and anxiety
If you’ve ever felt like you’re watching your life from the outside or lost time you can’t account for, you’re not alone. While up to 75% of people experience a fleeting dissociative episode, for some, it becomes a chronic disorder rooted in overwhelming trauma. About 90% of people with Dissociative Identity Disorder (DID), for instance, have a history of severe childhood abuse. The good news? Recovery is possible, but it requires more than traditional weekly therapy.
You need a specialized, trauma-informed approach to feel whole again. I’m Nate Raine, CEO of Thrive Mental Health. We’ve built our evidence-based IOP and PHP programs across Florida on a deep understanding of which recommended mental health services support dissociative disorders. We’ve seen how this structured care helps people move from fragmentation to integration.
Important Which recommended mental health services support dissociative disorders? terms:
- 24 hour mental health helpline
- Options for intensive mental health treatment
- Crisis intervention mental health services
First, What Are Dissociative Disorders? (And Why You Feel “Disconnected”)
Dissociative disorders are serious mental health conditions characterized by an involuntary escape from reality, creating a disconnection between your thoughts, identity, and memories. It’s more than just “spacing out”—it’s a significant disruption often developed as a coping mechanism for severe trauma, especially in childhood. The mind compartmentalizes traumatic experiences as a way to survive.
Diagnosing these disorders requires a qualified mental health professional to assess symptoms and history after ruling out medical causes like brain injuries. This ensures your treatment is custom to your needs. You can learn more from the American Psychiatric Association: Dissociative Disorders overview from a trusted source.
What are the primary types of dissociative disorders?
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) defines several types:
- Dissociative Identity Disorder (DID): Marked by having two or more distinct personality states that take control of behavior, accompanied by memory gaps beyond ordinary forgetfulness.
- Depersonalization/Derealization Disorder: Involves persistent feelings of being detached from one’s own body (depersonalization) or feeling that one’s surroundings are unreal (derealization).
- Dissociative Amnesia: Characterized by an inability to recall important personal information, typically related to trauma, that is too significant to be normal forgetting.
- Other Specified Dissociative Disorder (OSDD): A diagnosis for significant dissociative symptoms that cause distress but don’t meet the full criteria for the other specific disorders.
Understanding these distinctions is crucial for effective treatment. For more comprehensive information, consider resources like the Mayo Clinic: More on the types of dissociative disorders.
What are the common symptoms and causes?
Common symptoms often overlap with other conditions, making diagnosis complex. Key signs include:
- Memory loss (amnesia): Forgetting traumatic events, daily activities, or personal information.
- Out-of-body experiences: Feeling like you are watching yourself from the outside (depersonalization).
- Emotional numbness: A sense of detachment from your own feelings.
- Identity confusion or alteration: Feeling unsure about who you are or experiencing multiple identities.
- Derealization: A feeling that the world around you is unreal, foggy, or distorted.
- Co-occurring mental health problems: Depression, anxiety, and suicidal thoughts are common.
The primary cause of dissociative disorders is severe, prolonged trauma, especially during childhood. The brain dissociates as a survival mechanism to escape unbearable pain or fear. Key causes include:
- Childhood abuse and neglect: About 90% of people with DID in the U.S., Canada, and Europe experienced childhood abuse or neglect.
- Overwhelming trauma: Events like war, natural disasters, or early medical trauma can also be triggers.
- Disrupted childhood attachment: An unstable early environment can impair the development of a cohesive self, increasing vulnerability to dissociation.
While dissociation is a powerful defense, chronic use disrupts daily life. Effective treatment must address these root causes.
The 5 Recommended Mental Health Services That Actually Work
When it comes to which recommended mental health services support dissociative disorders, a comprehensive, trauma-informed approach is non-negotiable. These complex conditions require more than a one-size-fits-all solution. At Thrive Mental Health, we integrate evidence-based treatments within a supportive, structured environment to help you heal.
1. Specialized, Phase-Oriented Psychotherapy
This long-term therapy is the foundation of treatment. It focuses on building a strong, trusting relationship with a therapist who understands trauma. Treatment follows a three-phase model recommended by experts like the International Society for the Study of Trauma and Dissociation (ISSTD):
- Phase 1: Safety and Stabilization: The priority is establishing safety. This involves learning coping skills to manage intense emotions, control dissociative symptoms, and reduce self-harm.
- Phase 2: Trauma Processing: Once stable, you’ll carefully work through and integrate traumatic memories with your therapist’s guidance to prevent re-traumatization.
- Phase 3: Integration and Rehabilitation: This final phase focuses on integrating the self, improving daily life, and building a future without relying on dissociation. The goal is a unified sense of self and well-being.
This structured approach is vital for deep-seated healing. For more, see the ISSTD treatment guidelines.
2. Trauma-Focused Therapies (CBT, DBT, & EMDR)
Within the psychotherapy framework, these modalities provide concrete skills to manage symptoms and process trauma.
- Cognitive Behavioral Therapy (CBT): Helps identify and change negative thought patterns and behaviors linked to trauma, anxiety, and depression. It builds healthier coping strategies.
- Dialectical Behavior Therapy (DBT): Teaches crucial skills in mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness. It’s highly effective for managing intense emotions and reducing self-harm.
- Eye Movement Desensitization and Reprocessing (EMDR): A specialized therapy to reprocess “stuck” traumatic memories, reducing their emotional impact. It must be adapted by a trained clinician for dissociative disorders to be used safely, typically in Phase 2 of treatment.
3. Intensive Outpatient Programs (IOP)
When weekly therapy isn’t enough, but inpatient care is too much, Intensive Outpatient Programs (IOP) offer the perfect balance. IOPs provide structured, multi-day-a-week therapy while you continue to live at home and manage work or school.
At Thrive Mental Health, our IOPs offer:
- More than once-a-week therapy: Multiple hours of therapy several days a week for a higher level of support.
- Group therapy benefits: A sense of community that reduces isolation and validates your experiences.
- Individual counseling: Personalized one-on-one sessions to process individual issues.
- Flexible scheduling: Virtual and in-person IOPs across Florida, with evening options to fit your life.
- Skill-building workshops: Learn and practice vital coping skills in a supportive environment.
Our programs are ideal for stepping down from a higher level of care or for anyone needing more support than weekly sessions. Explore our Intensive Outpatient Programs.
4. Partial Hospitalization Programs (PHP)
For acute symptoms or crises that don’t require a 24/7 hospital stay, Partial Hospitalization Programs (PHP) provide the highest level of outpatient care. PHPs offer daily, intensive treatment for several hours a day, five days a week, serving as a direct alternative to inpatient care.
Our PHPs at Thrive Mental Health, available across Florida, are designed to provide:
- Daily structured treatment: A comprehensive schedule of individual and group therapy.
- Crisis stabilization: Immediate support and intervention to prevent hospitalization.
- Comprehensive skill-building: Intensive focus on coping mechanisms, emotional regulation, and relapse prevention.
- Integrated care: Collaboration between therapists and psychiatrists for a holistic approach.
PHPs are ideal for those with severe dissociative symptoms or co-occurring conditions who need a safe, structured environment for intensive healing. Learn more about our Partial Hospitalization Programs.
5. Medication Management for Related Symptoms
While no medication specifically treats dissociation, it’s crucial for managing co-occurring conditions like depression, anxiety, and mood instability. Addressing these symptoms with medication makes psychotherapy more effective. Under a psychiatrist’s guidance, common medications include:
- Antidepressants: To alleviate depression and anxiety, making trauma work more manageable.
- Mood Stabilizers: To even out emotional swings and reduce impulsivity.
- Atypical Antipsychotics: In low doses, may help manage severe dissociative symptoms or thought disorganization.
Medication management is always personalized and supports therapy—it does not replace it.
Which Recommended Mental Health Services Support Dissociative Disorders in Crisis?
Disclaimer: If you are thinking about hurting yourself or are in immediate danger, please call or text 988 in the U.S. to reach the Suicide & Crisis Lifeline. You are not alone.
When facing a mental health crisis with dissociative disorders, immediate, specialized support is critical. Knowing which recommended mental health services support dissociative disorders during these vulnerable times can be life-saving.

Why is safety the #1 priority in treatment?
Safety is the absolute foundation of treatment. Because these disorders are born from trauma, individuals often face significant risks:
- High risk of self-harm and suicide: More than 70% of people diagnosed with DID attempt suicide or engage in self-injury. This makes robust safety planning essential.
- Fugue states: Dissociative amnesia can lead to fugue states, where a person travels unexpectedly with no memory of it, putting them in vulnerable situations.
- Creating a crisis plan: Working with a therapist to create a plan with triggers, coping skills, and emergency contacts is a critical first step.
- Building coping skills: Learning grounding techniques and other skills helps manage distress and stay present.
- The role of a strong support system: A network of trusted friends, family, or support groups provides an essential layer of safety.
If you’re in crisis, call/text 988 right now. You are not alone.
Which recommended mental health services support dissociative disorders and prevent hospitalization?
While inpatient hospitalization is sometimes needed for safety, IOPs and PHPs are designed to provide intensive support that can prevent hospitalization or ease the transition home. Here’s how our programs achieve this:
- Daily structure and routine: The consistent schedule in IOPs and PHPs provides a stabilizing routine that anchors individuals to the present.
- Crisis management skills: Participants intensively learn and practice de-escalation techniques and how to use their support network.
- Peer support in group therapy: A therapeutic community reduces isolation and normalizes experiences, which is a powerful antidote to disconnection.
- Constant access to a clinical team: Consistent access to professional guidance allows for immediate intervention when needed.
- A safe environment for processing: The structured setting allows individuals to process intense emotions and trauma in a controlled, therapeutic manner.
By providing this intensive, structured care, our IOP and PHP programs in Florida empower individuals to manage symptoms, build resilience, and avoid more restrictive levels of care.
How to Access Treatment and Support a Loved One
Finding the right support for dissociative disorders can feel daunting, but effective treatment is within reach. Here’s how to access it for yourself or a loved one.
How do I find a qualified therapist and pay for treatment?
Finding a therapist trained in trauma and dissociative disorders is crucial. Here’s how to find the right professional and manage the cost:
-
Finding a trauma-informed specialist:
- Psychology Today directory: Search for therapists by specialization (e.g., “dissociative disorders,” “trauma,” “EMDR”), location, and insurance.
- ISSTD therapist finder: The International Society for the Study of Trauma and Dissociation (ISSTD) has a search feature for qualified professionals.
- Ask for referrals: Your primary care physician can often provide referrals.
-
Paying for care and verifying insurance benefits:
- Intensive programs like IOP and PHP are an investment, but many insurance plans provide significant coverage. Thrive Mental Health works with major providers like Cigna, Optum, and Florida Blue.
- We offer a quick, no-obligation insurance verification to clarify your benefits for our IOP/PHP programs in Florida, including locations in Miami and Orlando.
Finding the right clinical and financial fit is key to long-term recovery.
What resources are available for friends and family members?
Supporting a loved one with a dissociative disorder is challenging. Education and self-care are essential for caregivers to avoid burnout.
- Educate yourself: Understanding the disorder helps you provide empathetic support. NAMI offers excellent NAMI resources for families.
- Prioritize self-care: You can’t pour from an empty cup. Taking care of your own mental health by setting boundaries and seeking support is necessary, not selfish. There are 60 million unpaid caregivers in America; don’t forget your own needs.
- Find support organizations:
- The Sidran Institute offers resources on traumatic stress and dissociative disorders: Sidran Institute for traumatic stress.
- NAMI also provides support groups and educational programs for families.
You cannot pour from an empty cup. Taking care of yourself ensures you have the resilience to support your loved one effectively. For more insights on supporting family and friends, you might find this article helpful: Supporting a Loved One with Mental Health Challenges.
Frequently Asked Questions about Dissociative Disorder Treatment
Can you fully recover from a dissociative disorder?
Yes, recovery is absolutely possible, and many individuals with dissociative disorders lead fulfilling lives. “Recovery” typically focuses on achieving functional integration—where the individual develops a more cohesive sense of self, manages symptoms effectively, improves daily functioning, and builds healthy relationships. This may involve separate identity parts merging (fusion) or learning to cooperate harmoniously (resolution). The goal is to feel more whole and in control of your life, which may or may not mean a complete absence of all dissociative experiences, but rather a significant reduction in their disruptive impact.
How long does therapy for dissociative disorders take?
Treatment for dissociative disorders is generally long-term, often lasting several years, not weeks or months. This extended timeframe is necessary because these disorders are typically rooted in complex, early-life trauma. Healing requires building deep trust with a therapist, establishing safety, slowly processing traumatic memories, and integrating fragmented aspects of identity. It’s a marathon, not a sprint, and patience with the process is key for lasting change.
Is virtual therapy effective for dissociative disorders?
Yes, virtual therapy, particularly structured programs like our Virtual Therapy IOP and PHP at Thrive Mental Health, can be highly effective for dissociative disorders. The key is that the virtual program must be trauma-informed, provide consistent structure (individual and group therapy), and be led by clinicians experienced in treating dissociation. Virtual care can offer significant benefits, including increased accessibility, reduced travel time, and the comfort of receiving treatment from a familiar environment, which can be particularly helpful for individuals who struggle with external reality or social anxiety.
Your Path to Feeling Whole Again Starts Here
Understanding which recommended mental health services support dissociative disorders is the first step toward reclaiming your life. The journey from fragmentation to integration is challenging, but with the right structured, trauma-informed support, it is profoundly rewarding. Our integrated IOP and PHP models at Thrive Mental Health are designed to provide the clinical expertise, flexible scheduling, and compassionate care you need to heal. We believe in your capacity for recovery, and we’re here to guide you every step of the way, helping you move towards a future where you feel whole, connected, and truly yourself. You can learn more about our comprehensive remote mental health support: More info about remote mental health support.
Ready for support? Thrive offers virtual and hybrid IOP/PHP programs with evening options. Verify your insurance in 2 minutes (no obligation) → Start benefits check or call 561-203-6085. If you’re in crisis, call/text 988.